Treatment of hemophilia A in Brazil is offered to all patients at no cost. However, several unmet medical needs exist.
MethodIn this study, we applied the Delphi method to discuss with seven hemophilia A specialists the challenges that patients and the health system face regarding hemophilia A treatment and opportunities for improvement.
ResultsA consensus was obtained regarding the number of weekly infusions and patient adherence to treatment. The bleeding profile, unfavourable pharmacokinetics (PKs), low adherence and high daily activity were patient profiles that would benefit from using the extended half-life (EHL) recombinant factor VIII (rFVIII). The advantages of treatment with the EHL rFVIII were the lower number of infusions per week, which could increase patient adherence and decrease the risk of bleeds, due to a more constant plasma level, a lower value. Additionally, the EHL rFVIII could improve quality of life, especially in patients with high daily activity, such as adolescents and young adults. The panelists mentioned that EHL rFVIII, if available, could be offered first to the priority group (adolescents between 12 and 19 years old), followed by adults (20 to 64 years old) and elderly people (over 65 years old).
ConclusionIn summary, the EHL rFVIII offers the optimal prophylaxis by decreasing the dose frequency, increasing the treatment adherence and improving the QoL, without compromising safety and efficacy.
Hemophilia A is an inherited bleeding disorder caused by abnormalities on coagulation factor VIII and, currently, no curative treatment is available.1 Repeated bleeds into joints and muscles result in pain and incapacity and may cause severe arthropathy and deformities in the long-term, with associated muscle wasting.1
Current treatment consists of factor VIII replacement and one of the most difficult problems is that, frequently, patients develop the inhibitory antibody anti-factor VIII (also called inhibitors).2 In addition, the hemophilia A treatment requires frequent self-infusions (three or more times per week), that often come with pain and discomfort, as well as daily life limitations, depression and anxiety.3,4
According to the World Federation of Hemophilia, factor VIII replacement should consider the frequency of the bleedings and individual pharmacokinetics (PK), as well as patient history and preferences.2 The treatment can be offered in two different therapeutical plans: a) prophylaxis, consisting of the regular administration of therapeutic products and b) on demand, in which the therapy is offered in the presence of a bleeding episode.2 The Medical and Scientific Advisory Council Guidelines established prophylaxis as the gold standard treatment for hemophilia A.5
For hemophilia A replacement therapy, we have available concentrates derived from human plasma (pdFVIII) and the recombinant factor VIII (rFVIII). Recombinant factor VIII (rFVIII) products are manufactured in buffered human serum albumin (HSA; first-generation products) or without HAS, but containing sucrose as the main stabilizer (second-generation products).6,7 Currently, there are third-generation rFVIII products, with no animal or human proteins other than FVIII added during the manufactured process until the final formulation. These products may have standard half-life (SHL) or extended half-life (EHL), with the latter being potentially able to maintain proper factor VIII levels for longer periods, resulting in a higher trough level and, consequently, in more effective protection against bleedings with less frequent infusions.6
The SHL rFVIII concentrates are administered intravenously and used at least three times a week (under prophylaxis), which makes it difficult for the patient to adhere to the treatment, and negatively impacts the Quality of Life (QoL).8–10 Studies show that the lack of time, schedule inconveniences for treatment and social and psychological distress are factors that influence adherence.11,12 Therefore, the burden of hemophilia A treatment is high and adherence to treatment, especially in adolescents and young adults, appears to be suboptimal as, in these periods of life, the responsibility for the treatment is transferred from parents to patients, who often see the self-infusions as impediments to daily activities.13
In Brazil, the prophylaxis treatment is offered by the Unified Health System (SUS) to all patients at no cost and with a SHL rFVIII (although a small proportion of patients still receive pdFVIII). Despite the full access to hemophilia treatment, in the past years there has been no incorporation of new technologies by the hemophilia program in the Brazilian Public National Health System (the Sistema Único de Saúde – SUS). Therefore, several unmet medical needs still exist. In this context, this study used a modified Delphi Panel, aiming to get the understanding and consensus of unmet medical needs, treatment patterns, frequency of infusions, dose and the role of the EHL rFVIII in the treatment of hemophilia A patients in Brazil, from the perspective of the SUS.
Materials and methodsDelphi methodRecognized as highly cooperative and effective,14 a consensus-based approach, was carried out applying a modified Delphi technique, which took place between July and September 2020. The Delphi technique is a methodology that seeks to reach consensus on the opinions of a group of respondents, who are specialists on a topic, through a series of structured questionnaires.15,16
Three rounds were performed for this Delphi Panel.
A structured questionnaire was applied for each participant individually and anonymously. Answers return to the interviewees in a summarized form, called feedback. The feedback was provided by a new questionnaire that was adjusted considering the answers received by each round. Subsequently, participants could see the group's answers in the previous round.17,18 The third and final round is a face-to-face meeting,19 that allows interaction between the panelists, to discuss and give further information to sustain their opinions.20
In the first and second rounds, participants answered an online questionnaire on the MS Forms® platform. In the third round, the participants answered questions and discussed them on an in-person group web meeting. The consensus was considered when at least 6 of the 7 participants agreed on the same response (majority).
Panelist recruitmentAiming to get geographic representativeness of the whole country and reduce bias, seven physicians specialized in hemophilia A who work with patients in the SUS were selected from different states and cities, such as São Paulo, Espírito Santo, Pará and Paraná. The invitation was sent by email and a phone call was made to explain all the steps of the Delphi panel.
Literature review and questionnaire developmentTo develop the questionnaire, a literature search was performed to identify treatment patterns, frequency of infusions, dose and the use of the EHL rFVIII to address unmet medical needs regarding hemophilia A in Brazil. The search was carried out within bibliographic and gray literature databases, that included MEDLINE, ISPOR Scientific Presentations Database and LILACS BVS. Additionally, Brazilian Guidelines of Hemophilia were used.6 The search strategy combined keywords for “hemophilia”, “treatment”, “unmet needs”, “SHL rFVIII”, “EHL rFVIII” for English and Portuguese literature.
Based on the literature review findings regarding the hemophilia A treatment, the questionnaire was divided into three parts: unmet medical needs and treatment adherence (challenges and possible improvements in the SUS); frequency of infusions and dose of the current treatment in the SUS, and; if the EHL rFVIII could address the identified unmet needs in the treatment of hemophilia A patients in Brazil.
Round 1The first-round questionnaire was circulated by email to all 7 panelists, who had one week, from July 17 to 23, 2020, to respond. The first questionnaire prioritized open questions, utilizing an exploratory approach to avoid bias and the restriction of topics to be addressed in subsequent rounds. After the first round, the responses were compiled and analyzed.
Round 2Based on the round 1 answer analysis, a feedback was provided to the panelist. The feedback consisted of an adjusted questionnaire by the first-round answers. From August 20 to 26, 2020, the panelists answered the second-round questionnaire, also sent by email. After the second round, the answers were analyzed and compiled for the final discussion.
Round 3To obtain a consensus on the topics still open and validate those already obtained from the first two rounds, a face-to-face online meeting was performed. Based on the round 2 answer analysis, a questionnaire adjusted by the second-round answers was used as a discussion guide.
ResultsThe Delphi Panel identified unmet medical needs, treatment adherence challenges and possible aspects for improvement in the SUS, frequency of infusions and dose of the current treatment used in the SUS and how the EHL rFVIII could address the identified unmet needs in the treatment of hemophilia A patients in Brazil.
ParticipantsPhysicians specialized in hemophilia A were invited to participate in the study. All participated in the first and second rounds, however, six panelists were able to participate in the third round through a videoconference.
Unmet medical needs and treatment adherenceThe panelists obtained consensus about the unmet needs for the current treatment provided by the Brazilian public healthcare, which were:
- •
The SHL rFVIII requires several weekly infusions with protection throughout the day, depending on the time of administration.
- •
The PK characteristics of the SHL rFVIII available in the SUS could increase the risk of bleeding in moments of low plasma level.
- •
Intravenous treatment may impact patient adherence.
- •
The clinical condition of patients who do not adhere may worsen, due to the high frequency of infusions, requiring more frequent consultations, physiotherapy sessions, and other procedures, generating problems of self-esteem, absenteeism at school and work.
The panelists provided detailed comments to explain their responses:
“We do not have problems getting access to the recombinant factor VIII for the hemophilia A treatment. However, we should include other technologies, such as the EHL rFVIII”.
“Access to the recombinant factor is not a problem, but the access to new technologies is … there is a gap in the incorporation of new technologies by the hemophilia program in the SUS”.
The panelists evaluated the concept of treatment adherence as “low”, “moderate” and “high” adherence to the treatment of hemophilia, based on the percentage of the prescribed therapeutical plans and administrated infusions. Low adherence was defined by 3 out of 6 as the range between 40 to 50%, while the other 3 participants, said that low adherence is 50 to 60% of infusions administered as prescribed. As a result of the expert opinion, an average of 53% was estimated as low adherence.
Moderate adherence had an average of 69% of the infusions administered as prescribed. No consensus was established, as 3 out of 6 mentioned a range between 60 and 70%, while the other 3 participants said that moderate adherence is 70% of the infusions administered as prescribed. The consensus was achieved for the definition of high adherence. Panelists had agreed that 90% of the administered infusions as prescribed is the best way to define high adherence.
“I believe that 90% is accurate to define high adherence because it is impossible to expect 100% of the infusions administered as prescribed; there are some specific situations that we should not consider as a lack of adherence”.
Regarding patient characteristics that could influence treatment adherence, consensus was obtained for:
- •
Difficulties to intravenous access.
- •
Teenagers have difficulties to adhere, due to age-related behavior and the transition from the care provided by parents to self-care.
- •
The disbelief of treatment efficacy and lack of knowledge on how the treatment is important could influence adherence.
- •
Workload and high daily activities influence treatment adherence in adolescents and adults.
Most panelists commented on the lack of knowledge and time needed to manage the weekly number of infusions.
“The more aware of treatment benefits, the more patients understand the consequences of an inadequate treatment”.
“Some patients discontinue treatment due to the long time spent on infusions”.
“Adults and adolescents have difficulties in organizing daily activities and infusions”.
Social and economic factors, such as income and education, could facilitate or disturb treatment adherence. Four of six panelists mentioned that low-income people could have difficulties in following the treatment, however, 2 of the 6 panelists said that high-income people could show less engagement to treatment too.
“For instance, in my State, patients do not have free public transportation and, for that reason, some patients do not return to the clinic in the adequate period”.
“Sometimes, high-income patients are less compliant than low-income patients”.
“Undoubtedly, low income may hinder the treatment adherence, but it is not a determinant factor, a different and individualized approach is required”.
Problems related to the multidisciplinary team were not a consensus among the panelists. Three of six mentioned that a multidisciplinary team is necessary and also that they must frequently manage team replacements and training due to a high turnover. “Especially in a team that has a very high turnover, there is a lack of motivation in some professionals”.
Although there was no consensus on problems with multidisciplinary teams, the responses show that the panelists agreed that these are inherent to the needs and individual characteristics of each State.
“Problems related to the multidisciplinary teams are very individualized to each team and each State”.
“It is not possible to establish consensus on items that have local variations or certain specificities. Problems related to the multidisciplinary team occur, but it is not a consensus because it does not occur everywhere”.
The last question about unmet needs and treatment adherence aimed to identify the percentage of patients requiring greater coagulation factor protection. The panelists agreed that 40 to 50% of the total number of hemophilia patients in Brazil require a better option of care.
Frequency of infusions and doseParticipants obtained a consensus on the average dose of SHL rFVIII currently available in the SUS for primary and secondary prophylaxis, mentioning 25 to 29 international units per kilogram (IU/Kg) for both situations. However, as the tertiary prophylaxis treatment requires a higher individualized approach, no consensus was found. Four of 6 panelists mentioned that the tertiary prophylaxis dose of SHL rFVIII should be 15 to 20 IU/Kg and two said that the average dose of SHL rFVIII used in tertiary prophylaxis treatment must be 20 to 25 IU/Kg.
“We use PK to guide what amount of SHL rFVIII should be prescribed, the dose is individualized, however, the average is 15 to 20 IU/Kg”.
Treatment on demand depends on the bleeding episode and the average dose of SHL rFVIII mentioned was 25 to 29 IU/Kg.
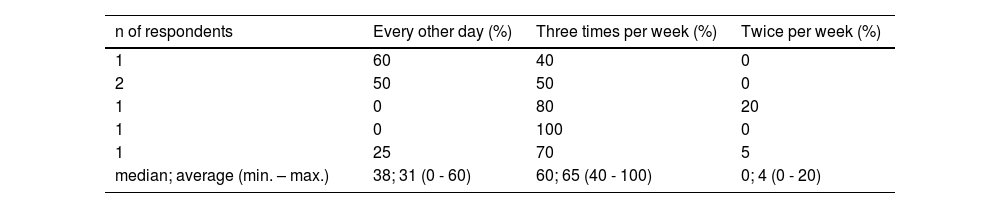
Raised as the most common patient profile, the Delphi panel explored the therapeutical plan of the secondary prophylaxis treatment. Table 1 shows the percentage of patients by the therapeutical plan of the SHL rFVIII.
Based on the distribution shown in Table 2, the median percentage of patients that use the every-other-day SHL rFVIII therapeutical plan was 38% (average 65, 40 - 100), 60% (average 65, 40 - 100) use three times per week and 0% (average 4, 0 - 20) use twice per week.
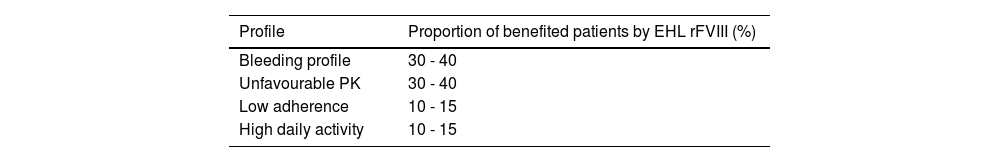
Percentage of patients by profile benefited by EHL rFVIII.
| Profile | Proportion of benefited patients by EHL rFVIII (%) |
|---|---|
| Bleeding profile | 30 - 40 |
| Unfavourable PK | 30 - 40 |
| Low adherence | 10 - 15 |
| High daily activity | 10 - 15 |
PK: pharmacokinetics; EHL: Extended half-life; rFVIII: recombinant factor VIII.
Pharmacokinetics, presence of target joint, bleeding profile and clinical response were mentioned as the key factors that motivate the decision-making as to the dose adjustment. The management of prophylactic treatment was performed considering two proposals: the adjustment of the amount of IU/Kg and dose, followed by the infusion frequency adjustment.
Addressing unmet needs with EHL rFVIIIThe panelists answered how the EHL rFVIII could address the unmet medical needs raised during the Delphi panel. The bleeding profile, unfavourable PK, low adherence and high daily activity were a consensus of patient profiles that would be benefited from using the EHL rFVIII. The proportion of patients benefited with the use of EHL rFVIII by profile is shown in Table 2. Regarding all patient characteristics, the panelists stated that 30 to 40% of the hemophilia A population over 12 years old could be benefited from the use of the EHL rFVIII.
The advantages of EHL rFVIII treatments, mentioned by all the panelists, are related to the lower number of infusions per week, which could increase patient adherence and may decrease the risk of bleeding, due to a more constant plasma level and a higher trough level. Additionally, the panelists agreed that the EHL rFVIII could improve the QoL, especially in patients with high daily activity, such as adolescents and young adults.
The panelists pointed out that, if the EHL rFVIII treatment is available for use in the SUS, the group having priority in receiving the treatment would be adolescents (aged between 12 and 19 years old), followed by adults (20 to 64 years old) and elderly people (over 65 years old).
DiscussionThis study aimed to discuss with experts in hemophilia treatment in Brazil, the unmet medical needs, treatment patterns, frequency of infusions, dose and role of the EHL rFVIII in the treatment of hemophilia A, in light of the treatment currently available in the SUS.
The Brazilian public healthcare provides SHL rFVIII, although a small proportion of patients still receive pdFVIII. The treatment with SHL rFVIII requires several weekly infusions due to the lower half-life, depending on the therapeutical plan, compared to the EHL rFVIII. The PK characteristics of the SHL rFVIII can potentially increase the risk of bleeding in moments with a lower plasma level.21 Moreover, intravenous treatment with morning infusions is time-consuming and may impact patient adherence, in particular for adolescents and young adults, as they tend to focus on their daily activities.13
Patients with poor treatment adherence due to the high frequency of infusions may worsen their clinical condition, presenting more bleeds, requiring more frequent consultations, physiotherapy sessions and other procedures, generating problems of self-esteem and absenteeism at school and work.13 In this sense, new treatment options are needed to ensure treatment adherence and mitigate the burden of disease.
Aiming to understand the differences between guideline recommendations and real-world clinical practice, the panelists answered questions about the frequency of infusions and doses used to treat hemophilia patients in Brazil. Pharmacokinetics, the presence of target joint, bleeding profile and clinical response were mentioned as the key factors motivating the treatment decision-making adjustment. The management of the prophylaxis treatment was performed considering two proposals: the increase of the IU/Kg dose, followed by the increase of infusions frequency and dose.
The panelists argued that the advantages of EHL rFVIII treatments are related to the lower number of infusions per week. The panelists pointed out that if they had EHL rFVIII available to use in the SUS, the group having priority to receive the treatment would be adolescents aged between 12 and 19 years old, followed by adults (20 to 64 years old), the last group being formed by elderly people (over 65 years old).
The use of an EHL rFVIII may decrease the burden of treatment, as demonstrated in several clinical trials.22–25 In the PROTECT study, 67.3% of the patients who received damoctocog alfa pegol, an EHL rFVIII, were effectively treated with extended intervals of every five or seven days, with no safety concerns and low rates of bleeds.23 The advantages of EHL rFVIII treatments, as mentioned by the experts participating in our study, are related to the lower number of infusions per week, which could increase patient adherence and, consequently, decrease the risk of bleeds due to a more constant plasma level and a higher trough level.
In conclusion, through the expert consensus, the treatment of hemophilia A in Brazil could be improved with the EHL rFVIII treatment. However, the results demonstrated by this study should be interpreted considering important limitations. Brazil is a large country composed of 27 federative units, this study might not represent the opinion of hemophilia A experts in the whole country, because the panelists in the Delphi panel were from four different states. The Delphi aimed to assess the value of the EHL rFVIII, but did not evaluate other treatments, such as those using the monoclonal antibody and gene therapy. Still, the consensus obtained in this study corroborates with the literature on the unmet medical needs and how they could be addressed.
ConclusionThe consensus was obtained regarding the fact that the unmet needs in the treatment of hemophilia A still exist, despite treatment with a rFVIII offered in the SUS. As expected, the high frequency of infusions and how it affects daily life and, consequently, the QoL of the patients appear as an important unmet need that requires being addressed to increase treatment adherence.
The panel of experts also obtained consensus about how the EHL rFVIII could potentially address the unmet needs regarding adolescents and young adults, who are people with a high daily activity and, consequently, a lower adherence to treatment and therefore, at a higher risk of presenting bleeds. The EHL rFVIII appeared as products offering optimal prophylaxis that could help patients with a bleeding profile, unfavourable PK, low adherence and high daily activity by decreasing the dose frequency, increasing the treatment adherence and improving the QoL without compromising safety and efficacy.
Author contributionsRP provided methodological advice and supervised the study. APAB wrote the first draft of the manuscript. All authors discussed and agreed with the content of the final version of the manuscript.
This study was funded by Bayer S.A.