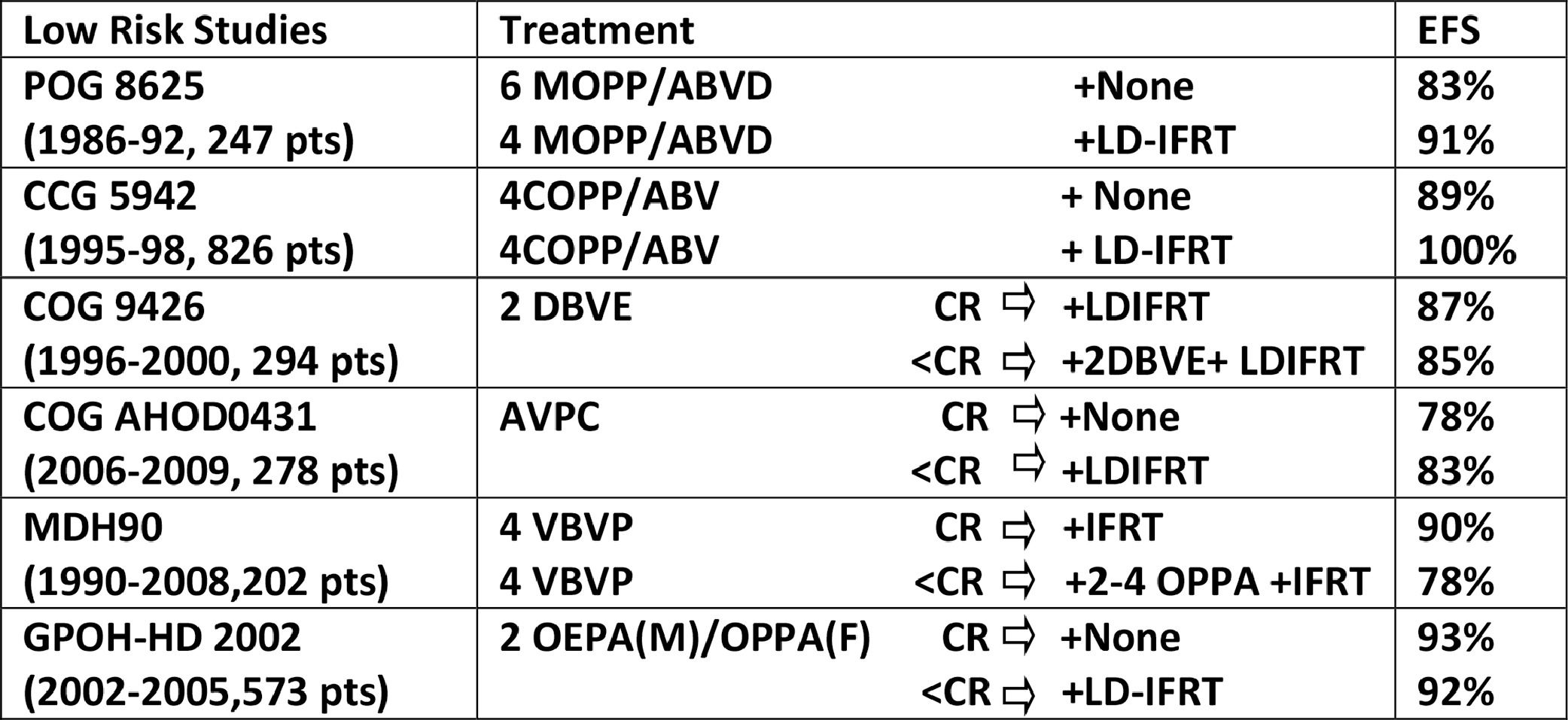
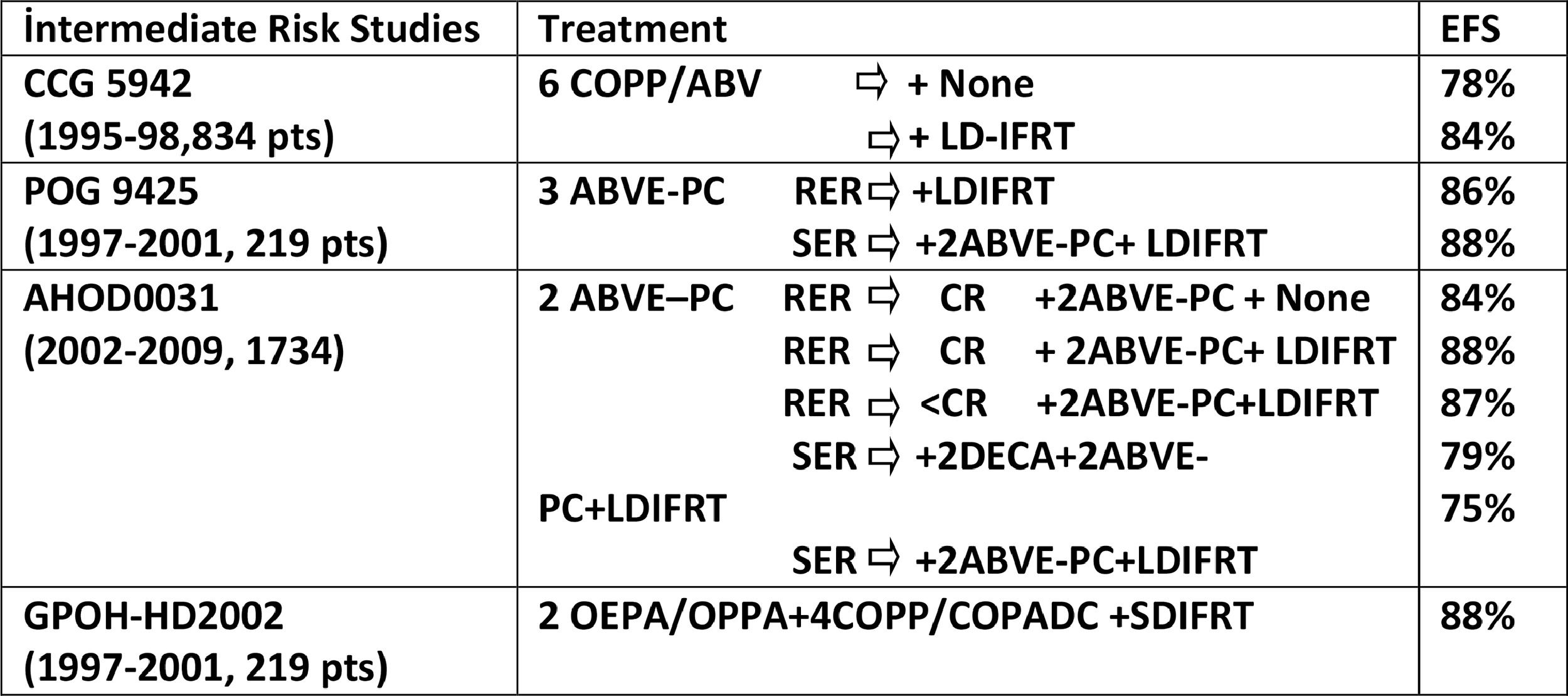
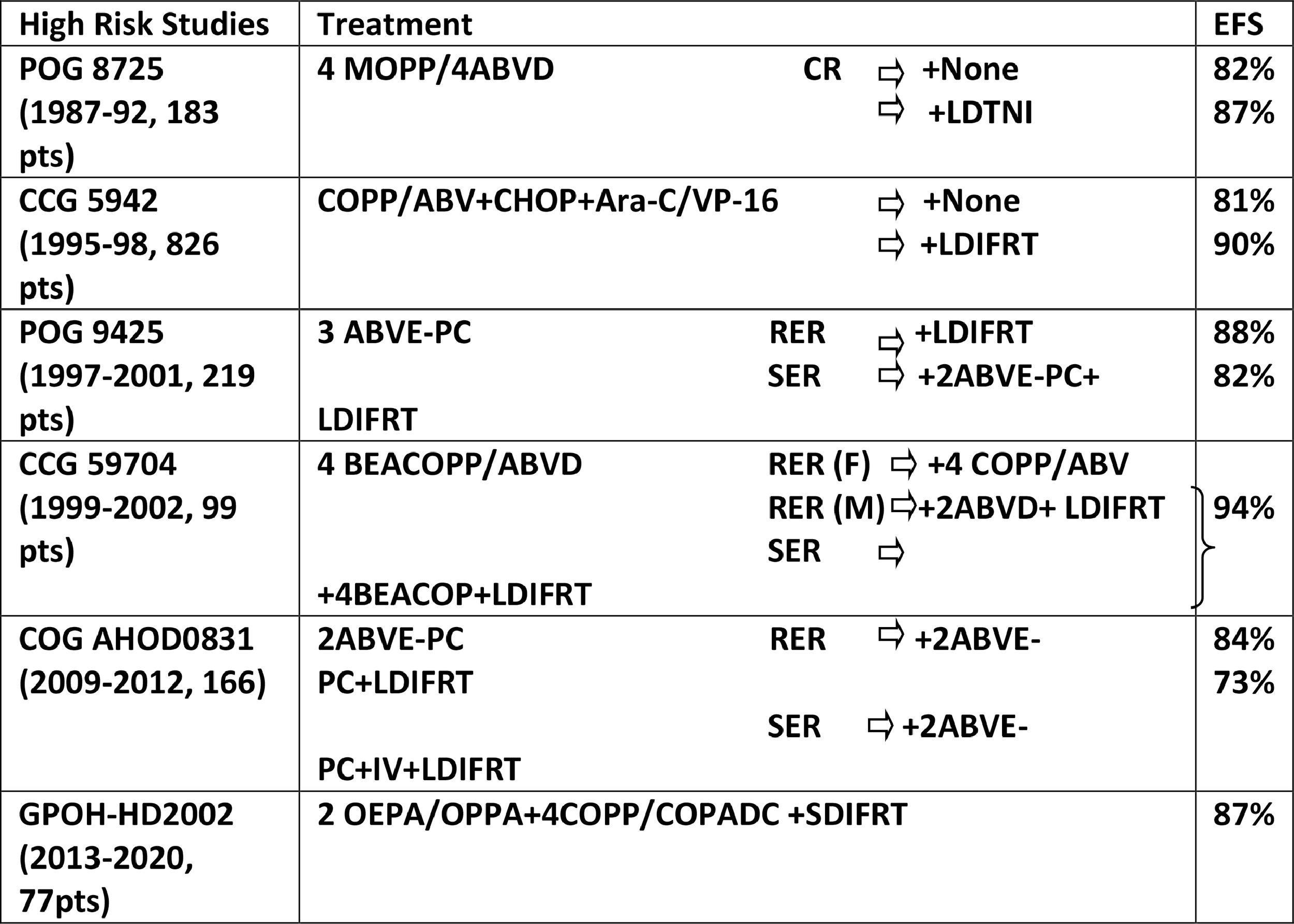
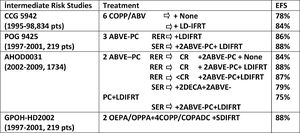
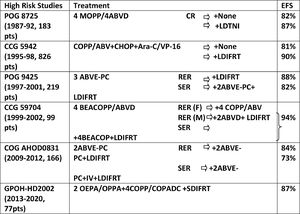
The treatment of HL has been designed according to risk stratification. Risk stratification is based on presenting features at diagnosis. Stage of disease, presence of bulky disease, presence of B symptoms, and number of involved nodes are the parameters of risk determination. Low risk group includes stage IA and IIA disease with no tumor bulk and no extranodal involvement. Stage IA and IIA with bulky disease or extranodal involvement, and stage IB and stage IIIA are defined as intermediate risk. Stage IIB with with bulky disease or extranodal involvement, IIIB and IV diseases are in high risk group. Treatment of HL in children consists of combined modality treatment including multiagent chemotherapy and low dose involved field radiotherapy. Modern therapy of HL can be based on both risk group and response (Table I, II, III). Standard chemotherapy in Hodgkin disease is ABVD or MOPP derivatives. Adriamycine, Dacarbazine, Bleomisin and Vinblastin are the major drugs of ABVD derivative protocols. MOPP derivatives include generally cylophospamide, vincristine, procarbazine, prednisolone. Hodgkin lymphoma is a radiosensitive disease. In general, doses of 15 to 25 Gy are used with modification based on patient and disease characteristics. In combined modality era, the extended treatment volumes are no longer needed. The Involved fields reduce the exposure of normal tissue and the late side effects by not reducing local control rate. The implementation of more tailored fields is a progress toward this goal, treating only the individual lymph nodes with a margin for microscopic disease. This, in conjunction with modern imaging, will continue to reduce exposure of normal tissue to radiation while maintaining equivalent local disease control rates. In some recent trials, radiotherapy was omitted in localized low risk disease and early responder patients.
Combined modality treatment will result in very high cure rates (Table I, II, III). The treatment results in children with early stage disease are perfect. Disease-free survival and overall survival reach up to 95% and 100%, respectively. About ten to twenty percent of advance stage patients may relapse. Since the prognostic outlook and life expectancy of HL have shown significant progress over the last decades, the quality of life and prevention of late side effects have gained considerable importance. Balance ensuring the best opportunity for long-term disease-free survival and the lowest risk of severe treatment toxicity should be achieved.
Table I. Treatment of Low Risk Group
Table II. Treatment of Intermediate Risk Group
Table III. Treatment of High Risk Group