Consensus of the Brazilian association of hematology, hemotherapy and cellular therapy on patient blood management
More infoThe use of strategies to reduce blood loss and transfusions is essential in the treatment of surgical patients, including in complex cardiac surgeries and those that use cardiopulmonary bypass. Antifibrinolytics, such as epsilon-aminocaproic acid (EACA) and tranexamic acid (TXA), are widely used in these procedures, as well as in other types of surgeries. These medicines are included in the World Health Organization (WHO) list of ‘essential medicines’. Scientific evidence demonstrates the effectiveness of EACA in reducing bleeding and the need for transfusions in heart surgery. EACA is highly recommended for use in heart surgery by the American Society of Anesthesiology Task Force on Perioperative Blood Management. Regarding the safety of EACA, there is no robust evidence of any significant thrombotic potential. TXA has also been shown to be effective in reducing the use of blood transfusions in cardiac and non-cardiac surgeries and is considered safer than other antifibrinolytic agents. There is no evidence of any increased risk of thromboembolic events with TXA, but doses greater than 2 g per day have been associated with an increased risk of seizures. It is also important to adjust the dose in patients with renal impairment. In conclusion, antifibrinolytics, such as EACA and TXA, are effective in reducing blood loss and transfusion use in cardiac and non-cardiac surgeries, without causing serious adverse effects.
The use of strategies to reduce blood loss as well as to lessen the need for transfusions is crucial in the treatment of surgical patients. Antifibrinolytics are widely used in complex heart surgeries and heart surgeries with cardiopulmonary bypass (CPB), as recommended by the Clinical Practice Guidelines of the Society of Thoracic Surgeons (STS) and the Society of Cardiovascular Anesthesiologists (SCA).1 Outside the context of heart surgery, their perioperative use has been expanded with the aim of reducing blood loss.2
Antifibrinolytics are included in the World Health Organization (WHO) list of ‘essential medicines’;3 they are used in various trauma management protocols, in the prevention and treatment of postpartum hemorrhages and by several surgical specialties. However, with the increased use of these agents, concerns have arisen about their safe use. Antifibrinolytics include epsilon-aminocaproic acid (EACA), tranexamic acid (TXA) and aprotinin.
Epsilon-aminocaproic acidEACA is a highly water-soluble colorless crystal, a synthetic analogue of lysine. It works by blocking the conversion of plasminogen into plasmin thereby inhibiting fibrinolysis.
HistoryEACA was studied in the laboratory for the first time in 1914; its research in human beings was expanded in the late 1950s.4 Japanese researchers tested its use in the treatment of several diseases, such as dysmenorrhea, emesis gravidarum and pregnancy toxemia, and observed that EACA was effective with minimal side effects. At the time, its fibrinolytic activity was not measured, but later studies showed that EACA was a powerful inhibitor of plasminogen activation. Researchers quickly recognized the potential of EACA to control hemorrhages in different clinical settings, including surgery. In the 1960s, EACA was used for the first time in a prostatectomy surgery, with significant results in reducing blood loss.5 EACA was approved by the United States Food and Drug Administration (FDA) in 1964.
Mechanism of action and pharmacokineticsThe proteolytic enzyme plasmin normally hydrolyzes polymerized fibrin resulting in fibrinolysis and dissolution of the fibrin clot. EACA modulates the fibrinolytic pathway by irreversibly binding to the lysine-binding sites of plasminogen. This action prevents the release of plasmin and inhibits fibrinolysis, increasing hemostasis.
Intravenous administration of EACA reaches maximum serum concentrations in approximately 10 min. After prolonged administration, EACA distributes into intra- and extravascular compartments, penetrating red blood cells and other tissue cells. With an elimination half-life of two hours, EACA is mainly excreted by the kidneys, with renal clearance similar to creatinine clearance.2
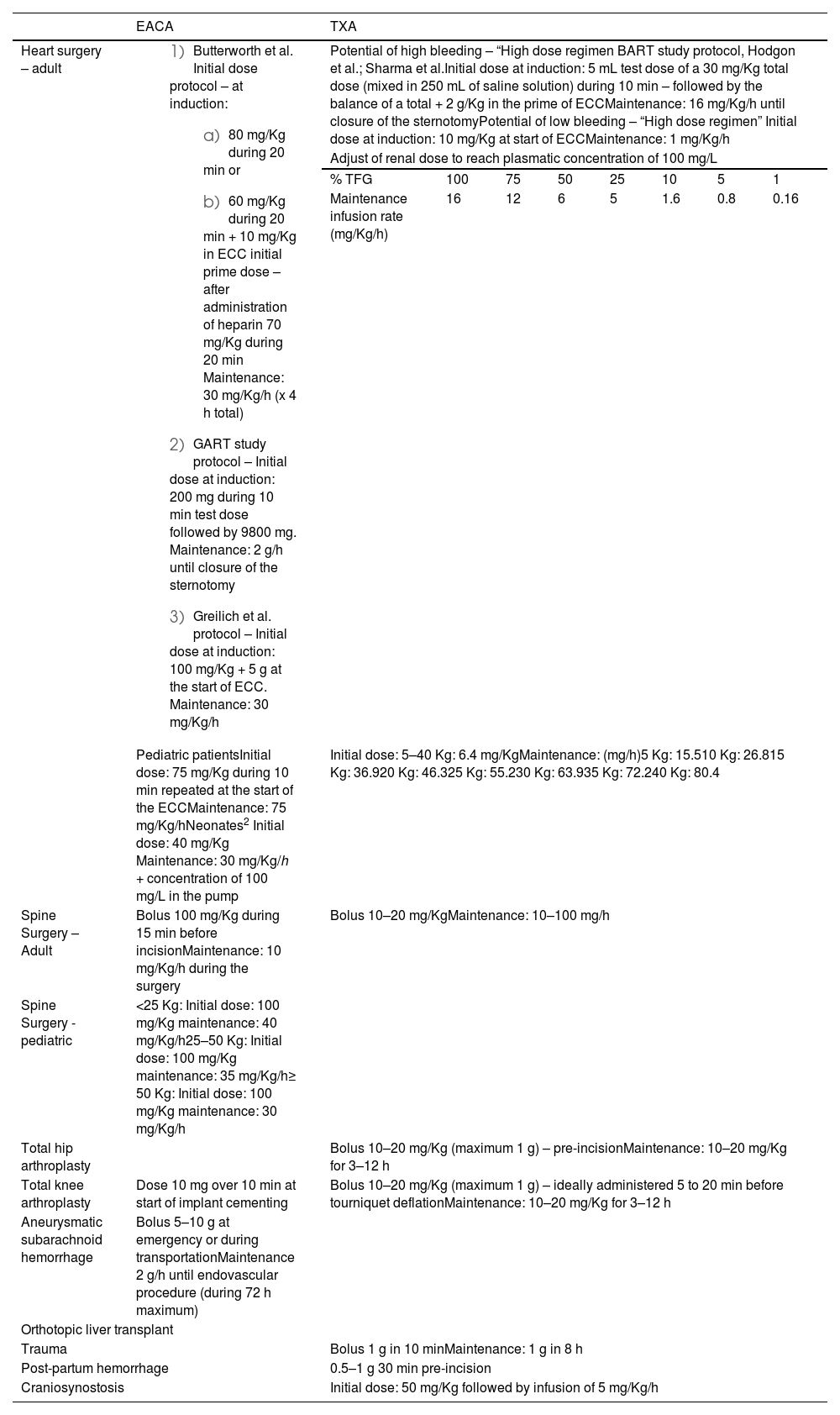
AdministrationThere is no standard guideline for EACA dosing and various dosing regimens have been used in clinical trials. The EACA dose can be administered at the time of induction or after anticoagulation but before starting CPB. Table 1 presents common dosing strategies in cardiac and non-cardiac surgery.2
Dosing strategies of epsilon-aminocaproic acid (EACA) and tranexamic acid (TXA) for adults and children2.
| EACA | TXA | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Heart surgery – adult |
| Potential of high bleeding – “High dose regimen BART study protocol, Hodgon et al.; Sharma et al.Initial dose at induction: 5 mL test dose of a 30 mg/Kg total dose (mixed in 250 mL of saline solution) during 10 min – followed by the balance of a total + 2 g/Kg in the prime of ECCMaintenance: 16 mg/Kg/h until closure of the sternotomyPotential of low bleeding – “High dose regimen” Initial dose at induction: 10 mg/Kg at start of ECCMaintenance: 1 mg/Kg/h | |||||||
| Adjust of renal dose to reach plasmatic concentration of 100 mg/L | |||||||||
| % TFG | 100 | 75 | 50 | 25 | 10 | 5 | 1 | ||
| Maintenance infusion rate (mg/Kg/h) | 16 | 12 | 6 | 5 | 1.6 | 0.8 | 0.16 | ||
| Pediatric patientsInitial dose: 75 mg/Kg during 10 min repeated at the start of the ECCMaintenance: 75 mg/Kg/hNeonates2 Initial dose: 40 mg/Kg Maintenance: 30 mg/Kg/h + concentration of 100 mg/L in the pump | Initial dose: 5–40 Kg: 6.4 mg/KgMaintenance: (mg/h)5 Kg: 15.510 Kg: 26.815 Kg: 36.920 Kg: 46.325 Kg: 55.230 Kg: 63.935 Kg: 72.240 Kg: 80.4 | ||||||||
| Spine Surgery – Adult | Bolus 100 mg/Kg during 15 min before incisionMaintenance: 10 mg/Kg/h during the surgery | Bolus 10–20 mg/KgMaintenance: 10–100 mg/h | |||||||
| Spine Surgery - pediatric | <25 Kg: Initial dose: 100 mg/Kg maintenance: 40 mg/Kg/h25–50 Kg: Initial dose: 100 mg/Kg maintenance: 35 mg/Kg/h≥ 50 Kg: Initial dose: 100 mg/Kg maintenance: 30 mg/Kg/h | ||||||||
| Total hip arthroplasty | Bolus 10–20 mg/Kg (maximum 1 g) – pre-incisionMaintenance: 10–20 mg/Kg for 3–12 h | ||||||||
| Total knee arthroplasty | Dose 10 mg over 10 min at start of implant cementing | Bolus 10–20 mg/Kg (maximum 1 g) – ideally administered 5 to 20 min before tourniquet deflationMaintenance: 10–20 mg/Kg for 3–12 h | |||||||
| Aneurysmatic subarachnoid hemorrhage | Bolus 5–10 g at emergency or during transportationMaintenance 2 g/h until endovascular procedure (during 72 h maximum) | ||||||||
| Orthotopic liver transplant | |||||||||
| Trauma | Bolus 1 g in 10 minMaintenance: 1 g in 8 h | ||||||||
| Post-partum hemorrhage | 0.5–1 g 30 min pre-incision | ||||||||
| Craniosynostosis | Initial dose: 50 mg/Kg followed by infusion of 5 mg/Kg/h | ||||||||
EACA: epsilon-aminocaproic acid; TXA: tranexamic acid; ECC: extracorporeal circulation.
EACA has shown efficacy in reducing hemorrhage and transfusion requirements in adult cardiac surgery with CPB. A 2007 meta-analysis compared the three antifibrinolytic agents and demonstrated that EACA is effective in reducing blood loss and need of transfusions in cardiac surgery, without increasing adverse effects.6 The 2008 BART study, a blinded multicenter randomized trial, compared aprotinin, TXA and EACA in high-risk cardiac surgery, showing that the three agents reduced postoperative hemorrhage, but aprotinin had a higher mortality rate.7
A 2011 Cochrane systematic review showed that EACA reduces blood transfusions in cardiac surgery by 30 % [relative risk (RR): 0.70; 95 % confidence interval (CI): 0.52–0.93] and by 19 % for surgeries in overall [relative risk (RR): 0.81; 95 % CI; 0.67–0.99]. Mortality appears not to have been affected by treatment with any of the antifibrinolytic drugs and lysine analogues did not present serious adverse effects.8 EACA was highly recommended for use in cardiac surgery in the 2015 edition of the American Society of Anesthesiology Task Force on Perioperative Blood Management.9
SafetyIn general, EACA is well tolerated. Due to its action on the fibrinolytic pathway, there is the theoretical potential to generate a pro-thrombotic state with consequent thromboembolic complications. However, there are no robust scientific trials or studies that indicate that EACA has a significantly worrying thrombotic potential. Reports of thrombosis are isolated and studies have not found clear differences between treatment and control groups.2
The relationship between EACA and kidney injury is contradictory. A 2011 Cochrane review found no increases in acute kidney injury associated with EACA when compared with placebo.8 Rhabdomyolysis and myopathy are adverse effects reported with chronic use of EACA. EACA has also been associated with cases of cerebral thrombosis, making it necessary to exercise caution in cases of head trauma and subarachnoid hemorrhage. It is contraindicated in cases of disseminated intravascular coagulation.2
The preservative benzyl alcohol used in intravenous formulations of EACA has been associated with a potentially lethal syndrome in low birth weight infants and newborns known as ‘gasping syndrome’. However, there are no data or case reports specifically implicating EACA. There are some relative contraindications, such as hypersensitivity to benzyl alcohol, parabens, pregnancy and breastfeeding.2Table 2 contains a list of various clinical scenarios and precautions and risks associated with the use of EACA.
Precautions/contraindications for the perioperative use of antifibrinolytics.
| Clinical scenario/patient condition | EACA | TXA |
|---|---|---|
| Allergy of hypersensitivity |
|
|
| History of significant venous or arterial thrombosis or thromboembolic events |
|
|
| Hereditary hypercoagulation states |
|
|
| Acquired and non-primary hypercoagulation states (including risk factors) |
|
|
| Kidney failure/electrolyte disorders |
|
|
| Subarachnoid hemorrhage or concomitant traumatic brain lesion |
|
|
| History of convulsion disorders or uncontrolled convulsion disorders | Doses greater than 2 g daily were associated to a higher risk of convulsions | |
| Concurrent treatment with other procoagulants | Increased risk of thrombosis with the use of Factor IX complex and anti-inhibitor coagulant concentrates |
|
| Disseminated intravascular coagulation | Risk of thrombosis: May require the concomitant heparin use | Use similar precautions as for EACA |
| Pregnancy | Category C: Without animal studies, without controlled data in human pregnancies | Category B agent, but there are no well-controlled studies about the use during pregnancy, its use in pregnancy should be limited |
| Diverse | Chromatopoeia and visual deficiency were reported on use in hemophiliacs |
Similar to EACA, TXA is a synthetic derivative of lysine, which competitively blocks the lysine binding site on plasminogen, thereby inhibiting fibrinolysis. 10
HistoryTXA was discovered by Japanese researcher Utako Okamato in the 1950s. Okamato and his group first published findings about their new drug in the 1960s11 with the original applications of TXA being for the treatment of postpartum hemorrhage and hemophilia. It was only in the 1990s that the use of TXA was applied in heart surgery.
Mechanism of action and pharmacokineticsTXA reversibly blocks lysine binding sites on tissue plasminogen activator (tPA) and plasminogen molecules, resulting in inhibition of fibrinolysis. It acts mainly by blocking high affinity sites.
The pharmacokinetic properties of TXA vary with the route of administration and comorbidities, such as renal failure. TXA has low binding affinity for plasma proteins and is minimally metabolized, being found in greater quantities in the liver, kidneys and lungs. The intravenous administration reaches maximum serum concentrations in about five minutes. The plasma half-life is approximately two hours, maintaining therapeutic levels for 6–8 h.
TXA crosses the placenta, but the concentration in breast milk is very low, with no significant adverse effects on breastfed babies. TXA elimination follows first-order kinetics via glomerular filtration, therefore, dosage adjustments must be made in patients with impaired renal function.2
AdministrationTXA can be administered intravenously, intramuscularly, topically, orally and even nebulized.12 Plasma levels of 10 mg/L have been reported to inhibit only 80 % of tPA activity, while a tenfold higher dose (100 mg/L) is required for 100 % inhibition.2Table 1 presents common dosing strategies in cardiac and non-cardiac surgeries.2
Scientific evidence of effectivenessTXA has become an essential component of antifibrinolytic therapy because it is considered safer than other agents as demonstrated in the BART study.7 A 2011 systematic review and meta-analysis involving eight studies and 544 patients submitted to cardiac surgery found that TXA significantly reduced the use of blood transfusions.13 These results were corroborated by another systematic review and meta-analysis from 2012 that analyzed evidence from several decades and specifically the amount of blood transfused in cardiac surgery. 14 In this analysis, which included 42 studies, it was found that TXA is highly effective in reducing the risk of transfusion (RR: 0.65; 95 % CI: 0.60–0.70; p-value <0.001).
CRASH-2, the largest prospective clinical study to date was carried out in 2010 involving 20,211 adult trauma patients in 274 hospitals of 40 countries.15 The aim of the study was to evaluate the effects of early TXA administration on mortality, occlusive vascular disease and blood transfusions in trauma victims. Comparing the group receiving TXA with the group receiving a placebo, a significant reduction in total mortality was observed, as well as in the risk of death from bleeding (RR: 0.85; 95 % CI: 0.76–0.96; p-value = 0.0077). Importantly, the benefits of TXA were only observed when administered within three hours of patient presentation.
A systematic review with meta-analysis on patients undergoing non-cardiac surgery included 69 randomized clinical trials with 6157 patients.16 TXA reduced the proportion of patients receiving blood transfusions (RR: 0.59; 95 % CI: 0.48–0.72) and the volume of red blood cell units transfused (Mean difference: −0.51; 95 % CI: −0.13 to −0.9) compared to the placebo or usual care. TXA was not associated with differences in deep vein thrombosis, pulmonary embolism, all-cause mortality, length of hospital stay, need for reoperation due to hemorrhage, myocardial infarction, stroke or seizure.
SafetyTXA excretion depends on renal function; it reduces as plasma creatinine levels increase. Therefore, caution must be exercised when administering the medication to patients with renal impairment by adjusting the dose as needed.
The use of TXA in non-cardiac surgeries has increased in recent years, mainly due to the relative safety of the drug in respect to thromboembolic events, as demonstrated in most retrospective analyses. In 2016, the first study was published that prospectively examined the thromboembolic risks of TXA in 4662 patients submitted to myocardial revascularization surgery with and without extracorporeal circulation.17 Of the patients undergoing cardiac surgery, TXA was associated with a lower risk of bleeding than placebo, with no greater risk of death or thrombotic complications within 30 days after surgery. In the CRASH-2 study, which analyzed the use of TXA in trauma, no significant differences were observed in thrombotic events between the groups. 15
A systematic review with meta-analysis of randomized clinical trials was carried out to evaluate the safety of TXA in patients with bleeding.18 A total of 234 studies with 102,681 patients were included in the meta-analysis. In patients with bleeding, there was no evidence that TXA increased the risk of thrombotic events, venous thromboembolism, acute coronary syndrome or stroke.
More recently, the Perioperative Ischemic Evaluation–3 (POISE-3) trial was published, which evaluated the efficacy and safety of using TXA in patients undergoing non-cardiac surgery.19 This double-blind placebo-controlled multicenter randomized clinical trial included 9535 patients. The incidence of bleeding was significantly lower with TXA than with placebo. The composite safety outcomes of myocardial infarction, ischemia due to isolated elevation of troponin, nonhemorrhagic stroke, peripheral arterial thrombosis, and symptomatic proximal venous thromboembolism at 30 days was similar between the groups (14.2% vs. 13.9 %; hazard ratio: 1.02; 95 % CI: 0.92–1.14], but the p-value for non-inferiority was not reached (p-value = 0.04).
Although there is no evidence of an increased risk of thromboembolic events in large studies, some authors recommend caution when administering the drug to patients with a history of thromboembolic events, hypercoagulable states or use of other prothrombotic medications.2 In these cases, topical TXA may be a better option in patients at increased thrombotic risk. In a systematic review with meta-analysis of 71 studies (7539 patients), topical TXA reduced the incidence of blood transfusion in adults undergoing surgery without any notable associated adverse events.20
Although the systematic review with meta-analysis of randomized clinical trials carried out to evaluate the safety of TXA in patients with bleeding did not find any increase in the risk of thrombotic events,18 it identified a dose-dependent increase in the risk of seizures, with doses higher than 2 g per day being associated with a higher seizure risk. In the POISE-3 study, a TXA dose of 2 g per day was evaluated compared with placebo, with seizures being similar and uncommon in both groups.19Table 2 lists precautions for the safe and effective administration of TXA.
AprotininAprotinin is a naturally occurring 58-amino acid single-chain polypeptide originally extracted from bovine tissue and currently produced using recombinant technology.
HistoryAprotinin, initially described in the 1930s, entered the clinical scene in the 1950s to treat hyperfibrinolytic conditions such as pancreatitis. In the early 1980s, Kirkland and colleagues made an accidental discovery about the prohemostatic properties of aprotinin during cardiopulmonary bypass (CPB) surgery when they observed an "exceptionally dry cardiac surgical field" after using aprotinin to attenuate the inflammatory response and post-perfusion syndrome associated with CPB.2 Subsequent studies focused on the effects of aprotinin on coagulation, with one landmark article demonstrating its ability to significantly reduce blood loss and the use of transfusion in cardiac surgery.21 In 1993, aprotinin received FDA approval for routine use in coronary artery bypass graft surgery.
A challenge for the use of aprotinin occurred with the publication of the study by Mangano et al. in 2006.22 The study of 4374 adult patients undergoing coronary surgery revealed that the use of aprotinin was associated with a greater risk of complications, such as kidney failure. A second study conducted in the same year also reported an increase in renal dysfunction with aprotinin.23 These findings led the FDA to add renal dysfunction to existing safety concerns about aprotinin.
However, the direct association between aprotinin and perioperative renal dysfunction has been questioned due to the relationship between transfusion and renal failure, which has made it difficult to identify the role of aprotinin in the development of this dysfunction. The situation, however, worsened with the publication of the results of the BART trial in 20087, which observed an increase in mortality among patients treated with aprotinin compared to those treated with TXA or EACA, although the difference was not statistically significant.
The results of these studies led to the withdrawal of aprotinin from the United States in late 2007, followed by regulatory agencies suspending the drug's license in Canada and Europe in 2008.2 Furthermore, a 2011 Cochrane review concluded that although aprotinin may be more effective in reducing blood loss and transfusion use compared with other antifibrinolytic medications, it was associated with a higher risk of death.8
However, the studies that support this evidence have been contested, raising methodological questions.24 Concerns about the BART study led Canada's regulatory authority to convene an advisory panel to examine these issues. The panel identified serious methodological problems in the study and concluded that the benefit of using aprotinin in non-complex cardiac surgeries could outweigh the risk. As a result, aprotinin was made available again in Canada.25
In 2012, the European Medicines Agency also recommended lifting the suspension of aprotinin after reviewing the risks and benefits of antifibrinolytic drugs. However, it is important to mention that the authors of the BART study refuted these conclusions.26 The Nordic® laboratory became a distributor of aprotinin in place of Bayer® in 2012 and began collecting data for safety assessment. This controversy surrounding aprotinin generated confusion among doctors regarding its role, especially after the release of the license by the European Medicines Agency.25
Mechanism of action and pharmacokineticsAprotinin inhibits the action of several serine proteases (such as trypsin, chymotrypsin, plasmin and tissue and plasma kallikreins) through the formation of reversible enzyme inhibitor complexes. By inhibiting kallikrein, aprotinin indirectly inhibits the formation of activated factor XII, a biochemical reaction normally amplified by kallikrein through a positive feedback mechanism. Therefore, aprotinin inhibits the initiation of coagulation and fibrinolysis induced by the contact of blood with a foreign surface.27
Aprotinin is metabolized by lysosomal enzymes and excreted renally with an elimination half-life of 5 to 10 h.
AdministrationAprotinin is inactive when administered orally. It is administered intravenously in an initial loading dose, followed by a continuous infusion.27
Scientific evidence and safetyThe only absolute contraindication for aprotinin is a positive aprotinin-specific IgG antibody test prior to use. However, there are no guidelines for applying this test.
There must be contingencies for anaphylaxis or anaphylactoid reactions whenever the drug is used and special care must be taken with patients who have received aprotinin in the last 12 months. Aprotinin may also falsely elevate or prolong several in vitro coagulation indices, including partial thromboplastin time and activated clotting time (ACT) measurements. For this reason, it is recommended to monitor anticoagulation with specific tests (minimum celite ACT of 750 s or kaolin ACT of 480 s).2
Aprotinin is a potent inhibitor of fibrinolysis and is effective in reducing transfusion in cardiac surgery. However, its safety profile, discussed previously, continues to be a source of controversy among experts around the world.2 A discussion of these controversies goes beyond the scope of this text.
Although not free from potential bias, data collected in the Nordic® laboratory safety registry may help better evaluate aprotinin safety controversies. Prospects for aprotinin may include evaluating its efficacy and safety in complex and higher-risk surgeries in robust randomized clinical trials. Several studies suggest that in these more complex procedures, aprotinin may have advantages over other available antifibrinolytic drugs.25 However, given the narrow indications and controversy, it remains unclear whether doctors who have become accustomed to performing surgeries without aprotinin will reinvest their trust in this drug.
Recommendations
- •
We recommend that a lysine analogue, such as tranexamic acid or epsilon-aminocaproic acid, should be considered in all adults undergoing surgery, especially in patients expected to experience moderate blood loss (>500 mL), as long as they do not have contraindications to its use.
- •
We recommend that preferentially tranexamic acid is used as the lysine analogue compared to epsilon-aminocaproic acid, due to the greater volume of literature proving its efficacy and safety in different clinical scenarios.
In conclusion, antifibrinolytics, including epsilon-aminocaproic acid (EACA) and tranexamic acid (TXA), play a crucial role in reducing blood loss and decreasing the need for transfusions in both cardiac and non-cardiac surgical patients. Scientific evidence demonstrates the effectiveness of these medicines, as recommended by clinical guidelines and included on the World Health Organization's list of ‘essential medicines.’ Furthermore, they are considered safe with no evidence of an increase in thromboembolic phenomena or other adverse events. These findings reinforce the importance of appropriate use of antifibrinolytics to optimize clinical results and improve the safety of patients undergoing surgical procedures. Future research should continue to explore their therapeutic potential and improve their use in the clinical practice.