Retinal vein occlusion is the second most common cause of visual loss due to retinal vascular disease after diabetic retinopathy.1 Among the risk factors described, it is well known that the hypercoagulable state present in neoplasias can culminate in vein occlusion. It is described that any ocular structure may be involved in acute leukemia2; involvement of the choroid and retina is the most common. However, leukemic cells can infiltrate the conjunctiva and lacrimal glands, producing obvious masses. Karesh et al. published a two year prospective study of newly diagnosed adults with acute myeloid leukemia; 64% of patients had retinal or optic nerve abnormalities where hemorrhages and cotton wool spots (a consequence of nerve fiber ischemia) were the most frequent findings.3 The association between central retinal vein occlusion and acute lymphoblastic leukemia (ALL) relapse has rarely been described though.4–6 We hereby report a case of central retinal vein occlusion as the presenting manifestation of relapse in ALL.
Case reportA 59-year-old female was diagnosed with ALL in November 2013. At that time, she had the following laboratory results: hemoglobin: 8.7g/dL; red blood cells: 2.95×109/μL; MCV: 89fL; total leukocytes: 18.66×109/L; lymphocytes: 5.374×109/L; segmented neutrophils: 2.930×109/L; blasts: 9143cells/μL; uric acid: 5.2mg/dL; lactic dehydrogenase: 1672U/L; creatinine: 3.1mg/dL; and urea: 83mg/dL. She received volemic resuscitation for tumor lysis syndrome. Subsequently, she developed pneumonia caused by Cryptococcus neoformans and herpes zoster skin lesions. Treatment was made with meropenem, amphotericin and acyclovir. In January 2014, after completing treatment for the infections, she was submitted to chemotherapy induction using the hyperCVAD regimen – course A (cyclophosphamide, vincristine, doxorubicin and dexamethasone). Immunophenotyping performed in February 2014 showed remission of the disease.
In March 2014 she presented febrile neutropenia and typhlitis. Empiric treatment with cefepime was started and the hyperCVAD regimen was interrupted. Blood cultures identified Escherichia coli and Klebsiella pnemoniae. Treatment was completed on April 20th 2014.
After hospital discharge, she was submitted to outpatient re-induction therapy with the adapted Berlin-Frankfurt-Munster (BFM) protocol (dexamethasone, vincristine, doxorubicin and l-asparaginase) in June 2014. In July she was unable to complete the fourth cycle of therapy due to hematological toxicity (hemoglobin: 9.0g/dL; red blood cells: 2.71×109/μL; total leukocytes: 0.870×109/L; neutrophils: 0.628×109/L; and platelets: 13×109/L).
In August 2014 she came to our hospital emergency department complaining of a headache of the right side of her head, sensitivity to light, nausea, vomiting and visual loss in the right eye that had started four days previously. The neurological exam showed no abnormality, except for the eye fundus examination, which revealed papilledema, intraretinal peripapillary and inframacular hemorrhage in the right eye. The left eye presented a pre-retinal hemorrhage.
Laboratory exams did not reveal any abnormality. A coagulation panel showed platelets 154×109/L; prothrombin time activity: 100%; international normalization ratio (INR): 1.00; and activated partial thromboplastin time: 36.6s.
A nuclear magnetic resonance image (MRI) was made, and the only abnormality was a hypointense lesion evidenced in the T2 sequence in the right temporal posterior region, which was probably a sequelae of a previous hemorrhagic infarct.
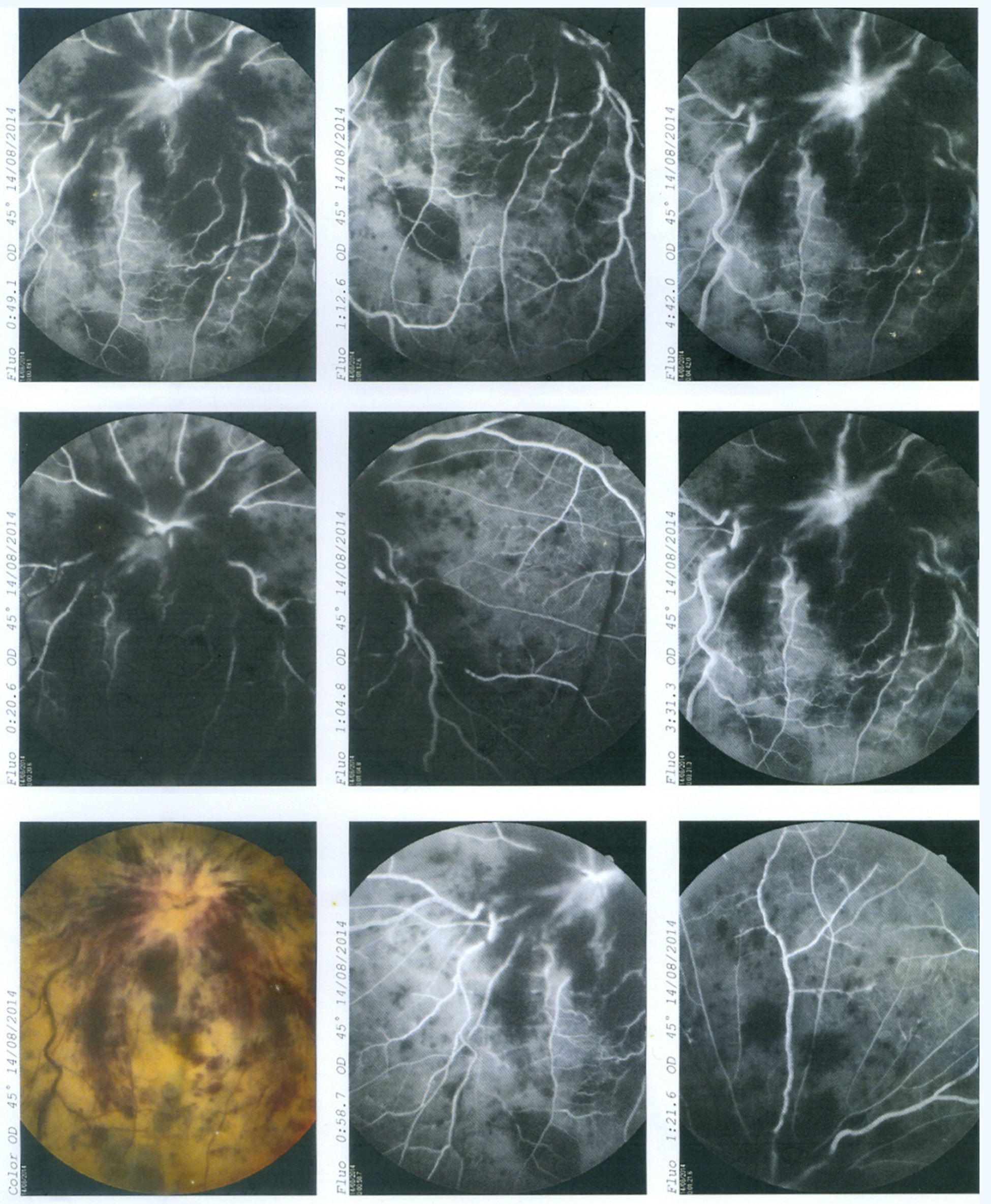
She was then submitted to a fluorescein angiography that revealed occlusion of the central retinal vein (Figure 1).
In order to exclude any infectious etiology, a lumbar puncture was made, with a normal opening pressure (150cmH2O). Cerebrospinal fluid analysis evidenced low glucose levels (28mg/dL and 89mg/dL in blood); high protein levels (89mg/dL); cellularity 2520cells/μL; 94% blasts; 5% monocytes; and red blood cells: 220cells/μL. Cultures for fungus, bacteria and cytomegalovirus antigenemia and herpes virus polymerase chain reaction (PCR) were all negative.
She was not taking any drug that would potentially be capable of inducing retinal vein occlusion.
In order to complete the evaluation of possible intracerebral vein thrombosis, the patient was submitted to a vascular MRI that revealed thickening of the right optic nerve and optic chiasm protuberance.
Immunophenotyping of the liquor had predominance of CD10, CD19, DC22, CD34, HLA DR cells, suggesting B lineage ALL. Lymphoblasts were identified in the cytopathological exam and bone marrow cytology confirmed medullar infiltration.
After confirming neurological relapse of ALL, intrathecal chemotherapy was given with dexamethasone, cytarabine and methotrexate. She had complete remission of headache, but had no improvement of her visual loss.
A magnetic resonance angiography of the central nervous system (CNS) was carried out to exclude other possible vascular thrombosis, but no alteration was found in the exam, except for infiltration of the right optic nerve.
She was discharged from hospital after two sessions of intrathecal chemotherapy, and continues outpatient treatment.
DiscussionThere are few cases reported in the literature showing ocular nerve infiltration as an isolated manifestation of ALL relapse, even though it is a consequence of CNS involvement with severe prognosis. In the case reported herein, the patient had a headache associated with visual loss, which strongly suggests CNS damage. Once her ophthalmologic exam showed only central retinal vein occlusion (CRVO), the clinical discussion focused on the etiology of the underlying process: whether it was a consequence of a hypercoagulable state or due to direct invasion of neoplastic cells since both conditions can culminate in CRVO.
In order to elucidate this question, a magnetic resonance angiography was performed to exclude other possible vein occlusions in the CNS, but the only finding was optic nerve infiltration, which had not been evident until this moment. It has already been described that MRI is useful in the early detection of ocular involvement.7
Even though CRVO is related with an hypercoagulable state, all the cases described in the literature that associate CRVO with ALL are secondary to an infiltration of leukemic cells.4–6 All cases show infiltration of the optic disk preceding vessel occlusion.
Treatment described in these cases consists in intrathecal chemotherapy and radiotherapy.8,9 There is no benefit in prescribing vascular endothelial growth factor (VEGF) inhibitors in these cases, as there is combined damage of the vein circulation and the optic nerve conduction; the latter can cause irreversible visual loss.10
ConclusionCNS relapse can precede hematological signs and symptoms, and regular ophthalmologic exams should be instituted in patients with ALL. If ocular symptoms are present and the ophthalmologic exam is normal, a MRI should be considered. In cases of ALL and retinal vessel occlusion, always consider optic nerve infiltration and rapidly institute treatment with intrathecal chemotherapy and radiotherapy to avoid irreversible damage.
Conflicts of interestThe authors declare no conflicts of interest.