The D antigen is the most immunogenic, next to the ABO blood group system. The purpose of D typing is to provide D negative units to negative recipients and avoid inadvertent D positive transfusions. The RhD and RhCE genes are located on chromosome 1 (p34–36). The RhD gene is highly polymorphic and contains more than 460 alleles.1 The D antigen encoded by the RhD gene has extracellular, transmembrane and intracellular regions. Mutations in the RhD gene may result in amino acid alterations in the D protein structural regions and the resulting phenotype is known as the D variant.2 Serologically, one can suspect a D variant under the following circumstances: using conventional method, red cells giving a ≤2+ reaction, in direct typing and a positive Indirect antiglobulin test (IAT) with IgG anti-D,2 a discrepancy between the two methods, variable reactions with different antisera, a discrepancy between the current and previous lab reports, and a D positive individual forming anti-D.3 Molecular studies have characterized the D antigen into Weak D, Partial D, Weak Partial D, and Del. Weak D individuals possess all D epitopes, however, there is a quantitative reduction especially in weak D types 1, 2, 3. Hence, these individuals do not form anti-D. They are usually overlooked during direct typing and need IAT to be detected. The majority of the weak phenotypes result from missense mutations and rarely due to the position effect.1 The D antigen is weakly expressed due to the impact of the C antigen in the trans position (Dce/dCe). During the era of polyclonal anti-D, these D variants had been identified as weak D. Over the years, the introduction of monoclonal antisera has resulted in D typing discrepancies.3 Partial D individuals may not have one or a few epitopes (qualitative reduction) and are generally typed as D positive. These individuals are typed as D negative only if the specificity of the monoclonal antisera is directed against the missing epitope. Hence, they are prone to alloimmunization against the missing epitopes (especially partial D, category 6 (DVI)). Partial D phenotypes arise chiefly due to missense mutations or gene conversion.4 Recently, the International Society of Blood Transfusion (ISBT) has included the Weak Partial variant, which describes weak D variants with qualitative changes in the epitopes, making them prone to D alloimmunization. These include weak D types 4.2, 11, 15 and 21.5 The D antigen sites per red cell for wild-type and variants have been enumerated using flow cytometry for the Indian population. The D antigen sites on the wild-type have been observed to be in the range of 7860–34,160. Weak D cases were observed to carry 1500–7500 D antigen sites. Partial D variants (DV, DIVa) displayed a mean antigen concentration of approximately 10,000 per red cell, with an exception of the DVI bearing a mean of 3175 D antigen sites.6 The DEL is a rare variant which is detected by adsorption elution tests/molecular tests. The prevalence of serological weak D worldwide has been estimated to range from 0.0 to 3.0%.2 There is no data with respect to the incidence of D variants in the South Indian population. In this study, I aimed to: (1) estimate the prevalence of serological weak D in our population; (2) compare the results of initial D typing results yielded by the conventional tube technique (CTT) and gel techniques, and; (3) implement a protocol in the identification of weak D cases at our institution.
This retrospective study was undertaken in the Department of Transfusion Medicine, Kovai Medical Center and Hospital, Coimbatore, India. The Directorate General of Health Services (DGHS), Ministry of Health and Family Welfare, Government of India recommends that D typing be performed with (1) two different antisera from two different manufacturers or different batches from the same manufacturer, or; (2) a blend of monoclonal IgM and IgG anti-D or monoclonal IgM and polyclonal (human) IgG anti-D can be used to detect weak D.7 During the study period (Jan. 2016 to May 2018), a total of 27,563 donor samples were subjected to ABO blood grouping and RhD typing, as per the recommendations provided by the DGHS. The D typing was done using a gel card, as per the manufacturer's instructions (Diaclon ABO/D+ Reverse grouping, IgM Monoclonal anti-D, Clones LHM 59/20 and LDM3+175-2, Biorad, Cressier, Switzerland). Simultaneously, all the samples were tested for D typing using the conventional tube technique (CTT) at saline phase, employing anti-D (Eryclone, IgM monoclonal anti-D, Clone P3x61, Tulip diagnostics, Goa, India). Appropriate controls were used. Those samples showing a reaction of ≤2+ were subjected to weak D testing using the LISS/Coombs gel card (Bio-rad, Cressier, Switzerland). A volume of 50μL of 0.8% red cell suspension was added in the reaction chamber, followed by the addition of 25μL of anti-D (Rhofinal, IgM+IgG monoclonal anti-D, Clone P3×61+MCAD6, Tulip diagnostics, Goa, India). The direct antiglobulin test (DAT) was performed on samples tested using the LISS/Coombs gel card (polyspecific anti-IgG+C3d, Biorad, Cressier, Switzerland). The DAT positive samples were excluded from the study as they can result in false positive reactions. The anti-D antisera used in this study for D typing did not detect partial D category VI (DVI). Statistical analysis was done using the Graph Pad Prism software version 7. The statistical difference between the mean values of the agglutination scores of the two methods (tube and gel techniques) was calculated using the paired t-test. Sensitivity, specificity, positive predictive value and negative predictive value of the gel technique were also calculated, considering the CTT as the “gold standard” technique. Spearman's correlation coefficient was used to calculate the strength of association between the two techniques. The κ (Cohen's Kappa) value was calculated to measure the agreement between the two methods. At a p-value of <0.05, differences were considered statistically significant.
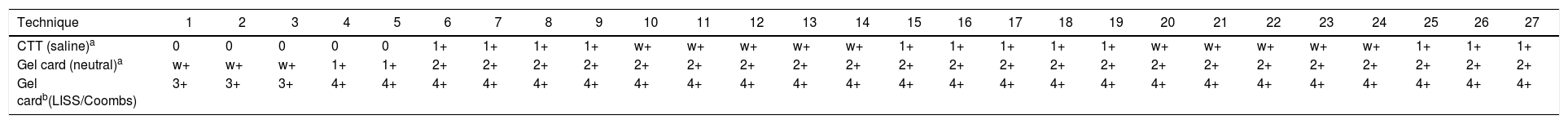
Of 27,563 donors tested, 25,984 donors (94.27%) and 1552 donors (5.63%) were typed as RhD positive and RhD negative, respectively, using both the gel and tube methods (concordance=99.98%, κ=0.99). There was a significant positive correlation between the two techniques (Spearman's correlation coefficient, Rho=0.60, p<0.0009). A total of 22 samples were typed as weak positive (a grade of agglutination ranging from weak positive to 2+) with anti-D using both the techniques. A discrepancy was observed in 5 samples. These were typed as D negative by CTT and D positive by the gel technique. All of the 27 samples tested positive in confirmatory weak D testing. In our study, prevalence for weak D was 0.097% (27 samples out of 27,563 donor samples). Serological characteristics of each case have been described in Table 1. Agglutination scores derived using the gel technique were significantly higher than the agglutination scores derived using the CTT (p<0.001). For D typing, sensitivity, specificity, positive predictive value and negative predictive value of the gel technique were calculated as 100%, 99.68%, 99.98% and 100%, respectively, when compared to the CTT.
Serological characteristics of the weak D samples detected in the present study.
| Technique | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CTT (saline)a | 0 | 0 | 0 | 0 | 0 | 1+ | 1+ | 1+ | 1+ | w+ | w+ | w+ | w+ | w+ | 1+ | 1+ | 1+ | 1+ | 1+ | w+ | w+ | w+ | w+ | w+ | 1+ | 1+ | 1+ |
| Gel card (neutral)a | w+ | w+ | w+ | 1+ | 1+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ | 2+ |
| Gel cardb(LISS/Coombs) | 3+ | 3+ | 3+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ |
CTT - conventional tube technique; LISS - low ionic strength solution.
In India, the prevalence of weak D is estimated to range approximately from 0.0075 to 0.2% of the total donor population from different geographic distributions.8 The prevalence of weak D in the current study was 0.097%. The RhD typing discrepancies are attributed to multiple factors, such as different methods (tube, gel, microplate) used for typing, different phases of testing (saline or Coombs’ phase), different avidity and specificities of monoclonal antisera and diversified RhD alleles with varied phenotypic expression.9 Studies from India have included only RhD negative donor samples for weak D testing. There is no mention of the samples showing weak reactivity, which leads to underreporting of the phenotype prevalence. Because of these reasons, true incidence of weak D is difficult to estimate in the Indian population. Our study shows that the gel technique is a better technique for CTT with good sensitivity and specificity for D typing with good concordance. A total of 5 samples showed negative results using the CTT and positive results by the gel technique at saline phase. They were found to be weak D positive, using confirmatory testing. Our findings are in agreement with the observations made by Ono et al., in which there was a good agreement between the gel and tube techniques for D typing.10
Molecular characterization of the D variants in our population has been studied by few authors. They found that 130 out of 223 samples (58.3%) carried a novel weak D allele RhD gene with exon 3 duplication. Whole RHD gene deletion, RHD(G63C), RHD(A244V), RHD(L216F), weak D Type 8 and weak D Type 25 were among the commonly identified RHD alleles in the study population.11 On the contrary, weak D types 1, 2 and 3 are the most common weak D types found in Caucasians.2 The DFR Partial D has been found to be the most common partial D category identified in the western Indian population.12 However, these findings cannot be generalized to the Indian population as a whole due to the vast genetic heterogeneity.
According to recent reports, serologically D negative individuals have been re-classified as D variants, using molecular genotyping.13 Despite its benefits, genotyping has not been globally accepted as a routine testing platform for the following reasons: the AABB recommendations for weak D testing have been in vogue for decades worldwide; there is a lack of awareness of the cost-effectiveness of genotyping among clinicians and transfusion medicine practitioners; the Rh immunoglobulin has a better safety profile; the Rh immunoglobulin prophylaxis is not a standard recommendation for weak D, and; the risk of alloimmunization in D variant individuals after exposure to D positive red cells is yet to be studied in all geographic distributions of the world.14 In a resource-limited setting like that of India, it is not feasible to establish molecular genetic testing facilities at all blood banks. Genetic testing to detect D variants using the multiplex polymerase chain reaction (PCR), even though it has a better sensitivity than the serological tests, has a cost which outweighs the benefits at our center (the multiplex PCR is 30 times more costly than the serological test).
Based on my results, I have modified the protocol for D typing as follows: Initial RhD typing is currently being done using the gel technique, as described above. The donor samples showing a grade of agglutination of ≤2+ reaction in initial D typing are further subjected to confirmatory weak D testing using the LISS/Coombs gel card. For weak D positive samples, the DAT is performed. The DAT positive units are discarded. Such individuals are given a donor card indicating that they are RhD positive donors and RhD negative recipients. The patient samples showing a grade of agglutination of ≤2+ reaction in initial D typing are considered as RhD negative for the purpose of transfusion and RhIg prophylaxis. Conventional monoclonal anti-D antisera do not detect the partial DVI category. Kulkarni et al. suggested that the antisera (any one of the clones LHM 76/59, ESD-1 and LHM 76/55), which reacts with all D variants, can be used for donor typing, wherever feasible.3
I conclude that the serological weak D phenotype is identified by the reactivity of RBCs with an anti-D reagent, giving no or weak (≤2+) reactivity in initial testing, but a strong reaction with the anti-globulin test. The gel technique is a sensitive and cost-effective technique in the identification of weak D individuals. Prevalence of weak D would be better elucidated using the gel technique. It is also suggested that antisera with any one of the clones LHM 76/59, ESD-1 and LHM 76/55 can be included for donor typing, wherever feasible, to identify all D variants.
Conflicts of interestThe author declares no conflicts of interest.