The authors report a case of Pyoderma gangrenosum (PG) with some clinical features mimicking PAPA (Pyogenic Arthritis, Pyoderma gangrenosum and Acne) syndrome, indicating a myelodysplastic syndrome (MDS). During the course of MDS, lesions of another neutrophilic dermatosis, erythema elevatum diutinum (EED), emerged.
PG and EED are uncommon neutrophilic dermatoses of unknown etiology and their pathogenesis is poorly understood. In a recent review, up to 50% of PG cases are associated with an underlying systemic disease such as inflammatory bowel disease, rheumatoid arthritis or hematologic disorder.1 Among them, acute myeloid leukemia (AML) is found in 7% of the cases.1,2 Furthermore, EED has been associated with these conditions.2
On the other hand, extracutaneous manifestations of neutrophilic dermatosis are rare. Just a few reports describe PG with involvement of the lungs, joints, liver, spleen, bone or blood vessels.3
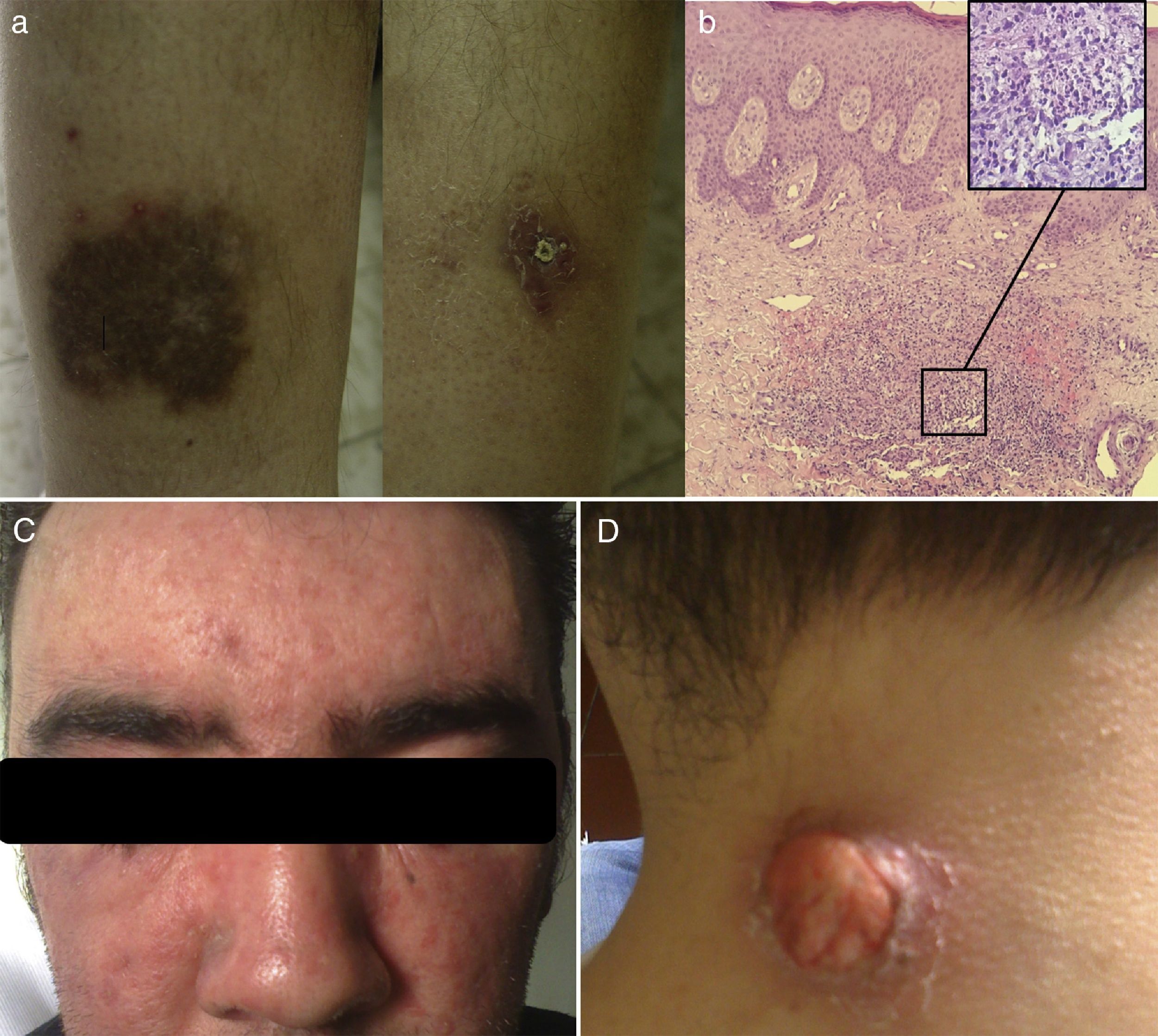
Case reportA 24-year-old man was referred in 2004 due to bilateral leg pustulosis lasting for two months with the lesions surrounded by dusky erythematous-violaceous halos. These lesions evolved to ulcers and cribriform scars (Figure 1a). Histopathology revealed a dense neutrophilic infiltration of the dermis, consistent with PG (Figure 1b). Since 2000, the patient had developed a lymphocytic interstitial pneumonitis and Evans syndrome (hemoglobin: 10.7g/dL; reticulocytes: 9.8%; platelets: 33×109/L; lactate dehydrogenase: 475IU/L; positive direct Coombs test), which were interpreted together as extracutaneous manifestations of PG.
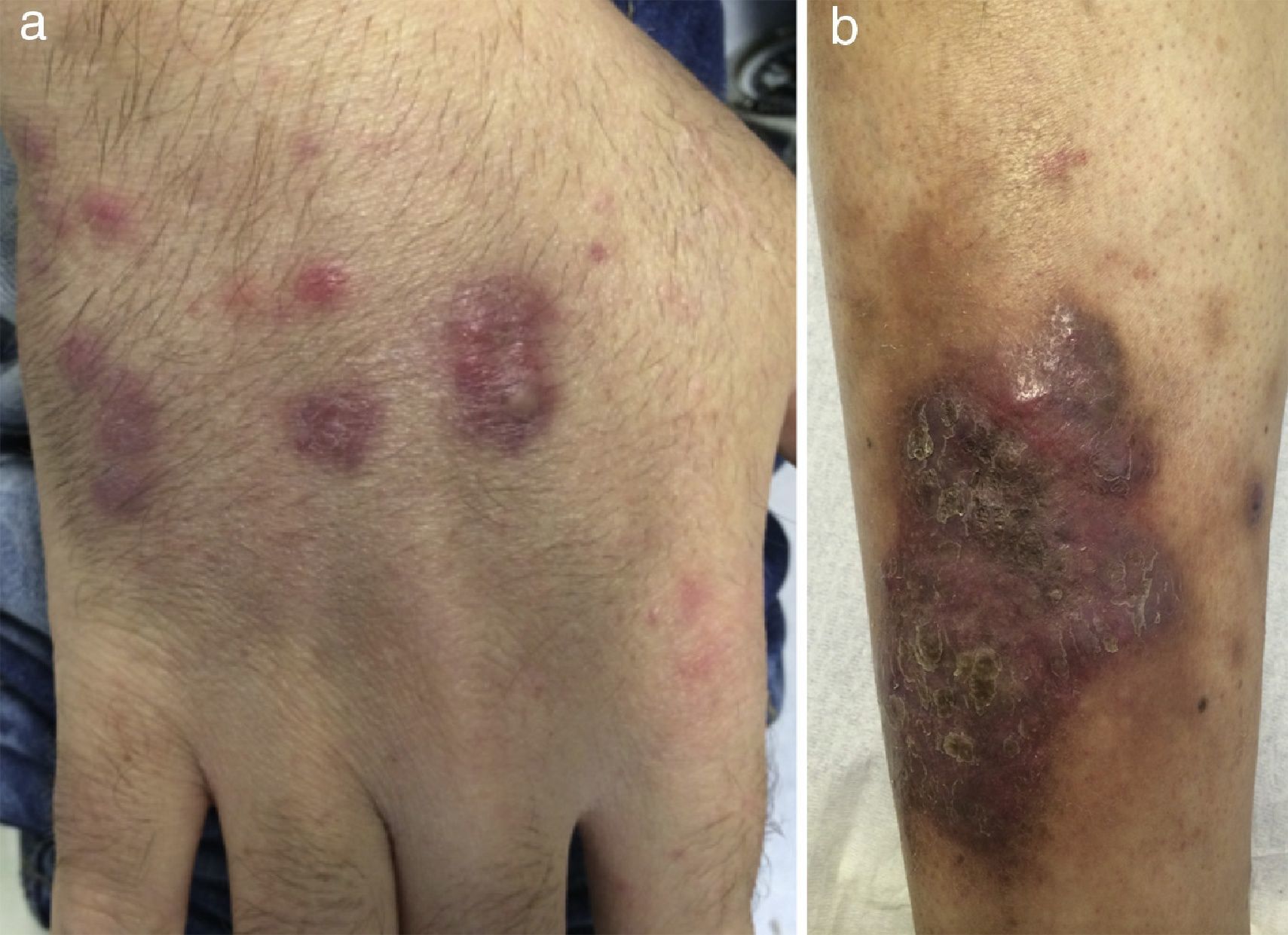
In 2007, new cutaneous features of extensive acneiform lesions appeared on the face resulting in a leonine appearance (Figure 1c) with new PG lesions (Figure 1d) and the onset of arthritis, which raised the suspicion of PAPA Syndrome. However, this was discarded because a molecular analysis of the PSTPIP1 gene revealed no mutations. In the same year, due to the worsening of cytopenias, a bone marrow biopsy was performed, with no diagnostic changes identified. The patient went on high-dose corticotherapy and intravenous immunoglobulin. In 2012, due to worsening of the cytopenias (hemoglobin: 7.0g/dL; mean corpuscular volume: 105fL; leucocytes: 5.02×103/μL; platelets: 23×109/L) under a prednisolone dose of 20mg/day, the bone marrow was evaluated again. A diagnosis of MDS classified as refractory cytopenia with multilineage dysplasia was made considering the bone marrow smear with multilineage dysplasia, blast count of 2% and normal karyotype of bone marrow nucleated cells. Considering the previous diagnosis of Evans syndrome, and the reduction in hemoglobin and platelet count under prednisolone, the patient was treated with splenectomy in October 2012. After the procedure, the blood counts improved and the prednisolone was suspended in May of 2013. The histology reported a spleen of 420 grams with no remarkable pathologic aspects. After six months without corticotherapy, in November 2013, he again presented with cytopenias (hemoglobin: 5.0g/dL; leucocytes: 8.42×103/μL; platelets: 13×109/L), which led to another evaluation of the bone marrow. A diagnosis of type II refractory anemia with excess blasts was made based on a blast count of 13% by morphology with immunophenotyping detecting 16% of myeloid blasts positive for CD34, CD33, CD13, CD117 and CD123, and a clonal evolution with 46,XY,del(12)(p12)[17]/46,XY[13] in a previous normal bone marrow karyotype. The bone marrow histology was concordant with this diagnosis. The Hematology Department decided to perform intensive induction chemotherapy and a donor search for allogeneic hematopoietic stem cell transplantation, which was not successful. After chemotherapy induction, the patient never presented hematological recovery and the bone marrow biopsy showed hypoplasia and no excess of blasts. During the aplasia period, PG lesions showed improvement. The patient was kept in best supportive care with transfusional support until June 2014, when progression to overt AML was documented with the reappearance of blasts in peripheral blood, bone marrow smear with a blasts count of 34% and karyotype with the previous reported cytogenetic alteration. Simultaneously to AML progression, new cutaneous lesions emerged on the back of his hands and on his right leg. They were nodular and erythematous consistent with EED (Figure 2), a diagnosis further supported by histology. Another unrelated donor search was requested and the patient started treatment with 5-azacitidine. At the end of the second cycle, there was no hematological response. At the end of the fourth cycle, the patient continued with no hematological response and the bone marrow evaluation showed a blast count of 14%. During this period, the patient had multiple infections with progressive deterioration of performance status, culminating in his death in January 2015 with pneumonia and AML refractory to intensive chemotherapy induction and 5-azacitidine.
DiscussionMDS are clonal hematologic disorders characterized by ineffective hematopoiesis and risk of transformation to AML. Up to about 30% can be associated with several autoimmune manifestations, which portends a poor prognosis.4 Apart from the known genetic and epigenetic mechanisms involved in ineffective hematopoiesis and clonal evolution to AML, immune mechanisms with bone marrow microenvironment inflammatory dysregulation and aberrant signaling of innate immune pathways, might be involved in MDS.5 There is also evidence that subtypes of MDS have high numbers of pro-inflammatory T helper-17 cells and regulatory T cells.6 The release of pro-inflammatory cytokines, such as tumor necrosis factor alpha and interferon-gamma, in autoimmune diseases could be a mechanism of damage directed at hematopoietic stem cells and erythroid and myeloid progenitor cells, explaining cytopenias and clonal evolution.6 Summing up this evidence, raises the hypothesis of a pathogenic interaction between MDS and autoimmune diseases. Several types of neutrophilic dermatoses have been described in association with MDS7 and it is interesting to observe recurrent bone marrow cytogenetic alterations, frequently observed in MDS, in cases of neutrophilic dermatoses.8 The pathogenic relationship between PG and hematologic disorders remains unclear, though multiple theories have been proposed. Similar to other autoimmune disorders, a common ‘trigger’ could damage the hematopoietic cells and impose cutaneous involvement by autoimmune phenomena. Otherwise, the immune system dysregulation observed in MDS, might be responsible for the production of autoantibodies against cutaneous antigens with perivascular immune complex deposition.3 Furthermore, only in very few reports, patients developed more than one type, as occurred in this patient with PG and EED.9 In this report, a transient improvement of the PG lesions was observed during aplasia after intensive chemotherapy and an outbreak of new lesions consistent with EED when the blood and blasts counts started to increase again. This phenomenon is in line with the hypothesis of a link between the pathogenesis of neutrophilic dermatoses and MDS. There are reports of improvements of neutrophilic dermatoses and other autoimmune diseases, with the institution of therapy directed at MDS, particularly 5-azacitidine.10 The success of this therapeutic approach seems to be linked with improvements of the hematologic disease. The absence of hematological and cytogenetic response to 5-azacitidine, and consequently the progression of the AML, could explain the appearance of another neutrophilic dermatosis (EED) portending a poor prognosis.
This case emphasizes that the investigation of longstanding cytopenias associated to neutrophilic dermatosis, such as PG, is of paramount importance to rule out an underlying MDS. The early recognition of this entity might have implications on the outcome, considering that the ideal treatment for PG can be the same as for the MDS, in cases where these entities coexist.
Conflicts of interestThe authors declare no conflicts of interest.