Allogeneic Hematopoietic Stem Cell Transplantation (allo-HSCT) patients are exposed to acute and chronic nephrotoxic events (drugs, hypotension, infections, and microangiopathy). The need for hemodialysis (HD) may be associated with high mortality rates. However, the risk factors and clinical impact of HD are poorly understood.
AimTo analyze survival and risk factors associated with HD in allo-HSCT Patients and methods: single-center cohort study 185 (34 HD cases versus 151 controls) consecutive adult allo-HSCT patients from 2007-2019. We performed univariate statistical analysis, then logistic regression and competing risk regression were used to multivariate analysis. Survival was analyzed by Kaplan-Meier and Cox proportional-hazards models.
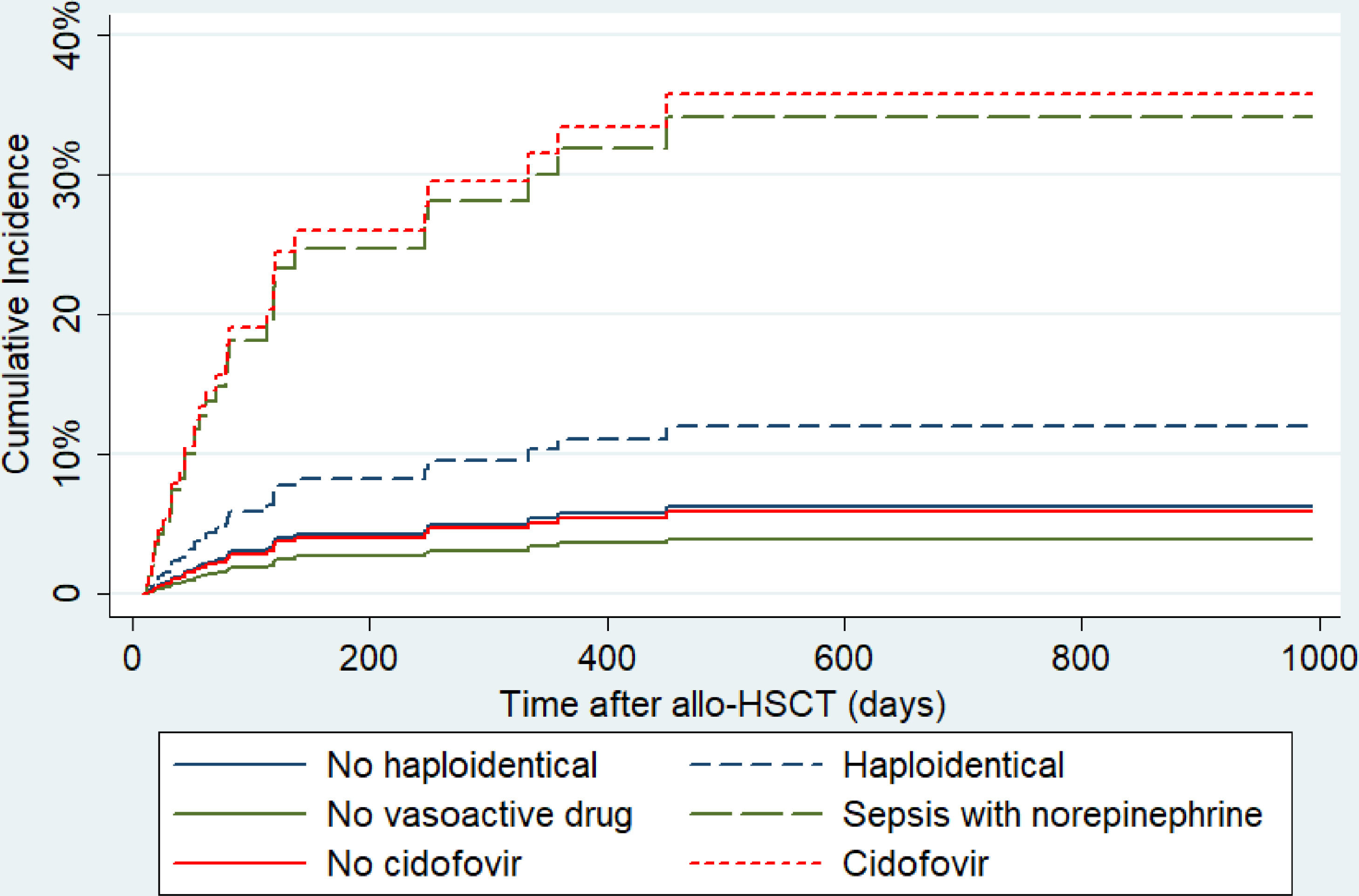
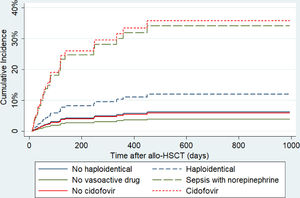
ResultsThe one-year HD cumulative incidence was 17.6%. Univariate analysis revealed that HD was significantly associated with male gender, age (p 0.056), haploidentical donor, grade II-IV acute GVHD, polymyxin B, amikacin, cidofovir, microangiopathy, septic shock (norepinephrine use) and steroid exposure. The median days of glycopeptides exposure (teicoplanin/vancomycin) was 16 (HD) versus 10 (no HD) (p 0.088). In multivariate analysis, we found: norepinephrine (hazard ratio, HR:3.3; 95% confidence interval, 95%CI:1.2-8.9; p 0.024), cidofovir drug (HR:11.0; 95%CI:4.6- 26.0; p < 0.001), haploidentical HSCT (HR:1.94; 95%CI:0.81-4.65; p 0.14) and Age (HR:1.01; 95%CI: 0.99-1.03; p 0.18) . The HD group had higher mortality rate (HR:6.68; 95% CI: 4.1-10.9; p < 0.001).
ConclusionHD was associated with decreased survival in allo-HSCT. Carefully use of nephrotoxic drugs and improving immune reconstitution could reduce severe infections (shock) and patients requiring cidofovir, which taken together may result in lower rates of HD, therefore improving survival.
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is used to treat a wide range of malignant and non-malignant diseases. Despite the overall improvement in outcomes with allo-HSCT, acute kidney injury (AKI) remains a frequent complication. It contributes to the morbidity and mortality associated with this procedure1 and, in fact, patients undergoing allo-HSCT are exposed to many acute and chronic nephrotoxic events.
Several studies describe that pre-existing kidney disease, dehydration/fluid shifts, sepsis, the use of calcineurin inhibitors (CNIs) and nephrotoxic drugs (antibiotics, contrast medium and chemotherapy) are associated with kidney injuries during the first transplantation month (D+30).1-3 Other complications indicating kidney dysfunction, such as hepatic sinusoidal obstructive syndrome (SOS), tumoral lysis and thrombotic microangiopathy (TAM), seem to be less frequent. In contrast, beyond D+30, age and other conditions can significantly contribute to AKI, such as microangiopathy, graft versus host disease (GVHD), drugs, cumulative nephrotoxic events and viral reactivations, such as BK (polyomavirus) and adenovirus.4,5
The literature addressing this topic has been focused on the cumulative incidence of AKI until D+100 following allo-HSCT, instead of analyzing the hemodialysis (HD) use incidence, which may result in higher morbidity and mortality than AKI.1,5 On the other hand, studies have shown that some drugs (such as CNI) and successive AKI events in patients following allo-HSCT may induce cumulative kidney toxicity in the long-term, which could evolve to kidney function loss and, consequently, require renal replacement therapy (RRT).1-6 Some studies have shown mortality rates of 55 to 100% in allo-HSCT patients requiring RRT.1,5
According to the RIFLE (Risk, Injury, Failure, Loss of function, End stage) criteria, the diagnosis and severity of AKIs are based on urinary volume output, serum creatinine and the duration of kidney dysfunction. The reported incidences of AKI and dialysis in the allo-HSCT setting could range from 36% to 73% and 4% to 15%, respectively.1-6 The AKI consequences can trigger positive feedback to patient deterioration caused by hypervolemia, decreased ability to fight infection and platelet dysfunction.1-5 A new kidney injury classification, defined as KDIGO (Kidney Disease: Improving Global Outcomes), has been recently established and is considered more sensitive to detect AKI7 than RIFLE. However, the KDIGO7 criteria have not been routinely assessed in allo-HSCT patients yet.
The literature addressing hemodialysis in allo-HSCT is, therefore, heterogeneous, often reporting only short-term incidences,1,2,4,5 and risk factors for this severe complication remain poorly understood. We designed a retrospective single-institution study in Brazil to investigate the one-year cumulative incidence and risk factors for hemodialysis in patients undergoing allo-HSCT. We also investigated how hemodialysis might impact on patient survival.
MethodsStudy design and participantsThis is a retrospective cohort study to identify risk factors for the need for hemodialysis among patients undergoing allo-HSCT. We reviewed the medical charts of 201 consecutive patients older than 18 years treated from January 2007 to January 2019 at a single private hospital in São Paulo, Brazil. We excluded patients from this study if they had received allo-HSCT from umbilical cord grafts and when missing data prevented adequate statistical analysis.
For this study, patients were divided into two groups: one with patients who needed to undergo hemodialysis (HD) and the other with no hemodialysis (HD-free). Variables were compared between groups in search for risk factors.
Ethics and good clinical practicesWe conducted this study following national and international resolutions, as described in the following documents: 1) ICH Harmonized Tripartite Guidelines for Good Clinical Practice, 1996; 2) Resolution CNS196/96 from the Brazilian Ministry of Health, and; 3) Helsinki Declaration. The Hospital Ethics and Research Committee approved the study protocol.
The study describes retrospective data and no interventional experiment has been conducted. Informed consent for the medical procedures had been applied to all patients. As this is a retrospective study based on medical records, no consent was obtained from patients for this study specifically. However, we ensured the anonymity of all patients and we evaluated only aggregated data.
Outcomes and variablesWe analyzed the following endpoints: overall survival (OS) and transplant-related mortality (TRM) at one year and D+100; cumulative incidence of renal replacement therapy at one year, and; cumulative incidence of relapse at one year. We also compared the following variables between the two groups: conditioning regimen; donor type; disease status; baseline creatinine clearance; type of calcineurin inhibitor (CNI); thrombotic microangiopathy (TAM); hemorrhagic cystitis; nephrotoxic drug exposure: teicoplanin/vancomycin, cidofovir, polymyxin B, amikacin or foscarnet; time of nephrotoxic drug exposure; septic shock (norepinephrine use); acute GVHD; steroid exposure; age; gender; graft source, and; overall survival (OS) at one year. We calculated the creatinine clearance using the Cockcroft-Gault equation8 and compared between groups. The nephrology team was the same across the study period and these specialists were responsible for the kidney failure diagnosis and hemodialysis indication. We registered the reason for the indication for dialysis in each case according to the medical record.
The variable steroid exposure was defined as 20mg of prednisone or equivalent for more than 14 days.1,2,5,9
Based on a previous study,9 we separated patients using the 55-year-old threshold, as the older group might experience higher toxicities rates, that indeed may occur later due to lower intensity conditioning regimens. Other age thresholds were also tested according to the non-parametric receiver operating characteristic (ROC) curve statistical analysis between age and hemodialysis.
Statistical analysisWe described the categorical variables by absolute and relative frequencies within each group and compared them by the Pearson Chi-Square test or Fisher's exact test, depending on the sample distribution. We described the continuous numerical variables as median and compared them by the Wilcoxon Mann-Whitney test (unpaired non-parametric test). In the univariate analysis, the stated significance statistical level (p) was < 0.05; however, the variables that correlated with the investigated outcomes at a p-value < 0.1 were also eligible to be included in the multivariate analysis. The Akaike information criterion (AIC) statistical method was also applied to establish which models would better fit the multivariate dataset. We analyzed the survival using the Kaplan-Meier and Cox proportional-hazards models with the log-rank to test the statistical significance level of survival data (p = 0.05 cut-off). The cumulative incidence rates of hemodialysis and relapses were established using the competing risk regression (Fine and Gray),10 while for the competing events for hemodialysis, it was death and for the TRM, it was relapse. The multivariate analysis for risk factors to hemodialysis was performed by the logistic regression and competing risk regression, which were compared by the statistician, and the better fit was reported in this study. We used the following software to analyze the data: the STATA 11 version and Statistical Package for the Social Science (SPSS).
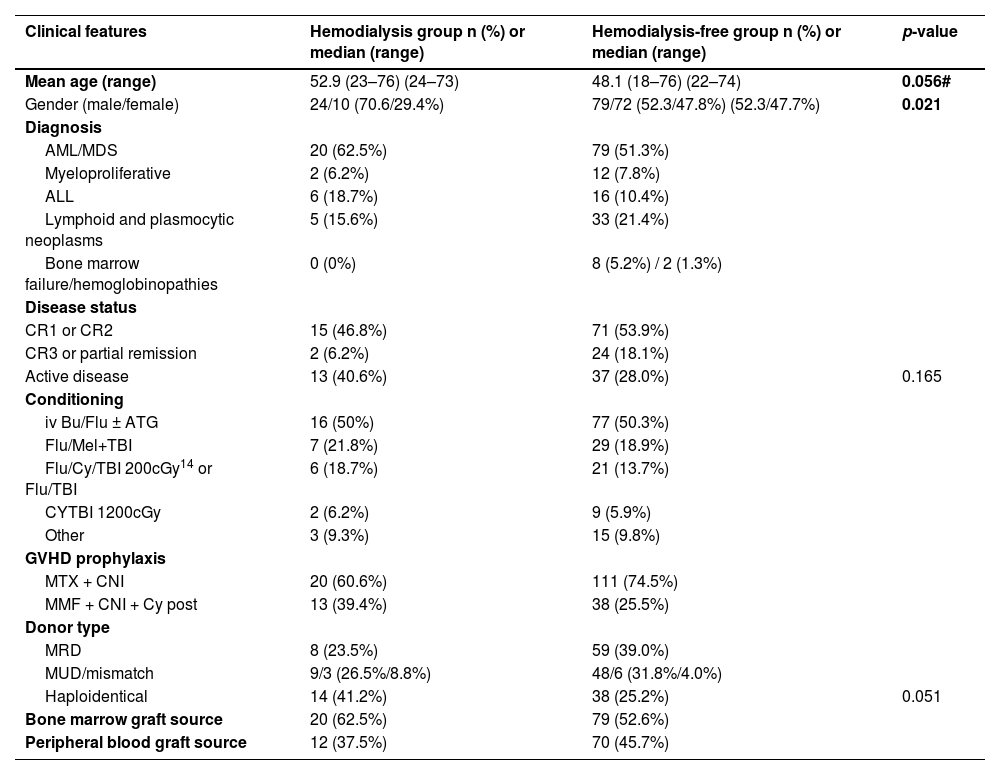
ResultsWe included a total of 185 patients undergoing allo-HSCT and their baseline clinical characteristics are shown in Table 1. Among these patients, 34 had to undergo HD during the follow-up. The one-year cumulative incidence of hemodialysis was 17.6%. In the HD-group, the median and mean time from allo-HSCT to hemodialysis were 55 and 99 days, respectively (IQ 25-75: 87 days; 95%CI: 61.6 - 137.6 days), while the time to hemodialysis ranged from 7 days (minimum) to 451 days (maximum).
Patient baseline clinical features.
| Clinical features | Hemodialysis group n (%) or median (range) | Hemodialysis-free group n (%) or median (range) | p-value |
|---|---|---|---|
| Mean age (range) | 52.9 (23–76) (24–73) | 48.1 (18–76) (22–74) | 0.056# |
| Gender (male/female) | 24/10 (70.6/29.4%) | 79/72 (52.3/47.8%) (52.3/47.7%) | 0.021 |
| Diagnosis | |||
| AML/MDS | 20 (62.5%) | 79 (51.3%) | |
| Myeloproliferative | 2 (6.2%) | 12 (7.8%) | |
| ALL | 6 (18.7%) | 16 (10.4%) | |
| Lymphoid and plasmocytic neoplasms | 5 (15.6%) | 33 (21.4%) | |
| Bone marrow failure/hemoglobinopathies | 0 (0%) | 8 (5.2%) / 2 (1.3%) | |
| Disease status | |||
| CR1 or CR2 | 15 (46.8%) | 71 (53.9%) | |
| CR3 or partial remission | 2 (6.2%) | 24 (18.1%) | |
| Active disease | 13 (40.6%) | 37 (28.0%) | 0.165 |
| Conditioning | |||
| iv Bu/Flu ± ATG | 16 (50%) | 77 (50.3%) | |
| Flu/Mel+TBI | 7 (21.8%) | 29 (18.9%) | |
| Flu/Cy/TBI 200cGy14 or Flu/TBI | 6 (18.7%) | 21 (13.7%) | |
| CYTBI 1200cGy | 2 (6.2%) | 9 (5.9%) | |
| Other | 3 (9.3%) | 15 (9.8%) | |
| GVHD prophylaxis | |||
| MTX + CNI | 20 (60.6%) | 111 (74.5%) | |
| MMF + CNI + Cy post | 13 (39.4%) | 38 (25.5%) | |
| Donor type | |||
| MRD | 8 (23.5%) | 59 (39.0%) | |
| MUD/mismatch | 9/3 (26.5%/8.8%) | 48/6 (31.8%/4.0%) | |
| Haploidentical | 14 (41.2%) | 38 (25.2%) | 0.051 |
| Bone marrow graft source | 20 (62.5%) | 79 (52.6%) | |
| Peripheral blood graft source | 12 (37.5%) | 70 (45.7%) | |
iv = intravenous; Bu = busulfan; Flu = fludarabine; Mel = melphalan; TBI = total body irradiation; CR1,2,3 = complete remission 1, 2, 3; ATG = rabbit anti-thymocyte globulin; CNI = calcineurin inhibitor; MTX = methotrexate; MMF = mycophenolate mophetil; Cy post = post-transplant cyclophosphamide; GVHD = graft versus host disease; MRD = matched related donor; MUD = matched unrelated donor. # Comparison using Student's t test.
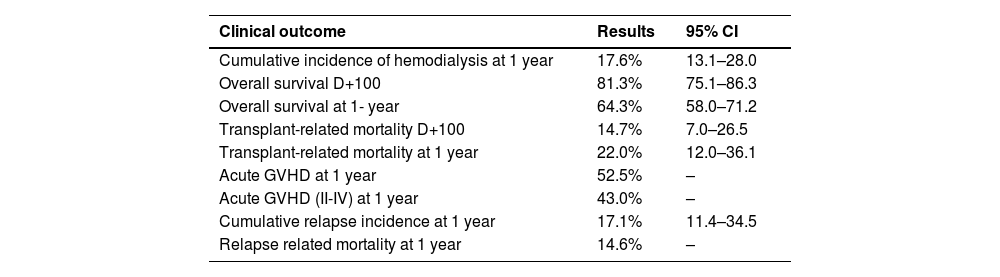
We summarize the main allo-HSCT clinical outcomes, such as survival, relapses, GVHD and transplant-related mortality (TRM), in Table 2.
Main clinical outcomes of patients undergoing transplantation (n = 185).
GVHD = graft versus host disease.
In general, the differences observed in baseline variables between the HD and HD-free groups were: haploidentical donor type (14/41.2% versus 38/25.2%; p = 0.051) and male gender 24/70.6% versus 79/52.3%; p = 0.021). Although not statistically significant, the proportion of patients with active disease status before HSCT in the HD group was superior to the HD-free group (13/40.6% versus 37/28%; p = 0.165).
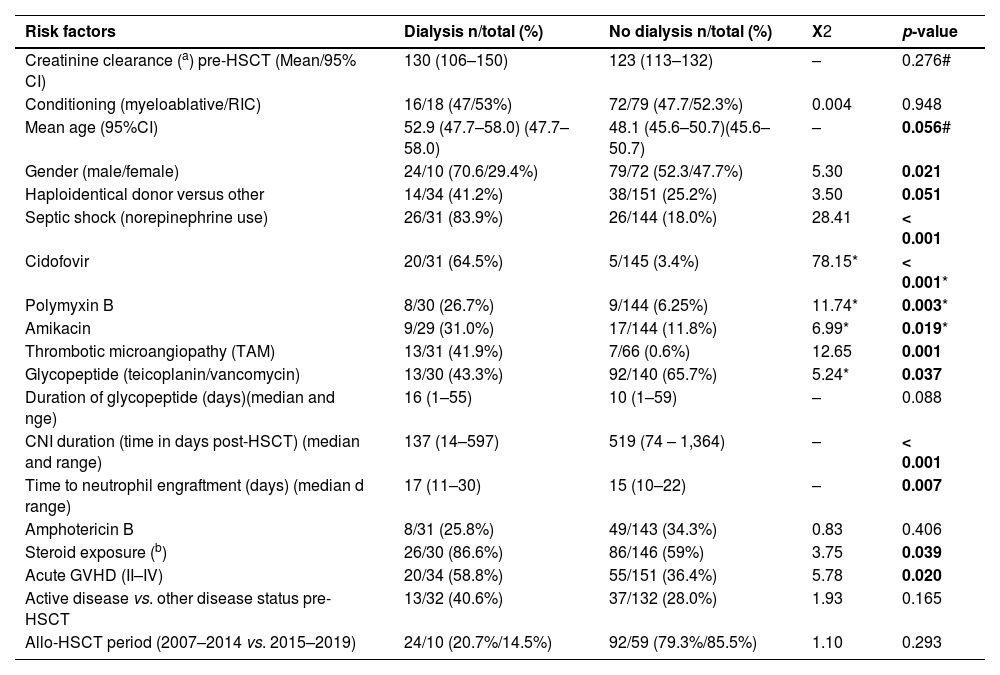
Table 3 shows the results from the univariate analysis of potential risk factors for hemodialysis. Overall, the observed frequencies of nephrotoxic drug exposure, according to each group (HD versus HD-free), were: glycopeptide (vancomycin/teicoplanin) antibiotics (13/43.3% versus 92/65.7%; p = 0.037), liposomal amphotericin B (8/25.8% versus 49/34.3%; p = 0.406), amikacin (9/31% versus 17/11.8%; p = 0.019), polymyxin B (8/26.7% versus 9/6.25%; p = 0.003), and; cidofovir (20/64.5% versus 5/3.4%; p < 0.001). Only 57 patients had available data regarding foscarnet administration following allo-HSCT and the following differences were observed between the HD (4/10; 40%) and HD-free (6/47; 12.8%; p = 0.062) groups. When analyzing the duration of each drug exposure, we found that the median calcineurin inhibitor (CNI) duration was shorter in the HD group than in the HD-free group (137 versus 519 days; p < 0.001) and that there was no statistically significant difference in glycopeptide exposure in the HD versus the HD-free groups (16 versus 10 days; p = 0.088).
Risk factors for hemodialysis, univariate analysis.
| Risk factors | Dialysis n/total (%) | No dialysis n/total (%) | X2 | p-value |
|---|---|---|---|---|
| Creatinine clearance (a) pre-HSCT (Mean/95% CI) | 130 (106–150) | 123 (113–132) | – | 0.276# |
| Conditioning (myeloablative/RIC) | 16/18 (47/53%) | 72/79 (47.7/52.3%) | 0.004 | 0.948 |
| Mean age (95%CI) | 52.9 (47.7–58.0) (47.7–58.0) | 48.1 (45.6–50.7)(45.6–50.7) | – | 0.056# |
| Gender (male/female) | 24/10 (70.6/29.4%) | 79/72 (52.3/47.7%) | 5.30 | 0.021 |
| Haploidentical donor versus other | 14/34 (41.2%) | 38/151 (25.2%) | 3.50 | 0.051 |
| Septic shock (norepinephrine use) | 26/31 (83.9%) | 26/144 (18.0%) | 28.41 | < 0.001 |
| Cidofovir | 20/31 (64.5%) | 5/145 (3.4%) | 78.15* | < 0.001* |
| Polymyxin B | 8/30 (26.7%) | 9/144 (6.25%) | 11.74* | 0.003* |
| Amikacin | 9/29 (31.0%) | 17/144 (11.8%) | 6.99* | 0.019* |
| Thrombotic microangiopathy (TAM) | 13/31 (41.9%) | 7/66 (0.6%) | 12.65 | 0.001 |
| Glycopeptide (teicoplanin/vancomycin) | 13/30 (43.3%) | 92/140 (65.7%) | 5.24* | 0.037 |
| Duration of glycopeptide (days)(median and nge) | 16 (1–55) | 10 (1–59) | – | 0.088 |
| CNI duration (time in days post-HSCT) (median and range) | 137 (14–597) | 519 (74 – 1,364) | – | < 0.001 |
| Time to neutrophil engraftment (days) (median d range) | 17 (11–30) | 15 (10–22) | – | 0.007 |
| Amphotericin B | 8/31 (25.8%) | 49/143 (34.3%) | 0.83 | 0.406 |
| Steroid exposure (b) | 26/30 (86.6%) | 86/146 (59%) | 3.75 | 0.039 |
| Acute GVHD (II–IV) | 20/34 (58.8%) | 55/151 (36.4%) | 5.78 | 0.020 |
| Active disease vs. other disease status pre-HSCT | 13/32 (40.6%) | 37/132 (28.0%) | 1.93 | 0.165 |
| Allo-HSCT period (2007–2014 vs. 2015–2019) | 24/10 (20.7%/14.5%) | 92/59 (79.3%/85.5%) | 1.10 | 0.293 |
GVHD = graft-versus-host disease; CNI = calcineurin inhibitor: HSCT = hematopoietic stem cell transplantation; RIC = reduced intensity conditioning.
After a median post-HSCT follow-up of 408 days, 29.7% (52/175) patients experienced at least one episode of sepsis, requiring the vasoactive (norepinephrine) drug due to hemodynamic instability, in which a higher proportion of septic shock was found in the HD group versus the HD-free group (26/83.9% versus 26/18.0%; p < 0.001). Addressing thrombotic microangiopathy (TAM) in 97 patients with available data, the differences found between the HD and HD-free groups were 13/43.3% versus 7/10.6% (p = 0.001). The acute GVHD grades II - IV rate (20/58.8% versus 55/36.4%; p = 0.020) and steroid exposure (26/86.6% versus 86/59%; p = 0.039) were also associated with the HD risk; the latter was also included because it could be implicated indirectly in the HD through an increased risk of severe infections. Still addressing the infection risk, the median time to neutrophil engraftment was higher in the HD group than in the HD-free group: 17 days/range: 11 to 30 versus 15 days/range 10 to 22 (p = 0.007). Moreover, in the HD group, most patients (20/58%) were neutropenic (neutrophil count < 1.0 × 109/L) at one-week before hemodialysis.
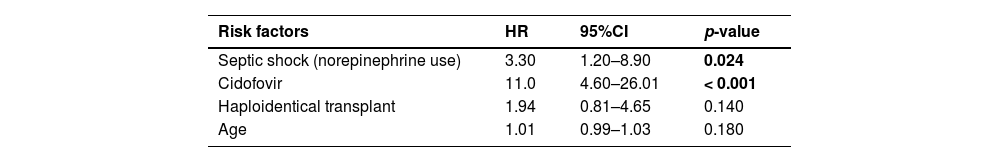
The multivariate analysis revealed that septic shock/norepinephrine (hazard ratio, HR: 3.3; 95% confidence interval, 95%CI: 1.2 - 8.9; p = 0.024) and the cidofovir drug (HR: 11.0; 95%CI: 4.6-26.0; p < 0.001) were significantly associated with an increased risk for renal replacement therapy (Table 4), all of which are also represented with the respective cumulative incidences in Figure 1. The Haploidentical HSCT (HR: 1.94; 95%CI: 0.81 - 4.65; p = 0.14) and Age (HR: 1.01; 95%CI: 0.99 - 1.03; p = 0.18) were marginally associated with a hemodialysis risk.
Multivariate analysis of risk factors for hemodialysis.
| Risk factors | HR | 95%CI | p-value |
|---|---|---|---|
| Septic shock (norepinephrine use) | 3.30 | 1.20–8.90 | 0.024 |
| Cidofovir | 11.0 | 4.60–26.01 | < 0.001 |
| Haploidentical transplant | 1.94 | 0.81–4.65 | 0.140 |
| Age | 1.01 | 0.99–1.03 | 0.180 |
HSCT = hematopoietic stem cell transplantation
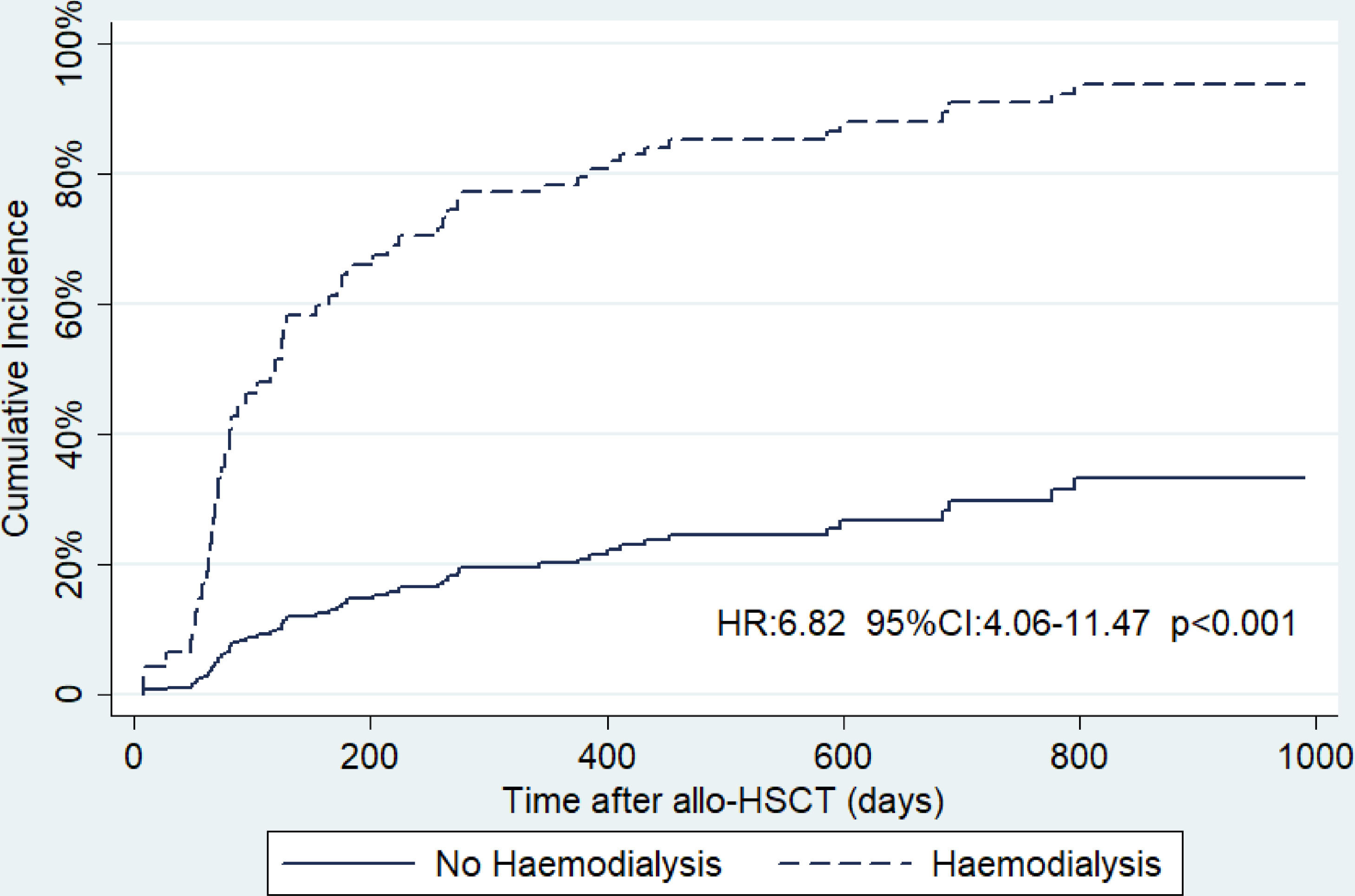
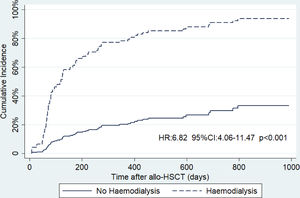
Addressing the impact of survival, according to the HD requirement, Figure 2 shows a significantly increased death risk of 6.82-fold (95%CI: 4.06-11.47; p < 0.001) in the HD group. At one year, the estimated incidence of death in the HD-free group was 21.2% (95%CI:14.8 - 29.7%), while for the HD-group, it was 75.0% (95%CI: 63.2% - 85.4%).
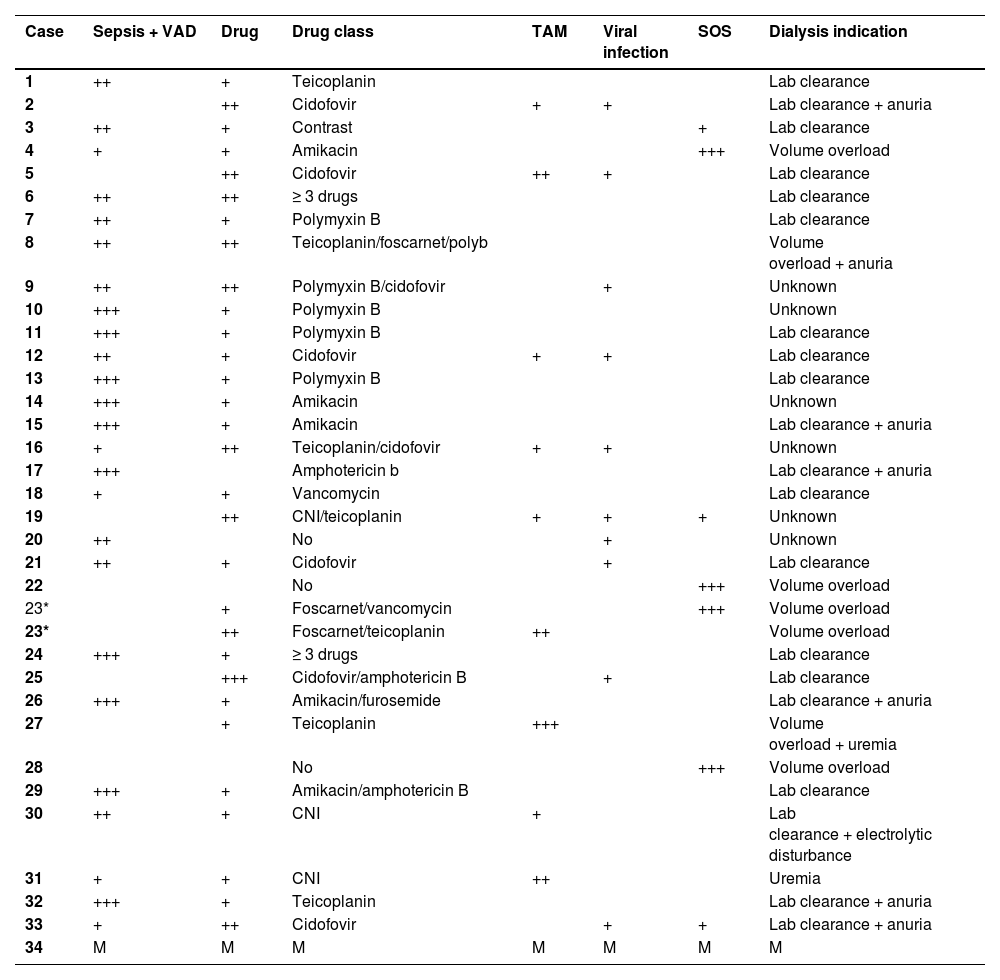
To better understand why 34 of our patients needed hemodialysis, each case was analyzed, discussed and reviewed together with nephrologists. Table 5 shows the main factors responsible for kidney failure, as well as each factor's contribution intensity in each patient, and the reasons why hemodialysis was indicated (as registered in medical charts). One case (that would be #34) was not shown in the Table due to incomplete data and inconclusive findings. We found that septic shock and cidofovir use were the leading causes of kidney failure. Additionally, some patients experienced TAM and SOS and other drugs, such as amikacin, amphotericin B, polymyxin B, foscarnet and glycopeptide, may have played a role in kidney injury. No GVHD-induced kidney lesions, such as nephrotic syndrome or immune-mediated glomerular disease, were observed.
Main causes and contributors to hemodialysis.
| Case | Sepsis + VAD | Drug | Drug class | TAM | Viral infection | SOS | Dialysis indication |
|---|---|---|---|---|---|---|---|
| 1 | ++ | + | Teicoplanin | Lab clearance | |||
| 2 | ++ | Cidofovir | + | + | Lab clearance + anuria | ||
| 3 | ++ | + | Contrast | + | Lab clearance | ||
| 4 | + | + | Amikacin | +++ | Volume overload | ||
| 5 | ++ | Cidofovir | ++ | + | Lab clearance | ||
| 6 | ++ | ++ | ≥ 3 drugs | Lab clearance | |||
| 7 | ++ | + | Polymyxin B | Lab clearance | |||
| 8 | ++ | ++ | Teicoplanin/foscarnet/polyb | Volume overload + anuria | |||
| 9 | ++ | ++ | Polymyxin B/cidofovir | + | Unknown | ||
| 10 | +++ | + | Polymyxin B | Unknown | |||
| 11 | +++ | + | Polymyxin B | Lab clearance | |||
| 12 | ++ | + | Cidofovir | + | + | Lab clearance | |
| 13 | +++ | + | Polymyxin B | Lab clearance | |||
| 14 | +++ | + | Amikacin | Unknown | |||
| 15 | +++ | + | Amikacin | Lab clearance + anuria | |||
| 16 | + | ++ | Teicoplanin/cidofovir | + | + | Unknown | |
| 17 | +++ | Amphotericin b | Lab clearance + anuria | ||||
| 18 | + | + | Vancomycin | Lab clearance | |||
| 19 | ++ | CNI/teicoplanin | + | + | + | Unknown | |
| 20 | ++ | No | + | Unknown | |||
| 21 | ++ | + | Cidofovir | + | Lab clearance | ||
| 22 | No | +++ | Volume overload | ||||
| 23* | + | Foscarnet/vancomycin | +++ | Volume overload | |||
| 23* | ++ | Foscarnet/teicoplanin | ++ | Volume overload | |||
| 24 | +++ | + | ≥ 3 drugs | Lab clearance | |||
| 25 | +++ | Cidofovir/amphotericin B | + | Lab clearance | |||
| 26 | +++ | + | Amikacin/furosemide | Lab clearance + anuria | |||
| 27 | + | Teicoplanin | +++ | Volume overload + uremia | |||
| 28 | No | +++ | Volume overload | ||||
| 29 | +++ | + | Amikacin/amphotericin B | Lab clearance | |||
| 30 | ++ | + | CNI | + | Lab clearance + electrolytic disturbance | ||
| 31 | + | + | CNI | ++ | Uremia | ||
| 32 | +++ | + | Teicoplanin | Lab clearance + anuria | |||
| 33 | + | ++ | Cidofovir | + | + | Lab clearance + anuria | |
| 34 | M | M | M | M | M | M | M |
VAD = vasoactive drug; SOS = sinusoidal obstruction syndrome; CNI = calcineurin inhibitor; TAM = transplant-associated microangiopathy; M = missing value.
Viral infection: poliomavirus or adenovirus.
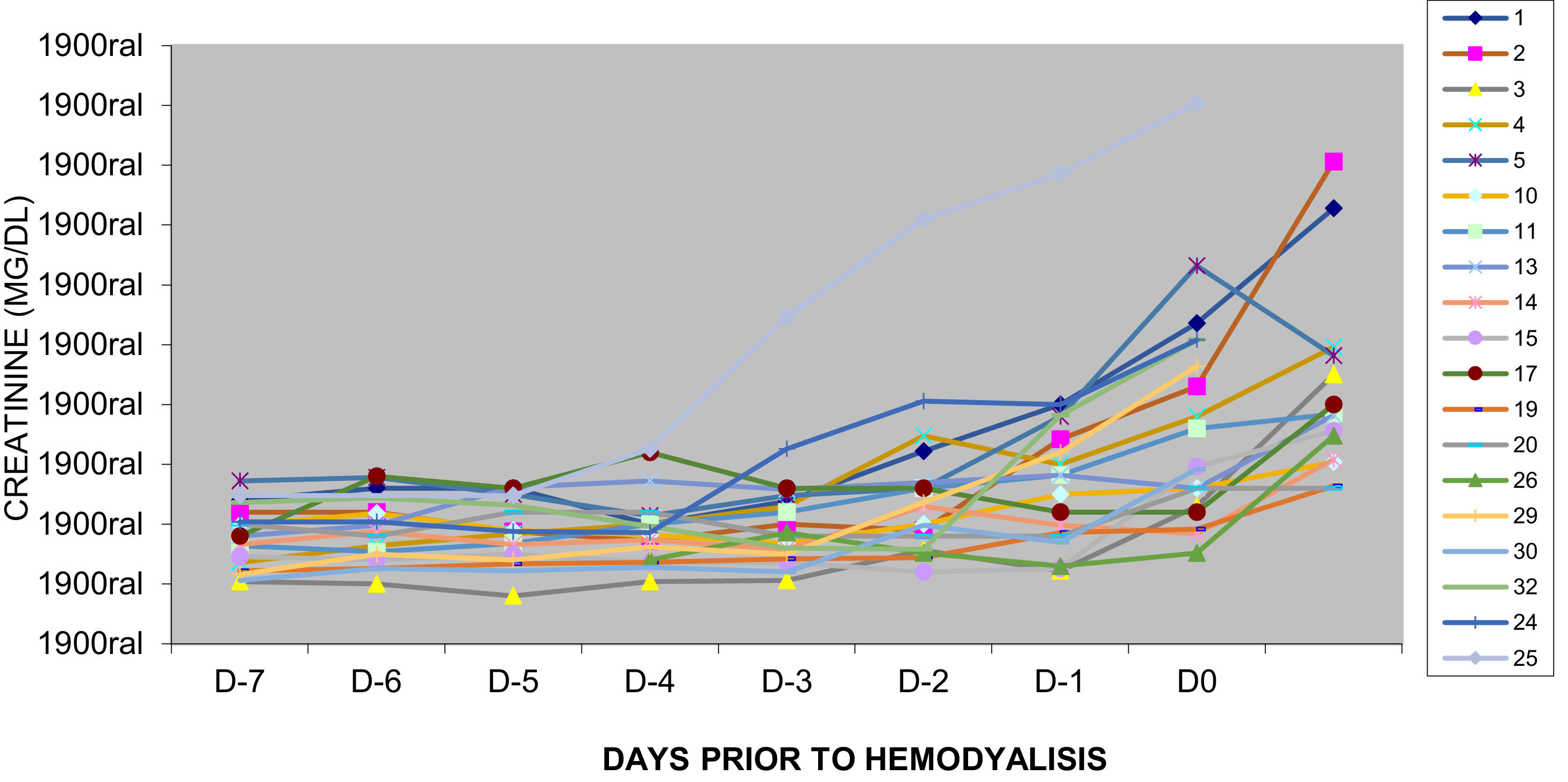
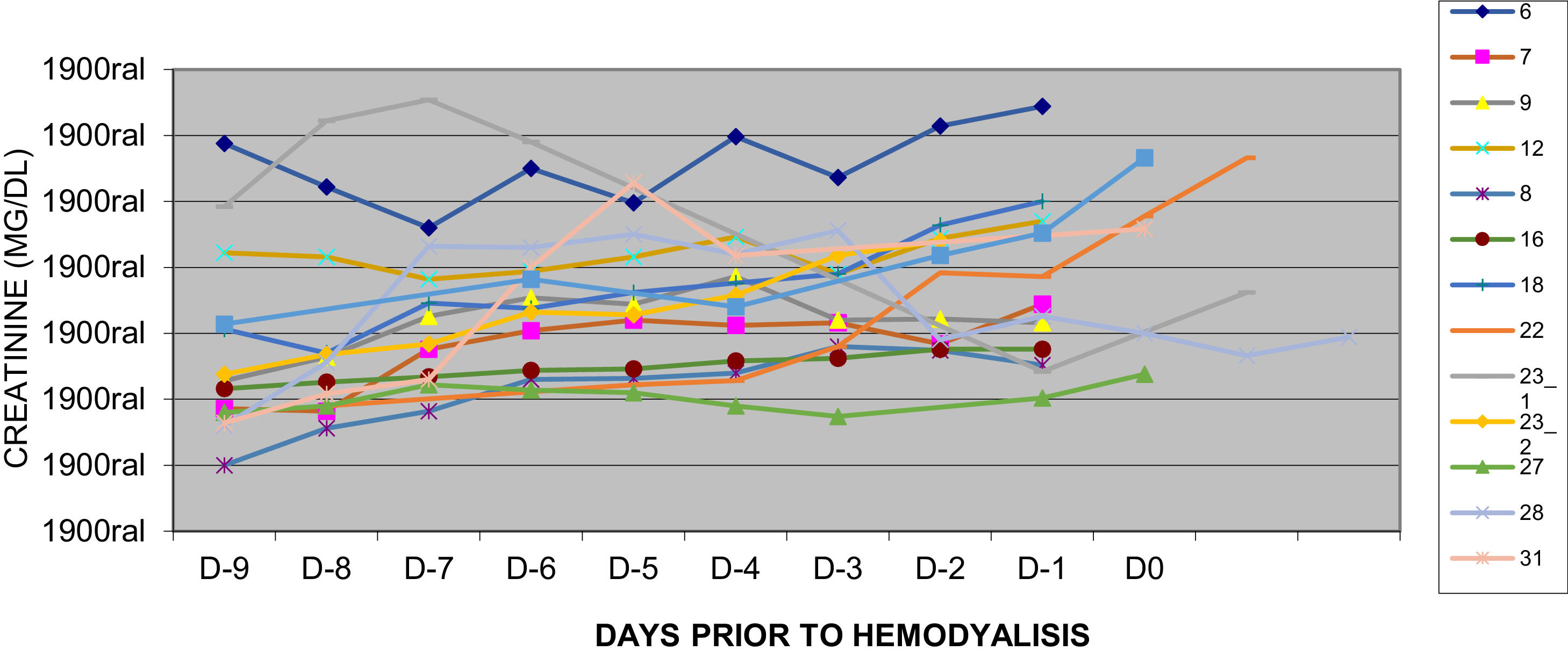
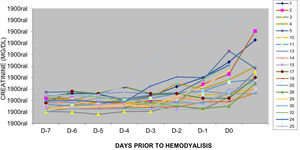
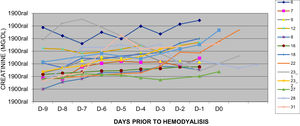
Furthermore, two different patterns of creatinine kinetics before hemodialysis were detected in patients in the HD group, as illustrated in Figures 3 and 4. Figure 3 shows a subset of patients with a relatively stable and normal creatinine, who experienced sudden/rapid increment in creatinine, usually related to an acute event, such as septic shock. In contrast, Figure 4 shows another patient subset, presenting with an already affected creatinine, who experienced floating creatinine kinetics with slower increment, probably related to cumulative or multiple events related to kidney injuries, such as drugs use, virus infection and microangiopathy.
The need for hemodialysis may have a substantial impact on allo-HSCT mortality. The literature shows that acute kidney injury is frequent in allo-HSCT, leading to high hemodialysis rates.1-3 However, the severe renal failure rates range very widely: from 4 to 49%.2 The 17.6% one-year cumulative incidence of dialysis seen in this study would be within this range cited in the literature. However, we believe that this rate is still too high and an “acceptable” rate has not been determined yet.
This unfavorable data may result from a combination of risk factors. Inappropriate or excessive indications for cidofovir use and a suboptimal approach to preventing bacterial sepsis could be the main issues.11 Moreover, because this is a cohort of patients treated in a private hospital, one could speculate that we might have faced a relatively high proportion of patients who had access to more treatment modalities and courses. Moreover, active disease status (30.5%) and haploidentical HSCT may contribute to an overestimation of the incidence of septic shock and severe viral infections. In addition, a longer duration of neutropenia and a higher proportion of acute GVHD in the HD group may play a role in the risk for infectious diseases (viral/bacterial) and thrombotic microangiopathy (TAM), as well. Indeed, an abusive administration rate (62.9%) and a prolonged use of glycopeptides (for a median time of 13 days) could be contributing to the HD risk. We believe that severe forms of hemorrhagic cystitis might have affected the kidney function of some patients, as well.
Another subset of our patients could subsequently be experiencing cumulative nephrotoxic events, as shown in Figure 4. These were also seen in one study, in which patients with early renal dysfunction, defined as a creatinine clearance < 60 ml/min up to D+90 following allo-HSCT, had increased risk (odds ratio (OR): 10) of developing a chronic kidney disease,12 indeed being more susceptible to kidney failure when affected by other nephrotoxic events. Although we could not assess it in our cohort, new biomarkers have been reported as factors significantly associated with more severe kidney damage in the pediatric allo-HSCT, such as serum cystatin C (cysC) and urinary neutrophil gelatinase-associated lipocalin (NGAL).13
The septic shock was an important complication in our cohort and one of the leading causes of kidney failure, experienced by 29.7% of the whole patient cohort and by 83.9% in the hemodialysis subgroup. Several studies addressed the need for admission in the intensive care unit (ICU) following allo-HSCT, which is usually caused by respiratory failure and uncontrolled sepsis,14-19 while we found one study15 that specifically focused on sepsis during the first year. The reported rate of ICU admission is heterogeneous, ranging from 11.4%19 to 13%,17 while a large case series reported up to 35%16 after a one-year follow-up. Therefore, these studies reported that septic shock incidences also range widely, from 3.217 to 15.7%.15 Indeed, they reported the duration of neutropenia as ≥ 14 days15 and acute GVHD17 as a risk factor for sepsis15 and UCI admission.17 Furthermore, the need for hemodialysis in the ICU is high, possibly affecting up to 66% of those patients.18
Despite the observation that polymyxin B and amikacin were associated with HD in the univariate analysis, we must interpret this data carefully, as these drugs are frequently used to treat septic shock, which was also identified as a risk factor for dialysis. The kidney function of these patients deteriorated rapidly (Figure 3; 48 - 72 hours), which might be a relatively short time to favor the possibility of drug-induced, rather than shock-induced, kidney lesion.
Before evaluating the impact of cidofovir on kidney failure, we must consider that the classical indications for this drug are adenovirus/BK-polyomavirus infections in a subset of severely immunosuppressed patients, which are frequently associated with hemorrhagic cystitis, viral-induced nephritis and microangiopathy, all known as nephrotoxic conditions, as well.2,5,11,20-22 Moreover, considering that in the haploidentical subset of patients, the incidence of hemorrhagic cystitis could reach up to 62%21 and in this context, we may explain why the haploidentical was also found as a risk factor for HD. Indeed, we believe that the TAM would also be contributing to kidney damage in our study, although it was not statistically significant in the multivariate analysis. As the TAM may be driven by CNIs, in this analysis we observed a shorter duration of the CNI in the HD group, probably because these patients died earlier; moreover, some stopped taking the CNI after kidney failure diagnosis due to suspected microangiopathy.
Despite the measures taken to prevent cidofovir-induced kidney injuries, such as using probenecid, hydration and dosing adjustments, unfortunately, our study found that cidofovir was strongly associated with the need for hemodialysis. Unacceptably, the subset of patients treated with cidofovir experienced a very high rate, up to 80%, of kidney failure, which is different from the rate of 9.3% reported by a systematic review.20 Another study had not observed an impact of cidofovir on the survival of patients with hemorrhagic cystitis.22 These findings, taken together with the observed toxicity profile, should make clinicians aware of the necessity to use this drug carefully.
ConclusionsThe observed one-year cumulative incidence of renal replacement therapy in allo-HSCT was 17.6%. Patients in hemodialysis had a very high mortality rate, of up to 80%, at one year following transplantation. Clinicians must be aware of cidofovir use and adjust the conditioning intensity, calcineurin inhibitors and other drugs and immunosuppression to prevent patients from being exposed to bacterial and viral infections, microangiopathy, shock and other nephrotoxic events. This is even more important because these interventions may have a greater impact in the haploidentical HSCT patient subset.
Fundingnone.
The authors thank the medical writer Patricia Logullo (based in Oxford, UK) for providing medical writing support and formatting the manuscript for publication and they personally funded her work. Additionally, the authors thank Jade Zezzi Martins do Nascimento, in the Hematology Department, Hospital Israelita Albert Einstein, for contributing in the data collection.