Immune thrombocytopenia (ITP) is an acquired bleeding disorder observed in the clinical practice. Little is known about its epidemiology in Brazil. The present study was conducted at a hematology referral center which covers a population of over 8 million in 184 municipalities in the state of Ceará. The purpose of this study was to draw a demographic profile of adult ITP patients with regard to sex, age, geographical origin and distribution across the state, and the proportion of secondary ITP. Following ethics committee approval, information was collected with an ad hoc instrument. The sample consisted of 187 adult ITP patients attending the Walter Cantídio University Hospital in 2015. The median follow-up time was 67 months (range: 1 month to 29 years). Female sex (n = 154; 82.35 %) was strongly prevalent in all age brackets, with an overall female/male ratio of 4.7:1. The median age was 41 ± 16.1 with an interquartile range of 29–55.5 years; there was no difference between the genders. Secondary ITP (18/187; 9.6 %) displayed a bimodal distribution and a linear increase between 38 and >68 years of age. The results of this survey on the epidemiology of ITP in Brazil suggest that ethnic and geographical factors may have a great impact on age and sex distribution and on the distribution of secondary ITP.
Immune thrombocytopenia (ITP) is an acquired autoimmune bleeding disorder mediated by platelet autoantibodies inducing platelet destruction and inhibiting platelet production, leading to isolated (and in some cases life-threatening) thrombocytopenia with mucocutaneous hemorrhage. ITP has been described as a rare disease, but recent epidemiological data suggest otherwise.1,2 Though insufficiently explored, this new evidence provides interesting insights into the characteristics of ITP.
Estimates of the burden of ITP are based on reported incidences and prevalences. The disorder affects adults at a rate of 1.6–3.9 per 100,000 person-years.3–6 The first reports, published between 1999 and 2009, are retrospective European studies based on databases and registries.
According to a critical review published by Terrell et al. (2010),7 the most reliable estimate of the incidence of ITP is that of Frederiksen & Schmidt3 (2.68 per 100,000 person-years). The authors carefully validated cases by chart review and included patients with platelet counts below 100 × 109/L or below 50 × 109/L, as the case might be.
In another recent study, Weycker et al.8 reported the annual incidence of ITP in the US to be 6.1 per 100,000 of the population, with different rates for females (6.7), males (5.5), children aged 0–4 years (8.1) and adults aged ≥65 years (13.7). These findings suggest that nearly 20,000 children and adults are diagnosed with ITP every year in the US, a substantially higher number than previously reckoned.
ITP has a preference for young women, but recent investigations have shown the condition to be fairly common in both sexes and at all ages.3,9,10 Due to the persistence of symptoms for over 12 months,11 ITP is defined as a chronic disease. This is supported by a range of studies on adult ITP patients,6,10,12,13 with some cases of recurrence having been reported.
The epidemiology of ITP has been investigated in some countries, such as in the UK, France, the US, Japan and Korea,5,6,8,12,14,15 but no epidemiological studies have, to our knowledge, been conducted in Brazil. To fill this gap, we evaluated the epidemiology of ITP based on a series of patients attending a hematology referral center in Northeastern Brazil.
ObjectiveThe purpose of this study was to draw a demographic profile of adult ITP patients with regard to sex, age, geographical origin and distribution across the state, and the proportion of secondary ITP.
MethodsThis was a descriptive, retrospective and quantitative case series study involving adult ITP patients (≥18 years) attending a hematology service in Fortaleza, capital of the State of Ceará. The service, run by the Walter Cantídio University Hospital (HUWC, Federal University of Ceará), serves as a referral center for the state's 184 municipalities, totaling over 8 million inhabitants (2010). Two previous studies about ITP have been produced in the same region.16,17 Inaugurated in 1959, the HUWC is a public hospital with a long history as a referral center for diagnosis and treatment of disease, organ transplantation and health education/training for medical students of the Federal University of Ceará.
SampleTrained researchers using an instrument designed for the purpose collected the demographic information used in this analysis. All adult ITP patients (≥18 years at the time of diagnosis) attending the hematology service in 2015 were included in the analysis (n = 187). Some patients had been followed for several years (in one case, since 1986), others were recently diagnosed (with confirmation of the diagnosis in 2015). There was data from 2016 concerning the follow-up evaluation of the treatment of some patients. The patients’ records were reviewed to validate the diagnosis of ITP, adopting as criterion a platelet count of <100 × 109/L in the absence of other causes of thrombocytopenia.
MetricsITP was defined according to the recommendations of the International Working Group (IWG).11 Primary ITP was characterized by isolated thrombocytopenia (peripheral blood platelet count <100 × 109/L) in the absence of other causes or disorders associated with thrombocytopenia. Primary ITP was diagnosed by exclusion, while secondary ITP was defined as any form of immune-mediated thrombocytopenia, except primary ITP.
In addition to the demographic variables, the analysis included blood counts, bleeding manifestations, laboratory findings (e.g. human immunodeficiency virus, hepatitis C, bone marrow aspiration) and therapies.
Statistical analysisThe collected data were analyzed with the JAMOVI v. 1.2.2.4 and Microsoft Excel 365 computer programs and organized in graphs showing age and sex distribution, geographic origin, and secondary ITP distribution.
Numerical variables are expressed as medians ± standard deviation, while categorical variables are expressed as frequency and, when appropriate, prevalence. The epidemiological maps were constructed using Microsoft Excel and the Microsoft Bing platform.
Ethical aspectsThe study protocol was approved by the research ethics committee at HUWC (Federal University of Ceará) and filed under #1.640.335.
ResultsThe medical records of the 187 adult ITP patients attending the hematology service in 2015 yielded the following results:
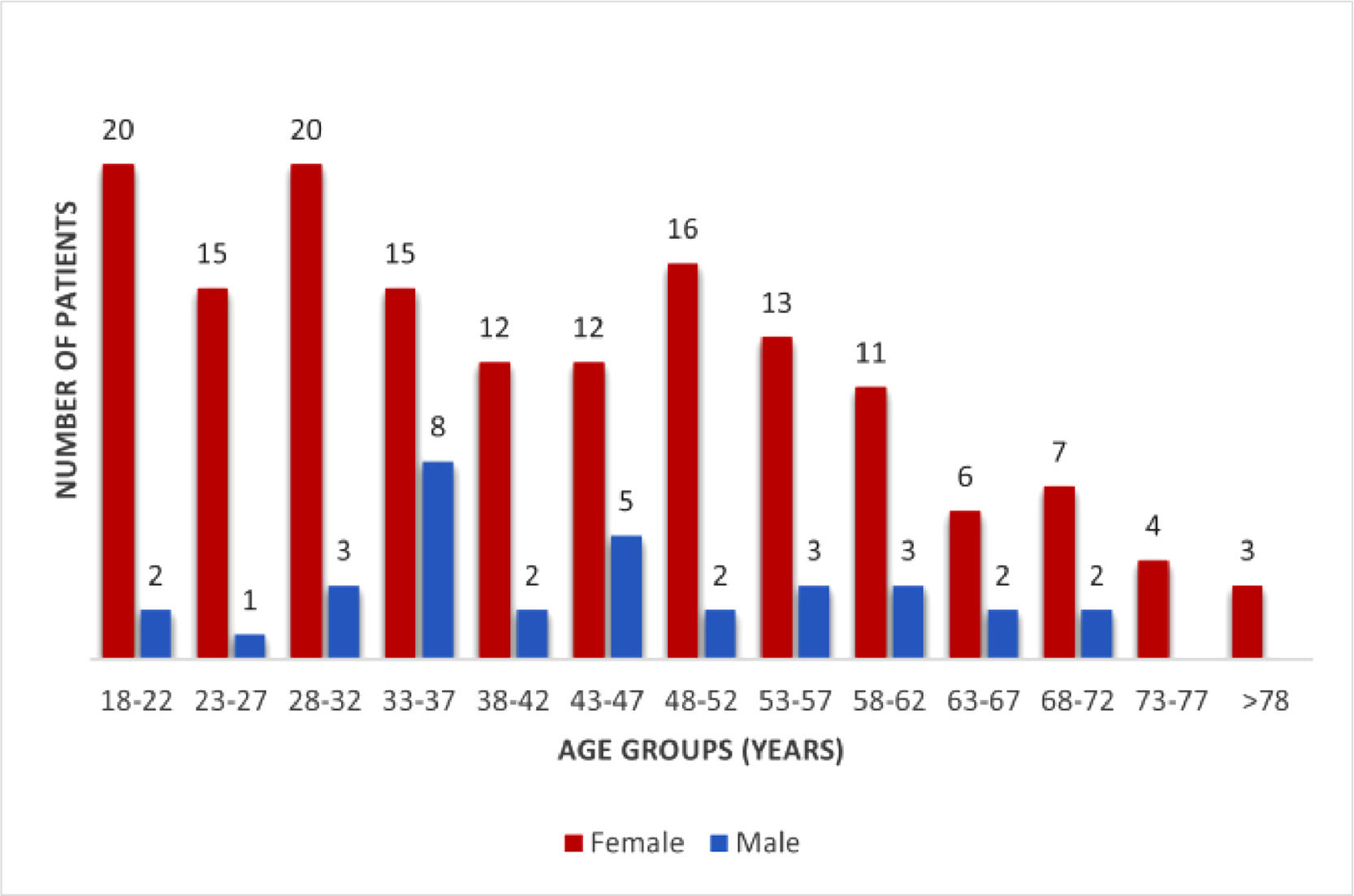
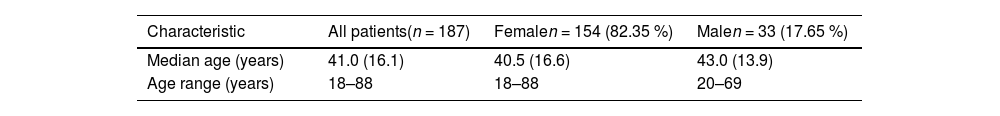
The median follow-up, that is time from the first consultation, was 67 months (range: 1 month to 29 years). The median age was 41 ± 16.1 years old with an interquartile range of 29–55.5 years, with no difference between the genders. Table 1 the female sex (82.35 %) was highly predominant in all age brackets, with an overall mean female/male ratio of 4.7:1 (Figures 1 and 2).
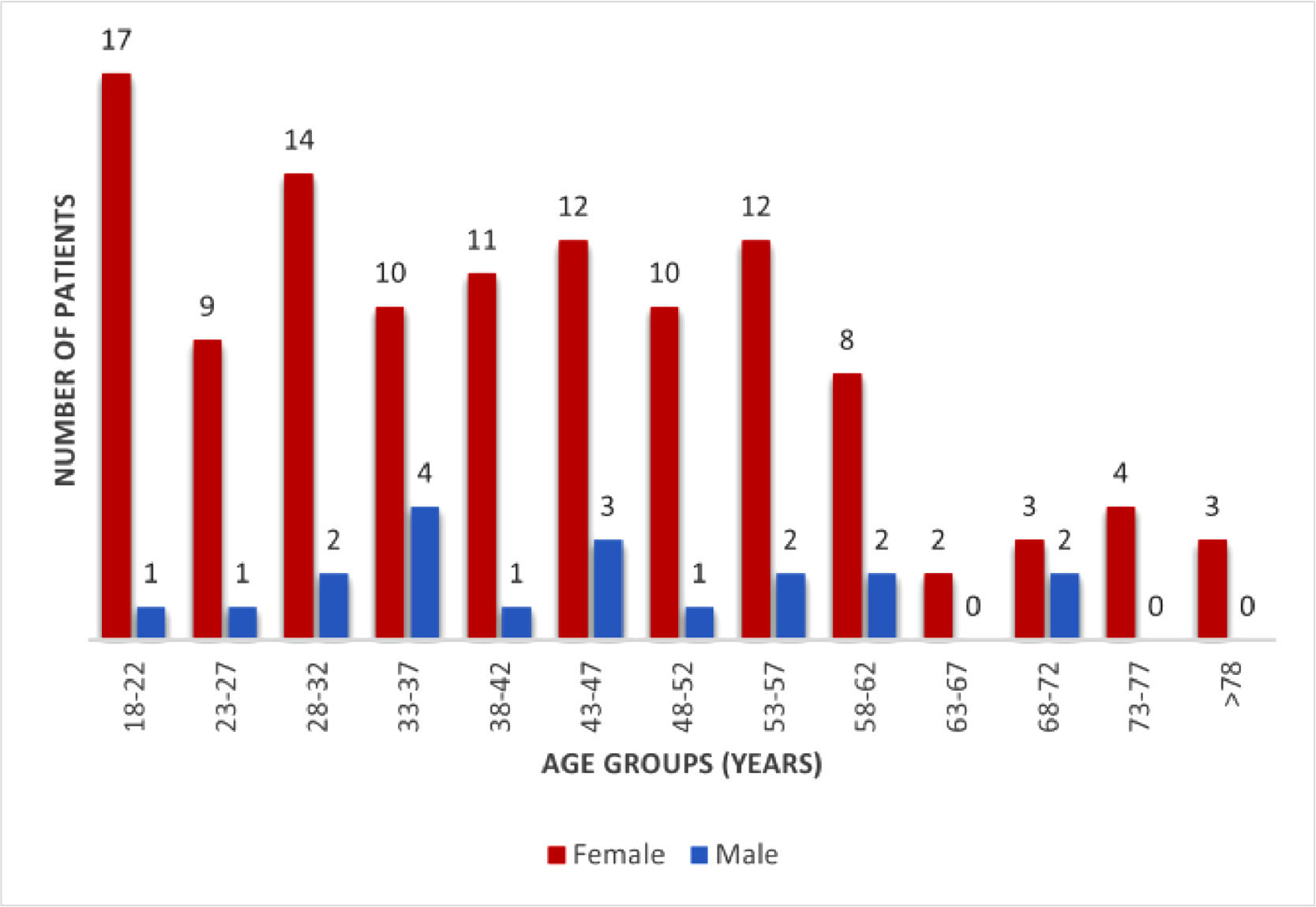
Due to the retrospective nature of the study, the variable “age at first symptoms <365 days before the first consultation” was only available for 134 patients. There was a delay between the first symptoms and first consultation of more the 365 days for the rest of the studied population (n = 53). These cases were excluded from the analysis shown in Figure 2, given that the first symptoms are more difficult to specify.
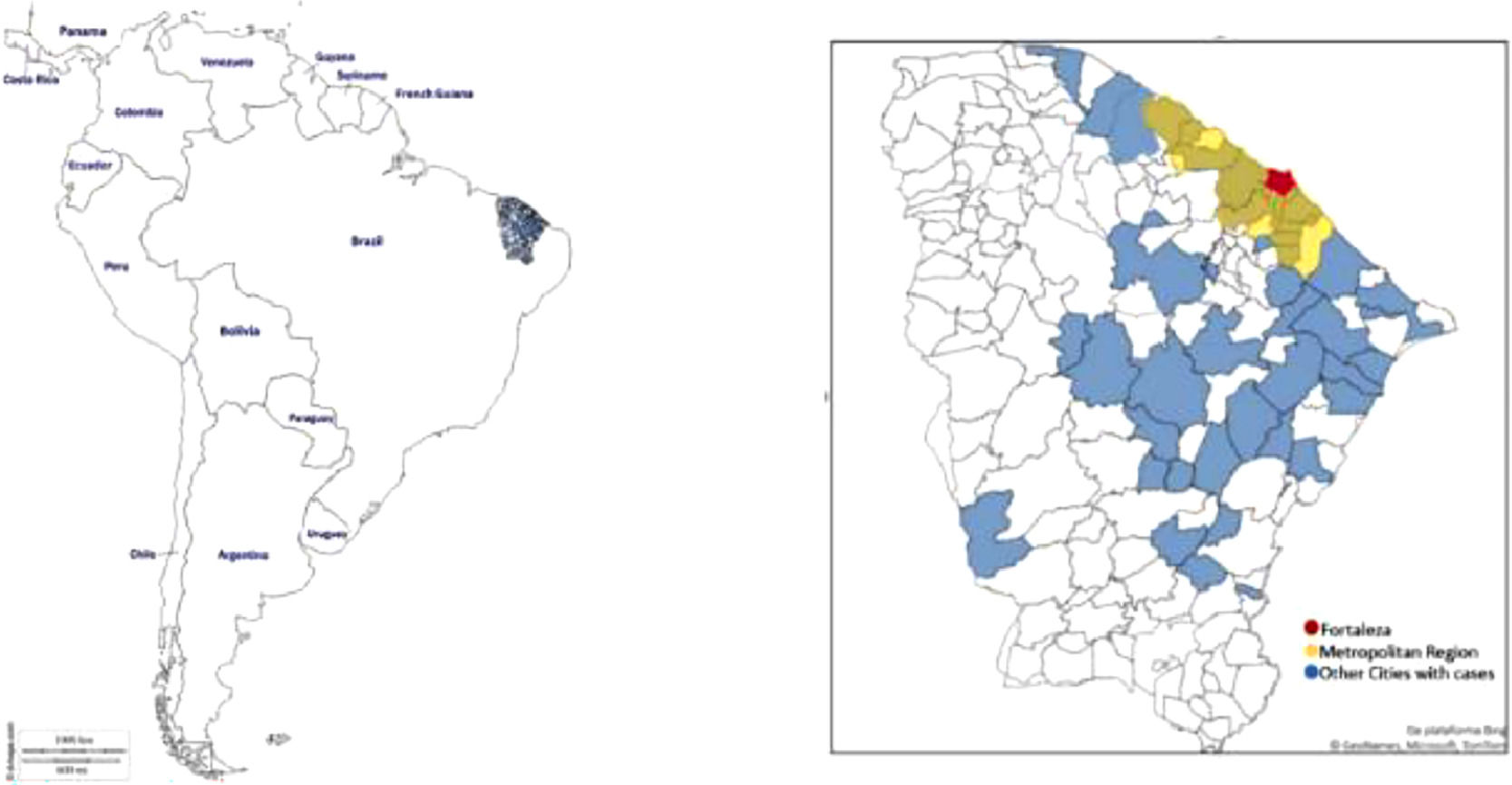
Most patients were residents of Fortaleza (n = 99; 52.94 %), followed by the metropolitan region (n = 48; 25.67 %) and towns in the countryside (n = 40; 21.39 %).
Bone marrow aspiration was performed in 157 patients (83.95 %) to exclude differential diagnoses, such as myelodysplasia. Of the over 60-year-old patients, approximately 81.8 % had been submitted to a bone marrow aspiration. Other causes or disorders that might have been associated with isolated non-immune thrombocytopenia were excluded: vitamin B12 deficiency (by vitamin B12 blood test level), pseudothrombocytopenia (by platelet count with anticoagulant citrate solution and peripheral blood smear analysis) and thrombotic thrombocytopenic purpura (by peripheral blood smear analysis and ADAMTS13 activity assay).
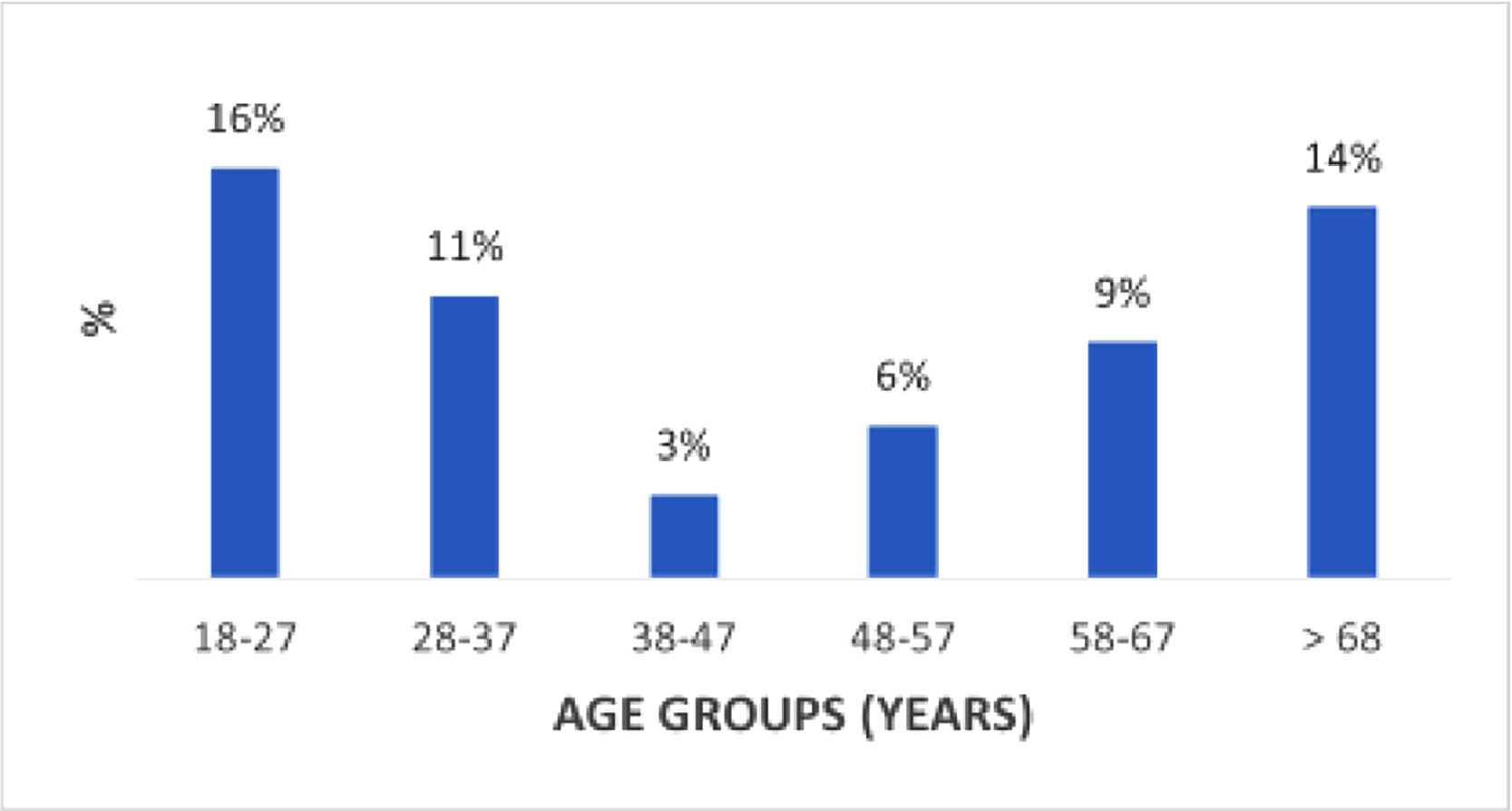
Nearly one tenth (18/187; 9.6 %) of the patients were diagnosed with secondary ITP. The associated underlying disorders were systemic lupus erythematosus (SLE - n = 5), antiphospholipid syndrome (APS - n = 5), Helicobacter pylori infection (n = 2), chronic lymphocytic leukemia (n = 1), hepatitis C virus infection (n = 1), autoimmune hepatitis (n = 1) and follicular lymphoma (n = 1). One patient had SLE associated with APS and Sjögren syndrome, and one patient was suspected of drug-induced ITP associated with thioridazine hydrochloride (Melleril®).
The frequency distribution of secondary ITP displayed two peaks, one for young adults (18–27 years) and one for seniors (>68 years) (Figure 4). The figure also shows a linear increase in frequency between 38 and >68 years of age.
DiscussionIn this descriptive retrospective case series study, we analyzed the medical records of 187 adult (≥18 years) ITP patients attending the hematology service in 2015. The median age was 41 ± 16.1 with an interquartile range of 29–55.5 years; there was no difference between the genders. The female sex (82.35 %) was highly predominant in all age brackets with the overall female/male ratio being 4.7:1.
Although ITP has been studied for over a century,18 its epidemiology is not well known for countries like Brazil. In fact, no data on the epidemiology of ITP in Brazil is available as according to the March 2019 report issued by the National Commission for the Incorporation of Technology into the Brazilian National Health Service (CONITEC),19 the incidence and prevalence of ITP in the Brazilian population have not yet been estimated.
By conducting this study at a hematology referral center, it was possible to estimate the burden of ITP and draw an epidemiological profile for the state (Figures 3.1 and 3.2). Ceará has a mixed urban, suburban and rural population, characterized by considerable ethnic and socioeconomic diversity.
The predominance of females observed in this study (154/187; 82.35 %) in all age brackets was expected (Figures 1 and 2) with similar findings being reported by studies on ITP incidence in a range of other countries. For example, Abrahamson et al.4 and Schoonen et al.5 observed that the overall mean incidence of ITP was significantly higher in women. The former studied 840 adult patients and found an incidence of 4.5/100,000 person-years (95 % confidence interval [CI]: 4.2–4.9) for women and 3.2/100,000 person-years (95 % CI: 2.8–3.5) for men. The latter reported compatible figures for a sample of 1145 ITP patients. In a prospective UK population cohort study involving 245 cases, Neylon et al.9 found only a slight difference between the sexes (134 vs. 111; female/male ratio - 1.2:1). A Korean study by Lee et al.15 including ITP patients of all ages also found ITP to be more common in women (female/male ratio - 1.3:1; 95 % CI: 1.2–1.4). According to the authors, the incidence was gender-specific among patients aged from 20 to 59.
Likewise, a study from Maryland, USA, by Segal & Powe20 showed a predominance of females in the middle-adult years, and an overall female/male ratio of 1.9:1. Bennett et al.21 also observed ITP to be more prevalent in women, with a tendency to increase with age and over time. The observed increase in prevalence may be, in part, the result of greater awareness among physicians, more efficient diagnostic tools and the advent of new therapies. On the other hand, the tendency to increase over time suggested to the authors that ITP in adults is essentially a chronic disease that may persist indefinitely.
The available epidemiological data confirm the observed female predominance. On behalf of the Intercontinental Cooperative ITP Study Group, Kühne et al.22 evaluated 340 adults (≥ 16 years) of whom 230 (68 %) were women. In 2016, Grimaldi-Bensouda et al.12 conducted a prospective observational cohort study evaluating 143 adult patients recently diagnosed with ITP recruited from 21 centers across France. Women accounted for 63 % and the median age was 50 years.
In the current case series, the median age was 41 ± 16.1 with an interquartile range of 29–55.5 years (range: 18–88) with no significant difference between the genders. In comparison to other studies, the median age in this study was lower than those described by Frederiksen & Schmidt3 (median: 56.4 years), Abrahamson et al.4 (median: 59 years), Neylon et al.9 (median: 56 years) and Segal & Powe20 (median: 49 years).
Based on the distribution of age at first consultation and gender of the 187 ITP patients (Figure 1), and the distribution of age at first symptoms and gender of the 134 patients diagnosed with a first lifetime episode (Figure 2), more ITP cases were observed in early and middle adulthood thereby matching the conclusions of Grimaldi-Bensouda et al.12
In contrast, several authors have concluded that the incidence of ITP increases with age. Frederiksen & Schmidt3 were the first to report growing incidences after 60 years of age with similar results having been published in other countries by Neylon et al.9, Abrahamson et al.4, Schoonen et al.5, Moulis et al.6, Weycker et al.8, Kurata et al.14 and Hung et al.23
In this study, secondary ITP accounted for 9.6 % of the 187 adult cases. This figure is slightly higher than that of Schoonen et al.5 (8.7 %), but considerably lower than the incidences reported by Cines et al.24 (20 %) and Moulis et al.6 (18 %). In the latter study, secondary ITP was more frequent in adults. Moreover, Hung et al.23 found the rate of secondary ITP to be significantly lower in children than in adults (4.2 % vs. 23.8 %).
Although there might be a bias concerning the difference between primary and secondary ITP, since this research was realized in a hematology service, a lower incidence of secondary ITP was also described in studies using databases based on administrative registers5,6 and clinical experience of authors.24 Those findings suggest that, regardless of the data source, the population of secondary ITP seems to be lower than primary ITP.
As shown in Figure 4, the frequency of adult secondary ITP displayed a bimodal pattern: one peak for young adults (18–27 years) and another peak for older adults (>68 years). Figure 4 also suggests an almost linear increase with age, starting at 38 years. A similar trend for secondary ITP was reported by Moulis et al.6
In view of the predominance of the female sex in this and other studies and the autoimmune nature of the disease, it is important to analyze the relationship between ITP, autoimmunity and female sex. Reviewing the main mechanisms responsible for increased immune activity in women, Libert et al.25 concluded that increased immune activity can enhance the susceptibility of women to autoimmunity. Likewise, Kühne et al.22 suggested that autoimmune disorders associated with the female sex can account for the greater number of adult women with ITP.
In a genomic analysis of Brazilian populations, Mychaleckyj et al.26 genotyped 2010 DNA samples from six studies in Northeastern Brazil, centered on Fortaleza. After exclusion related to low quality, 1538 DNA samples remained, which revealed a mixed European (56.8 %), Amerindian (20.3 %) and African (22.9 %) ancestry. The European component is most likely derived from populations from southern Europe, though the region was also at some point colonized by Dutch settlers.
The authors26 also observed that the implicated genes have known functions that span biological processes. The CIITA gene regulates major histocompatibility complex (MHC) gene transcription and is associated with immune function. The gene complex, including the CIITA and the adjacent DEXI/CLEC16A gene, have been shown to be associated with various autoimmune diseases. Moreover, Bronson et al.27 observed that the rs4774 CIITA missense variant is associated with risk of SLE. This is supported by other researchers such as Sood et al.28, who evaluated the global expression profile of peripheral blood from patients with ITP and identified an ITP-specific signature, which included interferon-induced genes. Several genes correlated with ITP have been shown to be associated with expression signatures in SLE and rheumatoid arthritis, indicating an overlap with other autoimmune disorders.28
Moreover, Cines et al.24 pointed out that environmental and genetic factors may impact platelet turnover, propensity to bleed and response to ITP-directed therapy.
Finally, Landgren et al.29 argued that ethnic, racial, and geographic differences influence virtually all human diseases and that certain conditions exhibit well-established differences between Africans and Europeans. In their study, ITP was identified in 1257 African Americans and 5939 White male veterans, but the prevalence did not differ significantly between the two groups. However, since ITP is thought to be predominant in women, restricting the sample to males may compromise extrapolation of their results.
The age and gender distribution in this study was similar to that of the French population studied by Grimaldi-Bensouda et al.12 but different from that reported for Scandinavian, UK, US and Asian populations, suggesting the importance of geographical and ethnic factors. The finding of 56.8 % of European ancestry in the genetic pool of the population of Ceará,26 and the historical connection with immigrants from southern Europe, possibly overlapping with France, is not without relevance. In addition, the implicated genes also have known associations with autoimmune disorders.
LimitationsThis study has some limitations. First, it was restricted to a single referral center not necessarily representative of the entire Brazilian population. Thus, though the study presented a cross section of the demographic profile of ITP adult patients, it may not be generalizable in other states of Brazil or in other settings, although Ceará is like many regions in low- and middle-income countries. Secondly, the cross-sectional design does not allow direct determination of risk relationships between the social-demographic characteristics and ITP. Thirdly, the patients were evaluated, and their files were written by different doctors, which may lead to some registration bias.
However, we believe it produced meaningful results, suggesting an impact of ethnic and geographical factors on age and gender distribution and on the distribution of secondary ITP.
ConclusionThis study of the epidemiology of ITP in Brazil is intended as a contribution to public health policy development, health care cost modeling and the updating of curricula used in health education. Based on a sample of 187 adult patients, the demographic profile drawn in this study shares similarities with profiles from other countries, especially France, with regard to the prevalence of the female sex and age distribution. These similarities between the profiles of Ceará and France may be related to genetic inheritance. Secondary ITP displayed a bimodal distribution and a linear increase between 38 and >68 years of age.