Involvement of the peritoneum occurs very rarely and is exceptional as an exclusive extranodal presentation of lymphomas. In most cases lymphomas associated with this rare entity are high-grade ones. PL secondary to high-grade nodal lymphoma is more frequent than primary peritoneal lymphoma, and there are only a few cases of the latter described in the literature.
Description of the caseWe present the case of a patient with constitutional syndrome and imaging findings suggestive of peritoneal carcinomatosis who was finally diagnosed with a Diffuse Large B-cell Lymphoma (DLBCL) by an ultrasound-guided core needle biopsy (CNB) of peritoneum. The patient received one polychemotherapy cycle; however tumor lysis syndrome occurred with death of the patient in the following days.
This case tries to show the existence of a PL without other radiological findings of lymphoma, a fact that is very exceptionally described in the literature.
DiscussionThe differential diagnosis between PL and others peritoneum diseases such as peritoneal carcinomatosis, malignant primary peritoneal mesotheliomas, tuberculous peritonitis, sarcomatosis, diffuse peritoneal leiomyomatosis or benign splenosis, constitutes a major problem in imaging techniques.
An exhaustive analysis of the radiological characteristics as well as a clinical-analytical context allows the differential diagnosis against peritoneal carcinomatosis and the rest of the entities previously referred although the final diagnosis will always be a biopsy.
ConclusionPL usually manifests as an aggressive histological subtype of high-grade lymphomas leading to a rapid progression and deterioration of the patient. It is crucial for the radiologist and the clinician to be aware of this rare entity providing the earliest possible diagnosis and optimal treatment to prolong the patient's life.
Peritoneal lymphomatosis (PL) is characterized by a diffuse thickening of peritoneal surface with multifocal nodules and masses reminiscent of peritoneal carcinomatosis. Extensive infiltration of the peritoneum secondary to lymphomas is unusual, occurring more frequently in high-grade non-Hodgkin lymphomas (NHL), with few cases published in the literature.1,2
PL is an infrequent presentation of any type of NHL with few reviews in the literature. We present the case of a 74-year-old man who attended the emergency department for abdominal distension with ascites, diaphoresis, constitutional syndrome, and imaging findings suggestive of peritoneal carcinomatosis. However, ultrasound-guided core needle biopsy (CNB) of peritoneum diagnoses a Diffuse Large B-cell Lymphoma (DLBCL), so that the diagnosis of PL is established.
This case is illustrative of the difficulties involved in image diagnosis of this entity, which represents a challenge for the radiologist. It is necessary to be familiar with this condition for an accurate and early diagnosis which directly influences the management of the patient. This case tries to show the existence of a PL without other radiological findings of lymphoma, a fact that is very exceptionally described in the literature.1
Description of the caseA 74-year-old man with a pathological history of anticoagulated paroxysmal atrial fibrillation, ex-smoker, active drinker, tubular colon adenoma with low-grade dysplasia resected 4 years ago, and benign prostatic hypertrophy admitted for ascites and constitutional syndrome with loss of at least 20 kg in two months. Additionally, the patient reports that he has had profuse sweating for a month. On physical examination he was in very poor general condition having a cachectic appearance with loss of muscle mass, dehydration of the mucosa, signs of bleeding in the oral mucosa, absence of palpable lymphadenopathy as well as abdominal distension, although not tension ascitis, with a positive fluid wave test. The analysis highlights severe platelet decrease with mild neutrophilia, hyperuricemia, increased lactate dehydrogenase (LDH) and β2Microglobulin and negativity for carcinoembryonic antigen (CEA) and alpha-fetus protein (AFP) tumor markers.
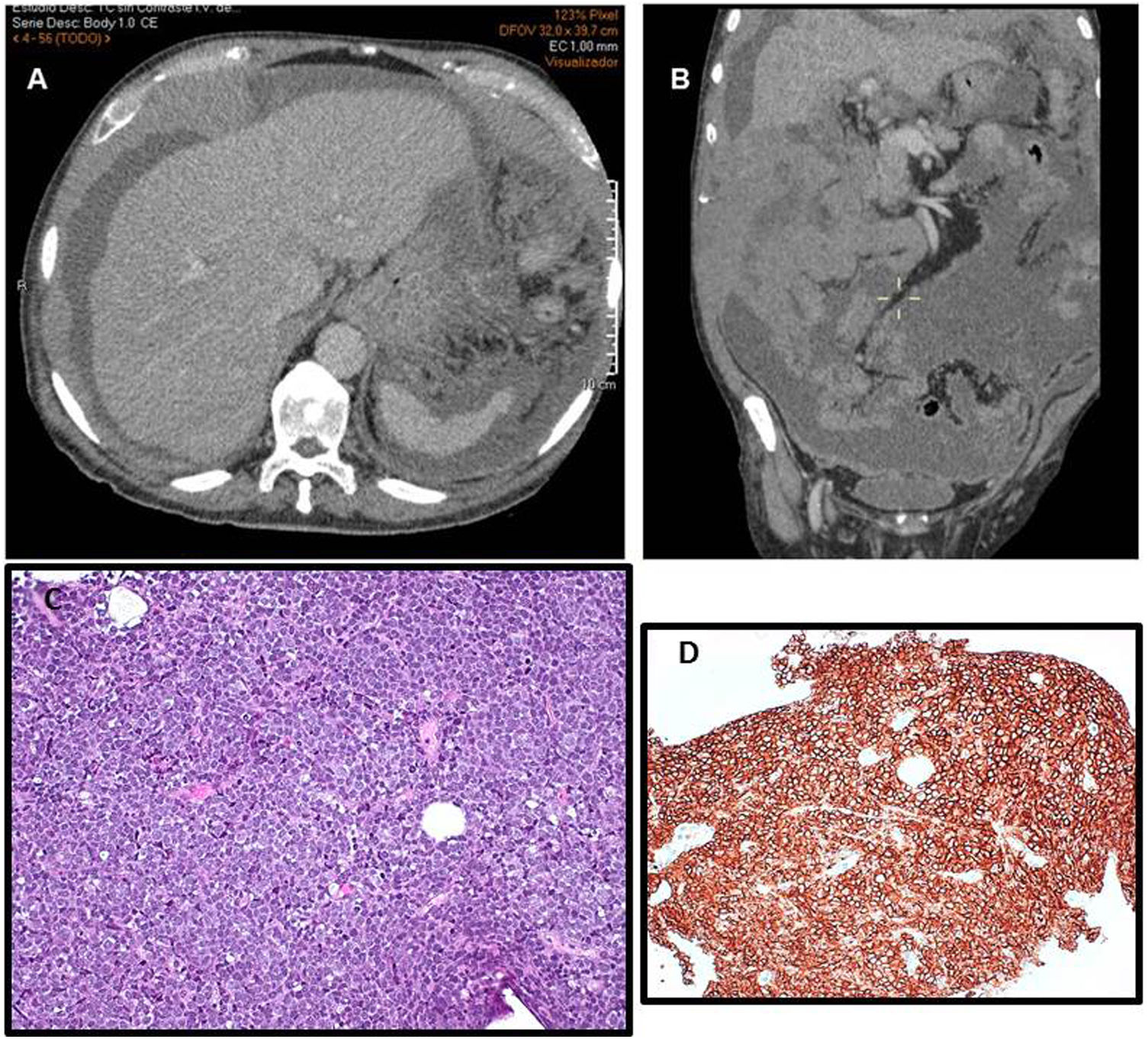
Thoracic-abdominal-pelvic computerized tomography (CT) scan with contrast shows a poorly defined hypodense focal lesion in the V-VI hepatic segment, as well as signs of chronic liver disease, an enlarged permeable portal vein (14 mm in diameter) and a normal spleen. Likewise, abundant ascites is observed with marked thickening in the lesser omentum and peritoneum, showing extensive hyperdense masses, especially on the right flank, which include the intestinal loops and mesenteric vessels suggestive of peritoneal tumor implants. Right pleural effusion is also observed (Figure 1A and B). No lymphadenopathy was observed at any level. CT findings are reported as suggestive of peritoneal carcinomatosis and possible chronic liver disease as well as liver space-occupying lesions (SOL). As the patient did not present tension ascites, the evacuating paracentesis was dismissed and the ultrasound-guided CNB of peritoneum was performed directly.
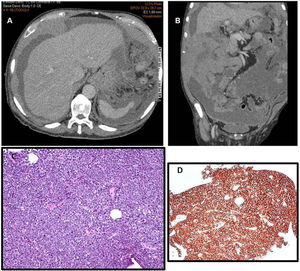
(A and B) Thoracic-abdominal-pelvic computerized tomography (CT), axial image (1A), and coronal (1B). Abundant ascites is observed with marked thickening in the lesser omentum and peritoneum. No lymphadenopathy was observed. (C) Histological confirmation of peritoneal lymphomatosis. The core-biopsy shows a diffuse monomorphic proliferation of medium and large lymphoid cells centroblastic-like (Hematoxylin–Eosin, 400×). (D) The CD20 expression by immunohistochemistry (200×).
Histological examination of the obtained samples reveals a diffuse monomorphic proliferation of medium and large lymphoid cells centroblastic-like with a positive immunophenotype for CD20, CD79a, Pax5, bcl2, bcl-6, CD10, MUM-1/IRF4 and a proliferative index with KI 67 about 70% (Figure 1C and D); and negative for CD3, cyclin D1, CD56, Chromogranin A, CK AE1/AE3 and CAM 5.2. The histological findings and the immunohistochemical profile are compatible with a DLBCL. The bone marrow extension study did not show neoplastic infiltration. Finally he was diagnosed with PL because of a DLBCL with a IV-B Ann Arbor stage and a 4 international prognostic index (IPI) (poor prognosis).
Considering the patient clinical deterioration, and since a complete diagnostic CT was already available, it was decided to start specific treatment prior to performing positron emission tomography (PET). The patient undergoes a first cycle of reduced-dose polychemotherapy (mini-CHOP schedule), due to its great fragility, with the preconceived idea of adding Rituximab in subsequent cycles. Despite the prophylactic measures adopted (hyperhydration, alkalinization as well as administration of rasburicase and allopurinol), a tumor lysis syndrome occurs with worsening kidney function and alteration in the acid-base balance with death of the patient in the following days.
DiscussionPL is usually a manifestation of an aggressive histological subtype of high-grade lymphoma that leads to rapid and progressive deterioration of the patient. Based on this premise, it is very important to stay alert to diagnose this rare entity and to establish an optimal treatment that will prolong the patient's life. Most occur in adults, although there are also cases described in children whose etiology is usually Burkitt's Lymphoma.3
The incidence of extranodal lymphoma is approximately 40%, being the most frequent location the gastrointestinal tract (5–20%). This fact generally assumes an aggravating factor in the prognosis. However, involvement of the peritoneum occurs very rarely and is exceptional as an exclusive extranodal presentation of lymphomas.4 In most cases lymphomas associated with this rare entity are high-grade ones (preferably DLBCL and Burkitt lymphoma), although some cases have also been described in lymphoblastic lymphoma and in low-grade follicular lymphoma.5,6
PL secondary to high-grade nodal lymphoma is more frequent than primary peritoneal lymphoma, and there are only a few cases of the latter described in the literature. The first bibliographic citation dates from 1986 and refers to the necropsy study of 3 patients with this pathology.2 Cytological study supposes a little value method to establish the diagnosis of this entity, being the most accurate method a laparoscopic biopsy or ultrasound-guided CNB of peritoneum or omentum.3 Lymphoma is a great radiological mimic affecting any topography of the organism although peritoneal infiltration is very rare. The differential diagnosis between PL and others peritoneum diseases constitutes a major problem in imaging techniques. PL is characterized by diffuse nodular thickening of the peritoneum with mesenteric masses with or without ascites.7 These findings are indistinguishable from peritoneal carcinomatosis that usually occurs by dissemination of primary digestive tract or gynecological (mainly ovary) tumors or by dissemination of a mucinous tumor (peritoneal pseudomyxoma). On the other hand, these findings are also frequent in other entities such as malignant primary peritoneal mesotheliomas, tuberculous peritonitis, sarcomatosis, diffuse peritoneal leiomyomatosis, and benign splenosis.8
There are certain radiological signs that support the diagnosis of PL compared to carcinomatosis. Thus, it is usual to observe more frequently in the first one the invasion of the greater omentum, profuse nodularity and pasted mesentery as well as a homogeneous peritoneum density on CT. Likewise, lymph node involvement (paraaortic, mesenteric, and retroperitoneal), the presence of bulky and confluent adenopathic masses (non-obstructive, less vascularized, and without significant necrosis) that are arranged coating the mesenteric vessels producing the "sandwich" sign; as well as splenomegaly and the existence of masses in the gastrointestinal tract (especially on the stomach and terminal ileum), would aim more to a presumed PL.1,3,9,10
An exhaustive analysis of the radiological characteristics as well as a clinical-analytical context allows the differential diagnosis against peritoneal carcinomatosis and the rest of the entities previously described although the final diagnosis will always be a biopsy.
Differential clinical-radiological characteristics between CT images of carcinomatosis, sarcomatosis and lymphomatosis have been published in the literature. This is a retrospective study of 122 patients with peritoneal disease, 22 of them with lymphomatosis. Ascites, anasarca, thickening of the peritoneum and omentum, peritoneal implants, adenopathic conglomerates, as well as splenomegaly are considered. PL stands out for the frequent involvement of the omentum and mesentery with or without involvement of the lymph nodes and spleen. Patients with peritoneal carcinomatosis more frequently have ascites, peritoneal thickening, and omentum caking, although these findings can be shared by both entities.7,10
In our case the absence of splenomegaly, mesenteric and retroperitoneal lymphadenopathy made us opt for peritoneal carcinomatosis instead of PL. Moreover the absence of involvement of the gastrointestinal tract as well as the very low frequency of this entity made it difficult to diagnose PL by image.
In several of the cases published in the literature PL prognosis was very poor because of the incoercible progression of the disease as well as the appearance of a tumor lysis syndrome when chemotherapy treatment was instituted. For this reason it is important to establish prophylactic measures against this probable complication.
In conclusion, PL usually manifests as an aggressive histological subtype of high-grade lymphomas leading to a rapid progression and deterioration of the patient. It is crucial for the radiologist and the clinician to be aware of this rare entity providing the earliest possible diagnosis and optimal treatment to prolong the patient's life. Contrary to peritoneal carcinomatosis treatment is based on systemic chemotherapy without any surgical intervention so the baseline situation of the patient at the start of treatment is crucial for its further evolution.3,10
Conflict of interestsThe authors declare no conflicts of interest.