Fanconi anemia (FA) is a rare genetic disease characterized by congenital malformations and bone marrow failure. One of the most common oral diseases in individuals with FA is periodontitis and adequate self-perception of periodontal status could contribute to its prevention and early detection.
AimTo compare oral health self-perception, measured by a questionnaire, with the clinical oral condition of patients with FA.
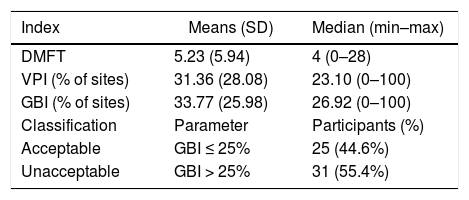
Methods and ResultsFifty-six patients with FA, over 11 years of age, answered a questionnaire about dental history and self-reported oral health. Decayed, missing, and filled teeth (DMFT), Visible Plaque Index (VPI) and Gingival Bleeding Index (GBI) were measured. The median age of participants was 21 years (min 11, max 44), 31 (55%) were females and 25 (45%) males. Thirty-five (62.5%) participants rated their oral condition as satisfactory and 7 (12.5%) participants reported tooth mobility, 10 (17.9%) exposed roots and 21 (37.5%) gingival bleeding. Clinical examination detected average DMFT = 5.23, VPI = 31.36% and GBI = 33.77%. The gingival bleeding report was more frequent among individuals with higher GBI (p = 0.014). The DMFT was higher in those who had already undergone dental treatments (p = 0.031). There was an association between participants who presented dental caries and who rated their oral health as poor (p = 0.03). The question “Do your gums bleed easily?” had good accuracy in the evaluation of periodontal disease (p = 0.68).
ConclusionOral health self-perception of individuals with FA about gingival inflammation was associated with their gingival bleeding index.
Fanconi anemia (FA) is an autosomal recessive genetic disorder characterized by congenital malformations, such as short stature, microcephaly, abnormal thumbs, skin hyperpigmentation characterized by “café-au-lait” spots and bone marrow failure. It is recognized that patients with this syndrome have an increased risk to develop malignancies, such as acute myeloid leukemia and solid tumors, such as head and neck, liver, and gynecologic cancers.1,2
It is controversial if individuals with FA have a poorer oral status than those non-affected by the disease,3 however, a higher microbial load has been speculated as a risk factor for oral malignancies in FA.4 Periodontal disease, an infectious disorder caused by pathogenic bacteria associated with an impaired host-immune response, affects up to 86% of these patients and must be prevented.4–8
The parameters for determining periodontal health are measured in a clinical examination that includes probing attachment loss, probing pocket depths, bleeding on probing and radiological bone loss.9 This requires trained dental examiners, dental equipment and infection-control protocols, which can be expensive and time-consuming.10
The use of valid self-report measures of periodontal diseases can be considered as a low-cost alternative to facilitate epidemiological studies and allow for surveillance of the periodontal condition of the population.11 Some studies have shown self-report assessment as an effective tool, for the assessment of periodontal condition. Previous data shows it has acceptable validity, ranging from moderate to high when compared to the clinical examination.12,13 In this context, a self-perception consistent with the clinical parameters could contribute to the prevention and earlier diagnosis of periodontal diseases, mostly in individuals requiring complex clinical care.
The aim of this study was to evaluate the ability of individuals with Fanconi anemia to perceive their periodontal condition. To do so, the answers to a self-reported questionnaire were compared with the clinical measurement of periodontal status in this population.
Material and methodsThis study was approved by the Brazilian National Research Ethics Committee (Approval number 1.219.800). All subjects diagnosed with FA who participated in the 4th Brazilian FA Family Meeting (Curitiba, Brazil) were invited to take part in the research. Individuals with 18 years of age or older who accepted to participate in the study signed informed consent. An assent form was provided for those younger than 18 years and a consent form was signed by their parents.
Participants answered a questionnaire including socio-demographic, education level (elementary school, high school or college graduate) and behavioral information, as well as dental history. Subsequently, they responded to a set of 8 self-reported oral health questions, adapted to Portuguese, from a questionnaire validated in English and Spanish.14 Hematological status was collected from medical records.
The clinical examination was performed by a single generalist dentist using artificial light, gauze, mouth mirror and dental floss. This professional was trained by a periodontist in a pilot study. The Visual Plaque Index (VPI) was determined using the dichotomous plaque score of 6 sites for each natural tooth selected (all the four first molars, right superior central incisor, left inferior central incisor).15 The number of decayed, missing and filled teeth (DMFT) was determined according to the World Health Organization (WHO) guidelines, and the full-mouth Gingival Bleeding Index (GBI) was determined by the presence or absence of bleeding from the gingival sulcus after flossing.16
The data collected were organized and tabulated in the Statistical Package for the Social Sciences® (SPSS Inc., Chicago, IL, USA), version 20.0, for descriptive and analytical statistics. The association between the self-reported oral health and the clinical measurement and hematologic status were assessed with the Mann-Whitney U-test. A p-value < 0.05 was considered statistically significant. Diagnostic tests (sensitivity, specificity, accuracy and ROC curve) were performed to measure the performance of each question, using the GBI as the reference for oral health evaluation. For this purpose, the GBI was dichotomized in “acceptable” for values lower or equal to 25% and “unacceptable” for values higher than 25%.
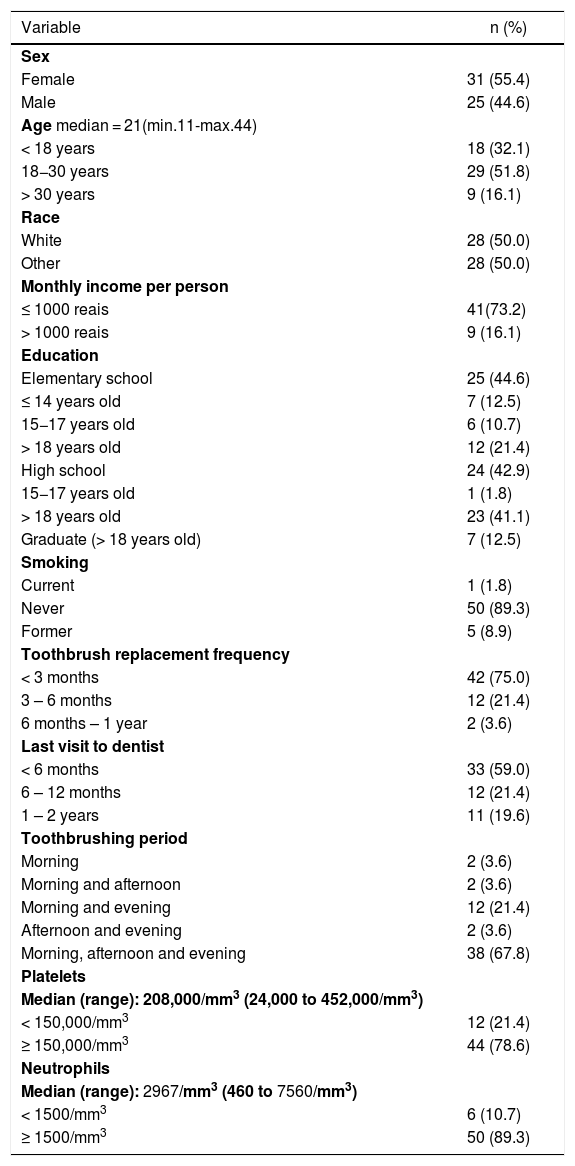
ResultsSixty-two individuals with FA agreed to take part in the study. From them, 6 were excluded due to the use of orthodontic appliances. The sample consisted of 56 participants whose socio-demographic, behavioral, dental history and hematological data are shown in Table 1.
Sociodemographic and behavioral data of participants.
| Variable | n (%) |
|---|---|
| Sex | |
| Female | 31 (55.4) |
| Male | 25 (44.6) |
| Age median = 21(min.11-max.44) | |
| < 18 years | 18 (32.1) |
| 18−30 years | 29 (51.8) |
| > 30 years | 9 (16.1) |
| Race | |
| White | 28 (50.0) |
| Other | 28 (50.0) |
| Monthly income per person | |
| ≤ 1000 reais | 41(73.2) |
| > 1000 reais | 9 (16.1) |
| Education | |
| Elementary school | 25 (44.6) |
| ≤ 14 years old | 7 (12.5) |
| 15−17 years old | 6 (10.7) |
| > 18 years old | 12 (21.4) |
| High school | 24 (42.9) |
| 15−17 years old | 1 (1.8) |
| > 18 years old | 23 (41.1) |
| Graduate (> 18 years old) | 7 (12.5) |
| Smoking | |
| Current | 1 (1.8) |
| Never | 50 (89.3) |
| Former | 5 (8.9) |
| Toothbrush replacement frequency | |
| < 3 months | 42 (75.0) |
| 3 – 6 months | 12 (21.4) |
| 6 months – 1 year | 2 (3.6) |
| Last visit to dentist | |
| < 6 months | 33 (59.0) |
| 6 – 12 months | 12 (21.4) |
| 1 – 2 years | 11 (19.6) |
| Toothbrushing period | |
| Morning | 2 (3.6) |
| Morning and afternoon | 2 (3.6) |
| Morning and evening | 12 (21.4) |
| Afternoon and evening | 2 (3.6) |
| Morning, afternoon and evening | 38 (67.8) |
| Platelets | |
| Median (range): 208,000/mm3 (24,000 to 452,000/mm3) | |
| < 150,000/mm3 | 12 (21.4) |
| ≥ 150,000/mm3 | 44 (78.6) |
| Neutrophils | |
| Median (range): 2967/mm3 (460 to 7560/mm3) | |
| < 1500/mm3 | 6 (10.7) |
| ≥ 1500/mm3 | 50 (89.3) |
In the open question about how many times the subject used dental floss in the previous week, most of the responders (n = 26, 46.4%) said they had not used it, 9 (16.1%) had used it twice and 9 (16.1%) had used it daily. When the same question was asked about the use of mouthwash, 44 (78.6%) participants said they had not used it and 7 (12.5%) had used it daily.
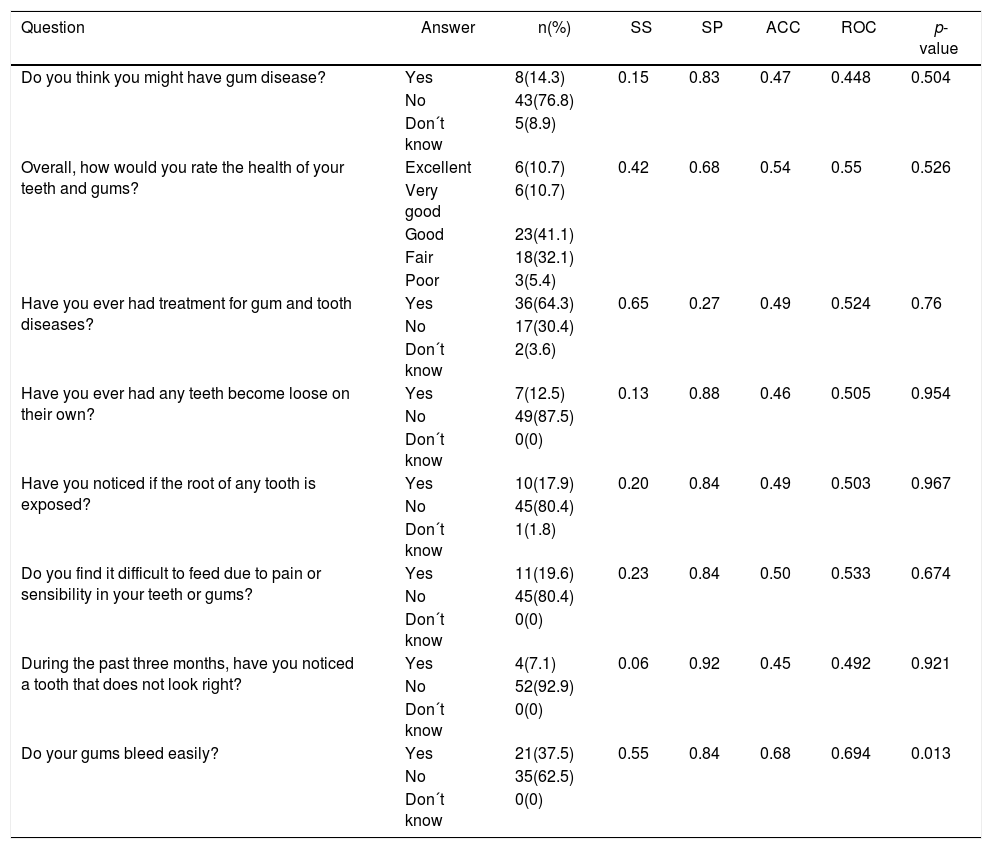
Thirty-six (64%) participants had already undergone some dental treatment before. Dental restoration (43%) was the most frequent one, followed by endodontic treatment (20%), extraction (20%), scaling and root planning (9%) and professional cleaning (5%). Table 2 shows the frequency of responses to each self-reported question from the questionnaire. Clinical data of participants are presented in Table 3.
Frequency of responses for self-perception of periodontal health questionnaire and diagnostic tests for each question in relation to GBI.
| Question | Answer | n(%) | SS | SP | ACC | ROC | p- value |
|---|---|---|---|---|---|---|---|
| Do you think you might have gum disease? | Yes | 8(14.3) | 0.15 | 0.83 | 0.47 | 0.448 | 0.504 |
| No | 43(76.8) | ||||||
| Don´t know | 5(8.9) | ||||||
| Overall, how would you rate the health of your teeth and gums? | Excellent | 6(10.7) | 0.42 | 0.68 | 0.54 | 0.55 | 0.526 |
| Very good | 6(10.7) | ||||||
| Good | 23(41.1) | ||||||
| Fair | 18(32.1) | ||||||
| Poor | 3(5.4) | ||||||
| Have you ever had treatment for gum and tooth diseases? | Yes | 36(64.3) | 0.65 | 0.27 | 0.49 | 0.524 | 0.76 |
| No | 17(30.4) | ||||||
| Don´t know | 2(3.6) | ||||||
| Have you ever had any teeth become loose on their own? | Yes | 7(12.5) | 0.13 | 0.88 | 0.46 | 0.505 | 0.954 |
| No | 49(87.5) | ||||||
| Don´t know | 0(0) | ||||||
| Have you noticed if the root of any tooth is exposed? | Yes | 10(17.9) | 0.20 | 0.84 | 0.49 | 0.503 | 0.967 |
| No | 45(80.4) | ||||||
| Don´t know | 1(1.8) | ||||||
| Do you find it difficult to feed due to pain or sensibility in your teeth or gums? | Yes | 11(19.6) | 0.23 | 0.84 | 0.50 | 0.533 | 0.674 |
| No | 45(80.4) | ||||||
| Don´t know | 0(0) | ||||||
| During the past three months, have you noticed a tooth that does not look right? | Yes | 4(7.1) | 0.06 | 0.92 | 0.45 | 0.492 | 0.921 |
| No | 52(92.9) | ||||||
| Don´t know | 0(0) | ||||||
| Do your gums bleed easily? | Yes | 21(37.5) | 0.55 | 0.84 | 0.68 | 0.694 | 0.013 |
| No | 35(62.5) | ||||||
| Don´t know | 0(0) |
SS: Sensitivity; SP: Specificity; ACC: Accuracy; ROC curve: Receiver Operating Characteristic.
Clinical data of participants.
| Index | Means (SD) | Median (min–max) |
|---|---|---|
| DMFT | 5.23 (5.94) | 4 (0–28) |
| VPI (% of sites) | 31.36 (28.08) | 23.10 (0–100) |
| GBI (% of sites) | 33.77 (25.98) | 26.92 (0–100) |
| Classification | Parameter | Participants (%) |
| Acceptable | GBI ≤ 25% | 25 (44.6%) |
| Unacceptable | GBI > 25% | 31 (55.4%) |
DMFT: Decayed, Missing, and Filled Teeth; VPI: Visible Plaque Index; GBI: Gingival Bleeding Iex.
The answers of self-reported questions were compared with the clinical condition evaluated. A statistically significant relationship was found among the participants who reported that their gums bleed easily and those with the highest GBI percentage (p = 0.014). As expected, the highest values of DMFT were expressed by the individuals who reported previous dental treatments (p = 0.031). Regarding the presence of decayed teeth, there was a statistically significant relationship between the participants who classified their oral health as unsatisfactory (fair/poor) and the presence of untreated lesions (p = 0.03). There was no statistical difference between platelet levels and GBI (p = 0.773) or self-reported gingival bleeding (p = 0.678).
The diagnostic tests were performed for each question in relation to the GBI and are detailed in Table 2. The only question in the questionnaire that correctly assessed the status of periodontal health was “Do your gums bleed easily?” (p = 0.013).
DiscussionOral self-assessment is considered an important preventive measure in the context of limited resources or time to perform a complete clinical examination.17 In hematological diseases, oral and gingival bleeding are common signs, frequently interpreted as a consequence of the underlying disease, instead of a bacterial dental biofilm-derived condition. In a primary or tertiary medical consultation, physicians and other non-oral health professionals tend to overlook the oral clinical examination.18 However, some questions in the interview may raise professional attention to underestimated clinical problems that can affect life quality and even negatively affect the overall treatment of the patient.
The National Fanconi Anemia Meeting is hosted every two years in the city of Curitiba, Paraná, Brazil. The patients come from all 5 regions of the country and the event aims to disseminate information about the disease to affected individuals and their families through lectures and activities provided by specialized professionals. In view of the overlooking of oral health in relation to other FA patient demands, efforts to increase the prevention of oral diseases must be made, mainly regarding self-perception of oral lesions.19
A study comparing the ability on mouth self-examination (MSE) of individuals with FA to the professional examination aimed to establish a technique for the secondary prevention of oral cancer in this population. The MSE is an example of a low-cost and non-invasive procedure for the detection of suspicious lesions, which could facilitate early detection of oral malignancies.19 Similarly, the prevention of periodontal disease in individuals with FA would be facilitated by self-report measures of periodontal status, favoring earlier diagnosis and treatment in initial stages of the disease.
Furthermore, self-reports are an alternative to estimate the prevalence of periodontal disease when a complete clinical examination is not possible20 and efforts have been made to validate this model in Brazil.17,21 In the context of the National Fanconi Anemia Meeting (many individuals, no dental chair and short time) this represents a great opportunity to evaluate the oral condition of a representative sample of FA patients. Considering that in the present study the majority of participants presented unsatisfactory clinical conditions related to gingival inflammation, it is important to know if it is compatible with their self-perception to adopt strategies of oral hygiene support and dental care.
Regarding the questionnaire, respondents who answered “Yes” to the question “Do your gums bleed easily?” presented a higher percentage of GBI. This was the only question that achieved “good validity”, that is considered when the sum of sensitivity plus specificity is 120% or above,12 reaching 139% in our questionnaire. Similarly, other studies found higher sensitivity and predictive values of questionnaires when adding questions about gingival bleeding.22–25 Moreover, an improvement in the predictive power of questionnaires has been observed when combining information of patients, such as age, smoking or previously “dentist-diagnosed”.17,26–28 However, in the present study the young age and low prevalence of smokers made this analysis infeasible.
The self-report questions reproduced in previous studies, as well as in the present one, had greater specificity than sensitivity, indicating a better ability to correctly identify the healthy individuals.12,13 Furthermore, the patient's perception of health is typically higher than the perception of the disease.17 Therefore, in situations in which there is a need to perform the evaluation of large groups quickly and with low cost, the questionnaire could be used to exclude healthy individuals from the need to undergo the periodontal clinical examination.26
Subjects with FA have concerns about several inherent conditions of the disease and risk of malignancies, which could divert the attention of oral health. Studies with hematopoietic stem cell transplantation candidates attributed the misguided self-perception of oral health to the worries about treatment success and death.18,29 As in the present study, patients with worse clinical condition were not able to perceive their oral health as poor.30 In addition, those who recognize their status as unsatisfactory had a statistical relationship with the presence of caries, but there was no association with gingival inflammation. This may mean that the poor condition of the teeth attracted more attention from the participants than the health of the gums. This outlook refutes the proposition that individuals who confront more disease might be more aware of their periodontal status 12 and reinforces the significance of prevention strategies.
In this context, children with FA could achieve lower accuracy in self-reported questions about periodontal health than the general population of the same age. Systematic reviews analyzed studies about the validity of self-reported periodontal disease among different age ranges but were not capable of establishing the effect of age on the accuracy of the instruments proposed.12,13 In the present study, despite a broad age range, considering the rarity of the FA, the hypothesis that individuals with advanced age may better identify periodontal diseases because of the higher severity of the disease could not be confirmed since there was no statistical difference between age and periodontal status.
There was no association between a lower count of platelets and higher levels of GBI, neither of higher perception of gingival bleeding reported by patients. These results are in conformity with findings of a study with candidates for allogeneic hematopoietic stem cell transplantation (HSCT), in which gingival bleeding was associated with the presence of visible plaque and not to the hematologic status.30
Although being a significant sample of a group of individuals with a rare disease, the small number of participants in this study could represent a limitation for statistical analysis. Moreover, the periodontal condition of the participants may have been overestimated, as measurements of probing depth, clinical attachment level and gingival recession were not performed.
ConclusionIndividuals with FA were capable of perceiving gingival inflammation manifested by gingival bleeding.
Conflicts of interestThe authors declare no conflicts of interest.