Consensus of the Brazilian association of hematology, hemotherapy and cellular therapy on patient blood management
More infoHemostasis plays a critical role in surgical procedures and is essential for a successful outcome. Advances in hemostatic agents offer new approaches to controlling bleeding thereby making surgeries safer. The appropriate choice of these agents is crucial. Volume replacement, another integral part of Patient Blood Management (PBM), maintains adequate tissue perfusion, preventing cellular damage. Individualization in fluid administration is vital with the choice between crystalloids and colloids depending on each case. Colloids, unlike crystalloids, increase oncotic pressure, contributing to fluid retention in the intravascular space. Understanding these aspects is essential to ensure safe and effective surgery, minimizing complications related to blood loss and maintaining the patient's hemodynamic status.
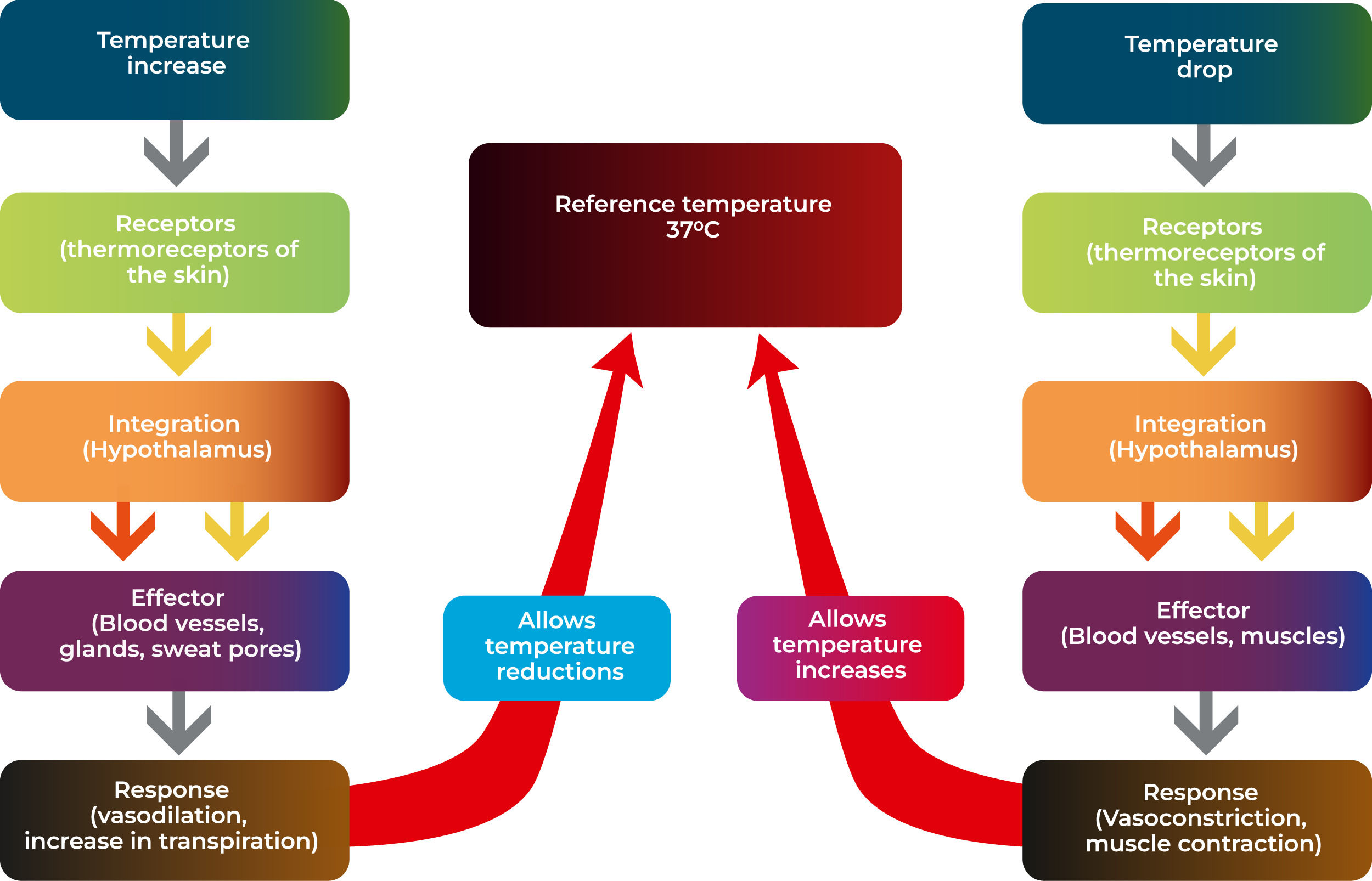
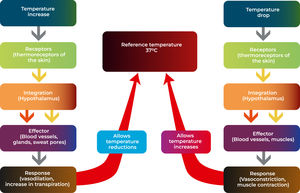
Inadvertent intraoperative hypothermia refers to a situation in which a patient's body temperature drops below normal during a surgical procedure. The pathophysiology of this phenomenon involves a combination of factors. The patient's exposure to a cold environment is a major contributor to intraoperative hypothermia. Operating rooms are typically kept at lower temperatures to reduce the risk of bacterial growth, but this can result in the patient's heat loss. Furthermore, the administration of anesthesia can lead to a decrease in the body's ability to regulate temperature, due to the action of the drugs on the regulatory center located next to the hypothalamus, thereby decreasing the afferent response to hypothermia.
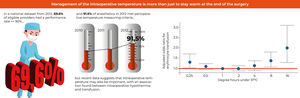
Inadvertent preoperative hypothermia is one of the main adverse events in the course of care of hospitalized patients, whether in the operating room or in interventional procedure units. Publications report incidences above 20 % in the pre-operative period, which reach beyond 60 % post-operatively.1 The journey of this group of patients has currently been the subject of a structured Horizontal Care model, with strategies, protocols, general guidelines aiming at reducing the morbidity and making the patient's journey safe, positive and focused on preventing events, which are well known to the staff involved in preoperative care.
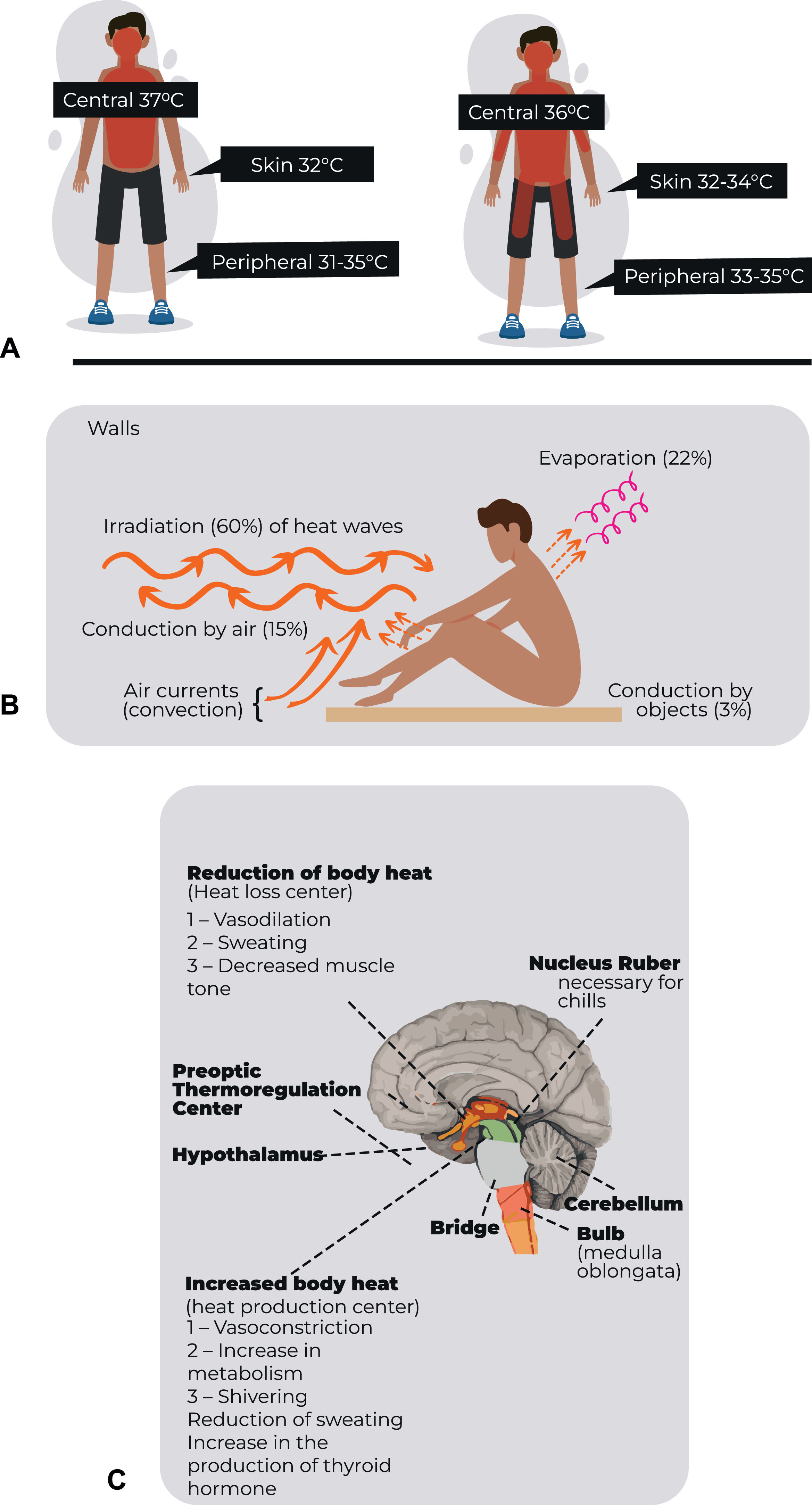
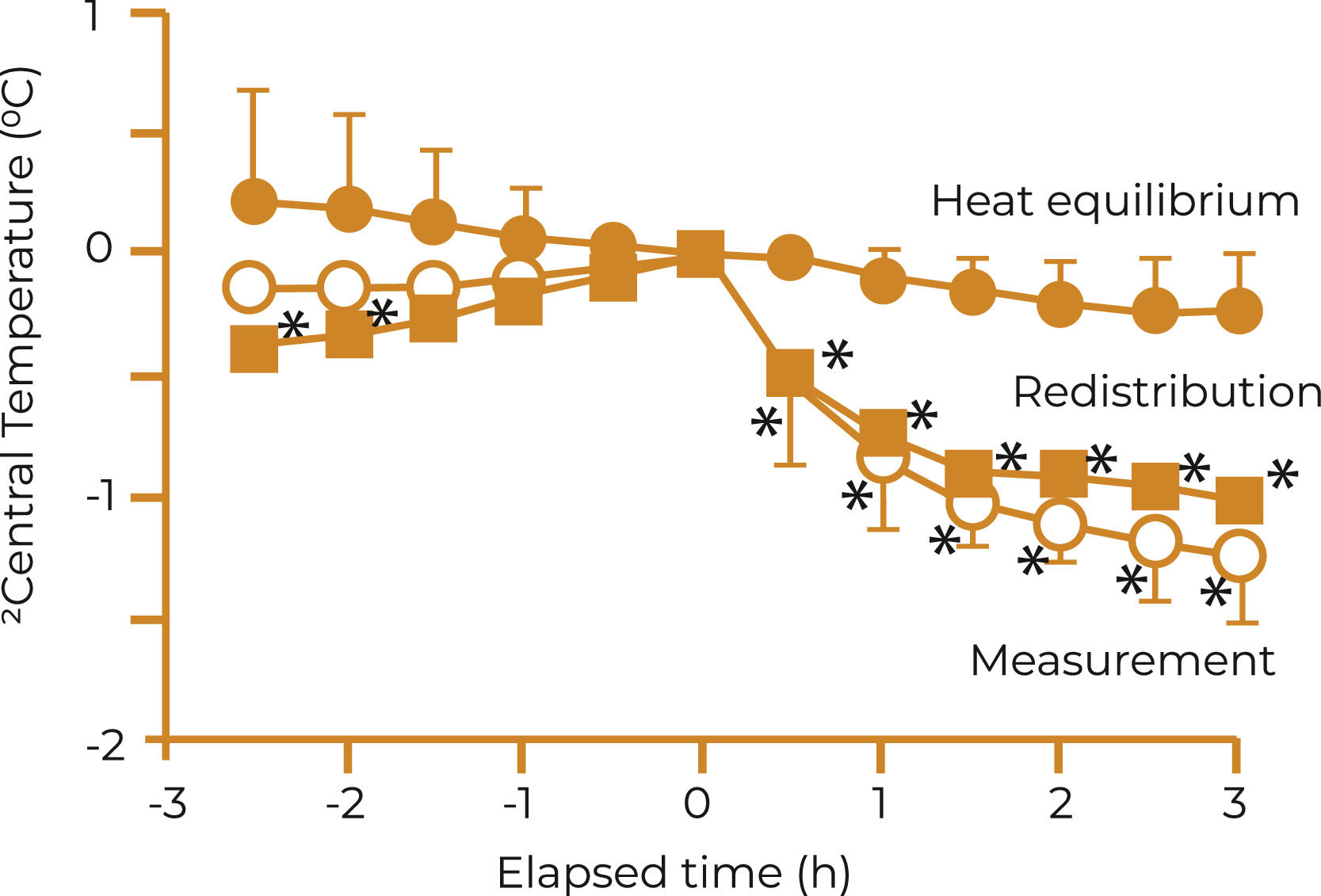
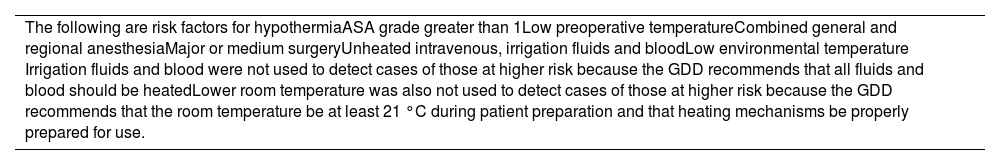
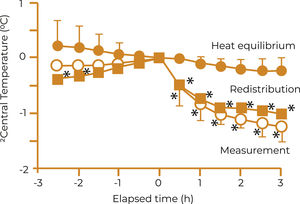
Preoperative hypothermia is defined as a core body temperature below 36 °C (96.8°F) at any time during the preoperative period. After induction of anesthesia, the most important cause of preoperative hypothermia is the distribution of body heat from the center to the periphery, an effect that contributes to much of the reduction in core temperature during the first hour of anesthesia (Figure 1).2
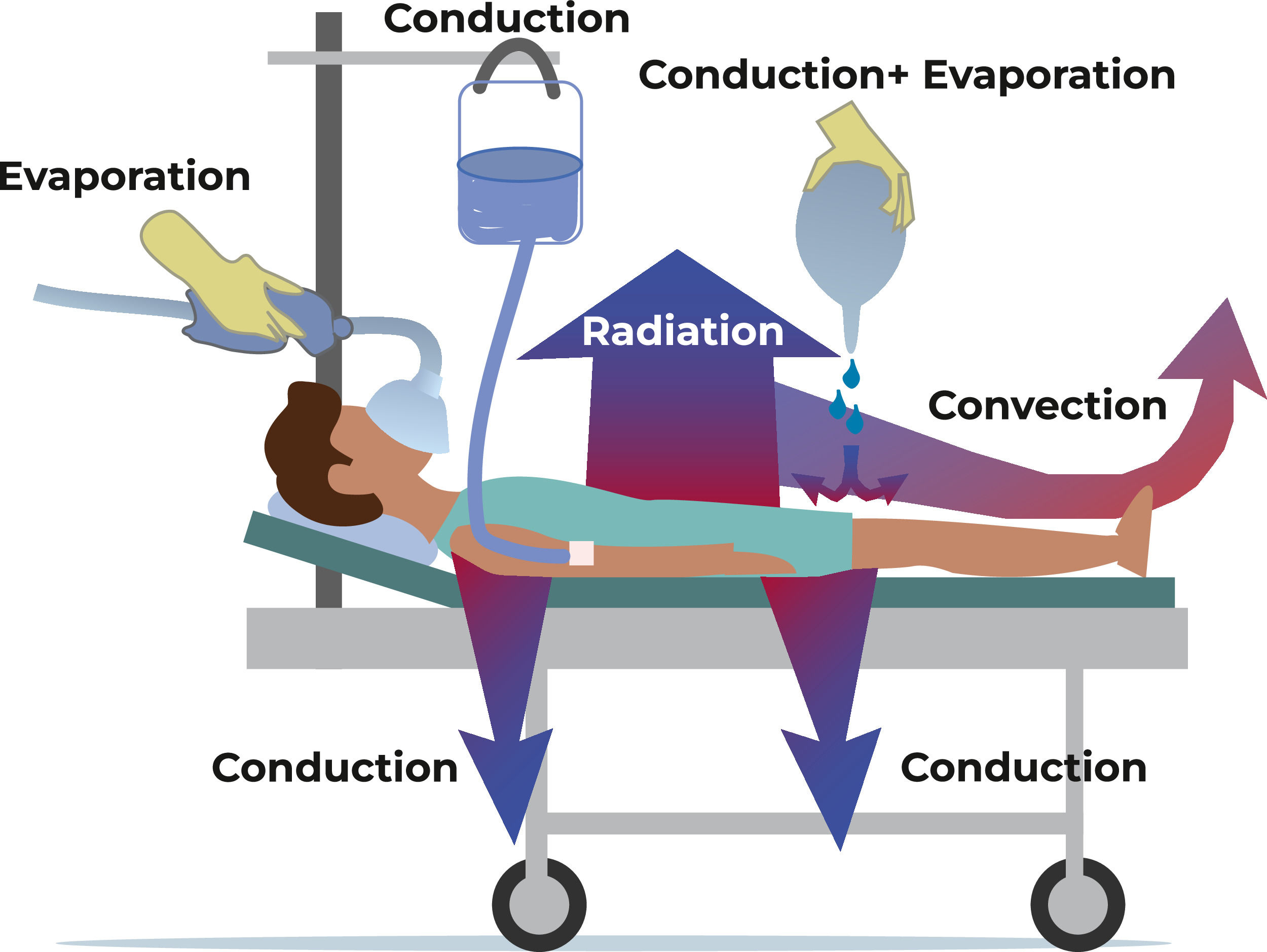
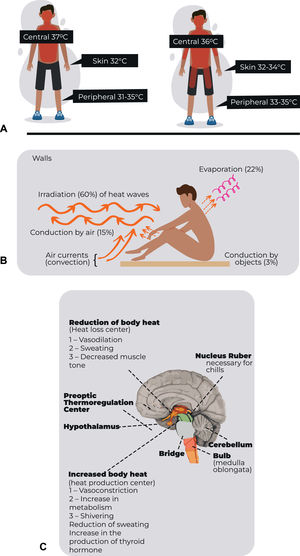
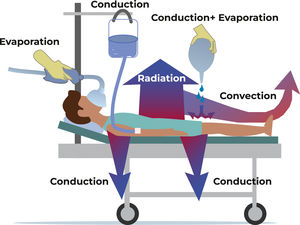
ThermoregulationOne of the main heat loss mechanisms involves radiation and convection during surgery, as patients are often unclothed to perform the surgery. They may also be subjected to procedures that involve internal organ manipulation which also contributes to heat loss. Furthermore, the use of cold intravenous fluids and air conditioning systems can contribute to hypothermia. The pathophysiology of inadvertent intraoperative hypothermia revolves around an imbalance between heat production and heat loss.
Heat production can be impaired by factors such as decreased metabolic rate during anesthesia, decreased muscle activity and the cooling effects of intravenous fluids. Heat loss, on the other hand, can occur by conduction (direct transfer of heat to a cooler surface), convection (transfer of heat to the surrounding air) and evaporation (loss of heat through body surfaces - Figures 2 and 3).
The deleterious effects of hypothermia effect several body systems and structures, negatively impacting the surgical patient's outcome. Hypothermia itself can delay healing and predispose patients to wound infections. Maintaining normothermia intraoperatively will probably reduce the incidence of infectious complications in patients undergoing colorectal resection and shorten their hospitalizations.3
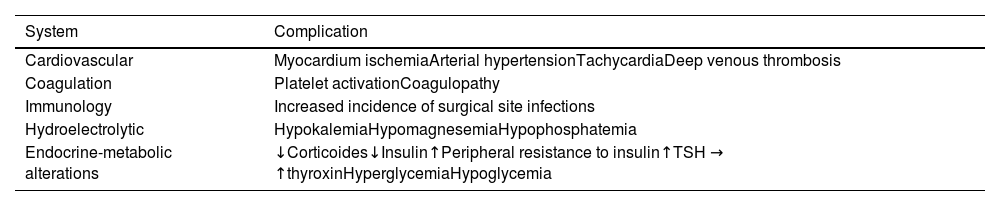
Hypothermia increases blood loss and the possibility of surgical site infections, in addition to prolonging postoperative recovery. Therefore, inadvertent non-therapeutic hypothermia is considered an adverse effect of general and regional anesthesia, which means that understanding hypothermia and its complications and the effective strategies for its prevention in the perioperative period are critical for healthcare providers. It is also essential to plan effective interventions that minimize or facilitate the prevention of complications resulting from anesthesia (Figure 4 and Table 1).2
Complications of hypothermia.
Adapted from Brazilian Guidelines for Preventing and Treating Inadvertent Perioperative Hyperthermia in Adults produced by the Sao Paulo State Society of Anesthesiology. J Infect Control 2018;7(1):01-16.2
The organization of a wide-ranging strategy aimed at prevention and active intervention in situations involving the surgical patient's journey must be a premise of good care dedicated to the patient. Communication within the surgical team is essential to understand and concern about how these events is essential for prevention. As examples, we can highlight information and communication with the patient and family, preoperative fasting time, occurrence of nausea and vomiting in the postoperative period, return to the patient's oral intake, guidance on stopping smoking in the preoperative period, reduction in intraoperative and postoperative use of opioids and inadvertent intraoperative hypothermia.
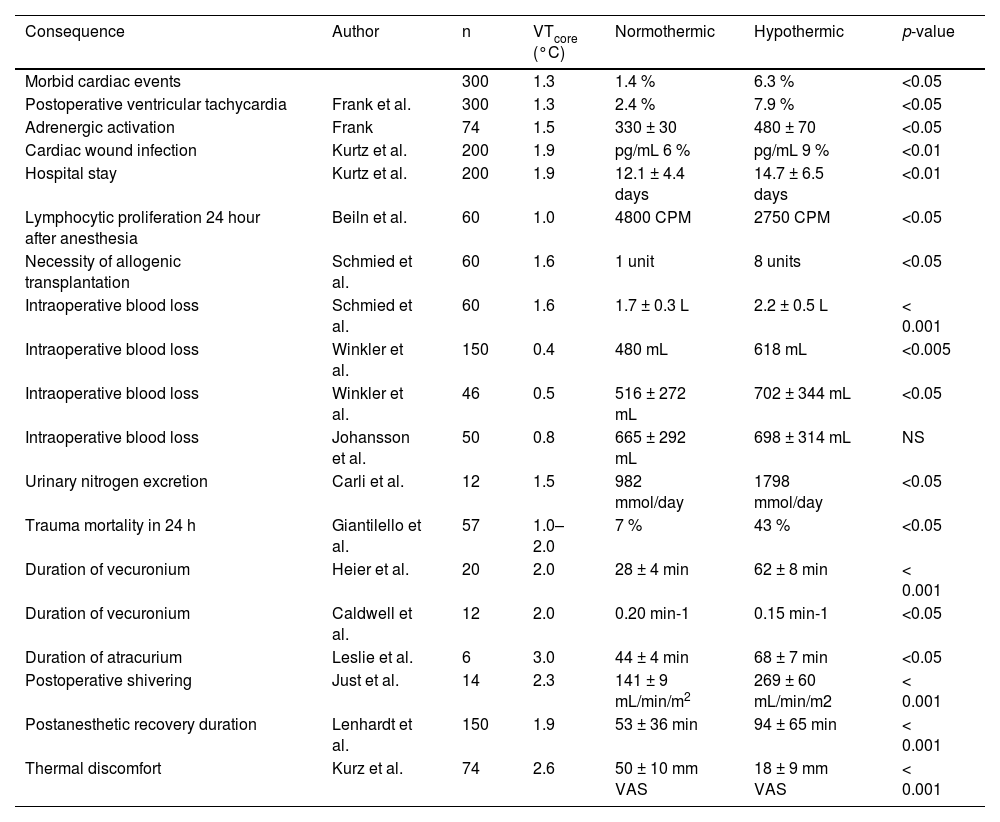
Strategies can be optimized with actions that seek to correct high prevalence events in this group of patients even in the preoperative period, including a reduction in the occurrence of inadvertent preoperative hypothermia. This can be achieved using a preoperative strategy such as heating using active heat transfer systems (e.g. thermal blankets, a technique that uses convection as a means of heat transfer) during hospitalization. Their maintenance in the intra- and post-operative periods helps to optimize care greatly reducing the occurrence of hypothermia, as well as giving clinical advantages (Table 2).4
Consequences of mild perioperative and perianesthetic hypothermia in humans.
Adapted from Reynolds L., Beckmann J., Kurz A. Perioperative complications of hypothermia. Best Pract Res Clin Anesthesiol. 2008 Dec:22(4).645–57.4
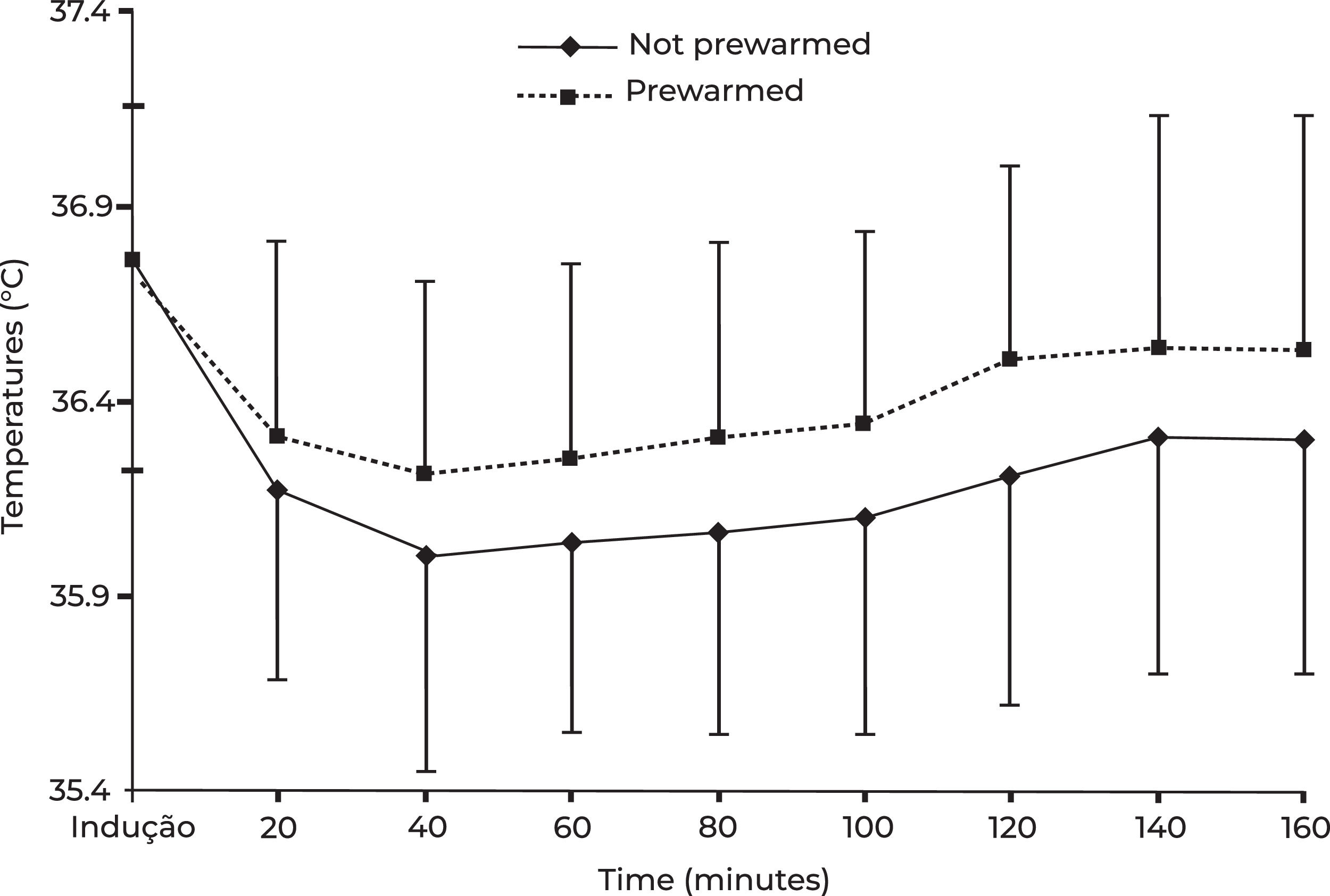
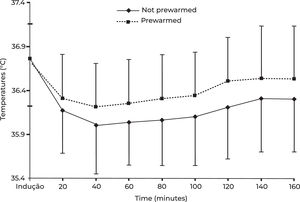
Thirty-one patients were prewarmed in the inpatient unit using an active heated air system (Bair Hugger) for 60 min which continued with active warming intraoperatively and 37 patients in the control group were not. There was a smaller decrease of 0.3 °C in mean core temperature in the preheated group at 40, 60 and 80 min post-induction (p-value ≤0.05). The temperature was maintained above the hypothermic threshold of 36 °C in 21 (68 %) patients in the preheated group compared to 16 (43 %) patients in the control group (p-value <0.05) (Figure 5).5
Patients should be well informed about the surgical procedure and discuss any concerns they have regarding hypothermia with their healthcare professionals.
Each case is unique and preventive measures may vary depending on the patient's characteristics and the type of surgery to be performed.
Furthermore, it was found that patients had a higher risk of cancer recurrence at one year if they had a low preoperative baseline body temperature (<36.6 °C - 17 % vs. 10 %; p-value = 0.034). Low body temperature (mean body temperature <37.4 °C) after surgery was an independent predictor of poor survival outcomes in patients with rectal cancer.6
Body temperature is not homogeneous: in the surgical patient, deep thoracic, abdominal and central nervous system (i.e. core), temperatures generally vary by 2–4 °C in relation to the arms and legs and much of the surface of the body, that is the skin, is even colder. Unlike the core temperature, which is tightly regulated, skin temperature varies markedly depending on environmental exposure (Table 3).
Risk factors for hypothermia.
Adapted from Brazilian Guidelines for Preventing and Treating Inadvertent Perioperative Hyperthermia in Adults produced by the Sao Paulo State Society of Anesthesiology. J Infect Control 2018;7(1):01–16.2
NICE Clinical-Practice-Guideline the management of inadvertent perioperative hypothermia in adults. National Collaborating Centre for Nursing and Supportive Care commissioned by the National Institute for Health and Clinical Excellence (NICE) http://guidance.nice.org.uk/CG65. 2014.7
The temperature of peripheral tissues (mainly arms and legs) depends on present exposure, exposure history, core temperature and thermoregulatory vasomotricity. Core temperature, although it does not completely characterize the content and distribution of body heat, is the single best indicator of thermal status in humans. Core temperature monitoring (e.g., tympanic membrane, pulmonary artery, distal esophagus and nasopharynx) is used to monitor intraoperative hypothermia, prevent overheating and facilitate detection of malignant hyperthermia. Because these sites are not necessarily available or convenient, a variety of near-core sites are also used clinically. These include the mouth, armpit, bladder, rectum and surface of the skin. Each has distinct limitations, but can be used clinically in appropriate circumstances. The level of precision that is clinically necessary has not yet been established. However, a good rule of thumb which has been used in many studies, is that the combined inaccuracy of a site/thermometer combination should not exceed 0.5 °C. One basis for this choice is that the smallest difference has proved to be associated with hypothermia-induced complications. Measuring tympanic temperature using a temperature sensor placed in the tympanic canal or close to the central nervous system (frontal region) allows for more precise and continuous measurements of core temperature (Figure 6).
Recommendation
- •
Active prevention of intraoperative hypothermia is essential for adequate care of the surgical patient. This includes measures such as pre-warming using active heated air warming systems, such as the Bair Hugger, in the inpatient unit, as well as maintaining perioperative warming.
- •
Effective communication within the surgical team is essential to ensure that prevention of hypothermia is a priority at all stages of surgery. A shared understanding of the risks associated with hypothermia and prevention strategies is critical to ensure a coordinated and effective approach.
- •
Accurate monitoring of body temperature, preferably using core temperature measurement methods, such as the tympanic membrane, pulmonary artery, distal esophagus or nasopharynx, is crucial to detect and prevent hypothermia during surgery. This allows timely interventions to maintain the patient's body temperature within normal limits.
Inadvertent intraoperative hypothermia occurs due to a combination of factors such as a cold surgical environment, incorrect anesthesia-induced temperature regulation, exposure of the patient's body and use of certain medical interventions. Understanding the pathophysiology of this condition is crucial to implementing effective preventative measures and optimizing patient outcomes.