The time elapsed from diagnosis to hematopoietic stem cell transplantation (HSCT) is influenced by numerous factors. In Brazil, patients using the public health system are also dependent on the availability of HSCT-specific beds in the hematology ward.
Objective and MethodsWe conducted a cohort study of listed patients who underwent allogeneic HSCT at a Brazilian public hospital to investigate the impact of the waitlist time on post-HSCT survival.
ResultsThe median time from diagnosis to HSCT was 19 months (IQR, 10 - 43), of which 6 months (IQR, 3 - 9) were spent on the waitlist. The time on the waitlist for HSCT appeared to influence mainly the survival of adult patients (≥ 18 years), with an increasing risk according to this time (RR, 3.53 and 95%CI, 1.81 - 6.88 for > 3 and ≤ 6 months; RR 5.86 and 95%CI, 3.26 - 10.53 for > 6 and ≤ 12 months, and; RR 4.24 and 95%CI, 2.32 - 7.75 for > 12 months).
ConclusionPatients who remained on the waitlist for less than 3 months had the highest survival (median survival, 856 days; IQR, 131 - 1607). The risk of reduced survival was about 6-fold higher (95%CI, 2.8 - 11.5) in patients with malignancies.
A higher time interval from diagnosis to HSCT is associated with a higher relapse rate and greater accumulated toxicity due to the need for more treatment lines while the patient is waiting for the HSCT.1–3 Several factors influence the time interval from diagnosis to HSCT, such as the duration of the treatment protocol, the time to indication for transplant and the severity of the underlying disease and availability of a compatible donor. In Brazil, in addition to these factors, patients using the public health system are also dependent on the availability of HSCT-specific beds in a hematology ward, which is an additional concern for successful treatment.2 Based on this reality, we investigated the impact of the waitlist time for allogeneic HSCT on the post-transplant survival at a public hospital in southern Brazil.
MethodsThis was a retrospective cohort study of patients listed for HSCT at a public hospital in southern Brazil between January 2013 and June 2019. Patients who underwent HSCT through a private health insurance system were excluded. All data were collected from electronic medical records until November 2020. The following variables were collected to characterize the sample: the patient socioeconomic data, diagnostic data and data related to the period between diagnosis and HSCT (initial and pre-HSCT disease status, time from diagnosis to HSCT and time on the waitlist for HSCT with an identified donor); HSCT data (transplant type, hematopoietic stem-cell source, conditioning regimen, graft-versus-host disease (GVHD) prophylaxis, time to neutrophil engraftment [neutrophil count greater than 500 cells/mm³ for 3 consecutive days], donor chimerism, final disease status and length of hospital stay]); donor data, and; data related to post-HSCT outcomes. We classified acute and chronic GVHD by target organ and overall severity according to previously published clinical and laboratory criteria.4,5
Myeloablative conditioning regimens were defined as those containing a dose of total-body irradiation above 9 Gy, busulfan at a dose of 8 mg/kg or more and melphalan at a dose of 140 mg/m² or more. In patients undergoing HLA-identical sibling HSCT who received myeloablative regimens, GVHD prophylaxis included cyclosporine and methotrexate (on days +1, +3, +6 and +11), with the exception of pediatric cases of acute lymphocytic leukemia (ALL) and myelodysplastic syndrome, in which methotrexate is not used. In patients undergoing matched unrelated donor HSCT who received myeloablative regimens, prophylaxis included tacrolimus or cyclosporine and methotrexate (on days +1, +3, +6, and +11) in addition to rabbit anti-thymocyte globulin at a total dose of 7 to 14 mg/Kg. In patients receiving reduced-intensity regimens, prophylaxis included mycophenolate mofetil in combination with cyclosporine. In haploidentical donor HSCT, prophylaxis included cyclophosphamide after stem cell infusion (on days +3 and +4) in combination with tacrolimus or cyclosporine and mycophenolate mofetil. In cord and placental blood HSCT, prophylaxis included tacrolimus or cyclosporine without methotrexate. Eligible patients are listed on the date a donor is found and begin scoring priority points based on the time on the list and diagnosis.6 To prioritize cases, the Brazilian Ministry of Health applies objective scoring criteria that include the urgency and curability of each diagnosis. Diagnoses that score the highest in these criteria are severe aplastic anemia, hypocellular myelodysplastic syndrome, severe combined immunodeficiency, osteopetrosis and acute leukemia with induction failure. For patients younger than 13 years of age, regardless of the underlying disease, 20 points are added to the final score. In addition, 0.33 points are added for every day on the waitlist.6
The primary outcome was patient survival from HSCT to the end of the follow-up (death or last follow-up visit). We used SPSS software, v. 27, for statistical analyses. Results were summarized descriptively and are presented as means with standard deviations, medians with interquartile ranges (IQRs, 25th to 75th percentile) or numbers and percentages of patients with the characteristic under study. The variables were compared with the use of nonparametric tests and the differences between proportions were analyzed by the chi-square test. A univariate analysis was conducted to identify the variables associated with survival. Continuous variables were categorized into quartiles (Q1, Q2 and Q3) for the survival analysis. The survival was estimated with the use of the Kaplan-Meier method and compared with the use of the log-rank test and/or Tarone-Ware test. Variables with a log-rank p-value of less than 0.20 were included in the multivariate regression model.
We used multiple imputation for missing data in the Cox regression model for the survival analysis.7,8 Only the variables with a p-value of less than 0.05 were kept in the final general model. In addition to the general model, we performed survival analyses for pediatric (younger than 18 years of age) and adult patients and according to the diagnosis (malignancies). The study protocol was approved by the institutional review board of the participant hospitals, under registration numbers 63004716.6.1001.5330 and 02898218.0.3001.5327.
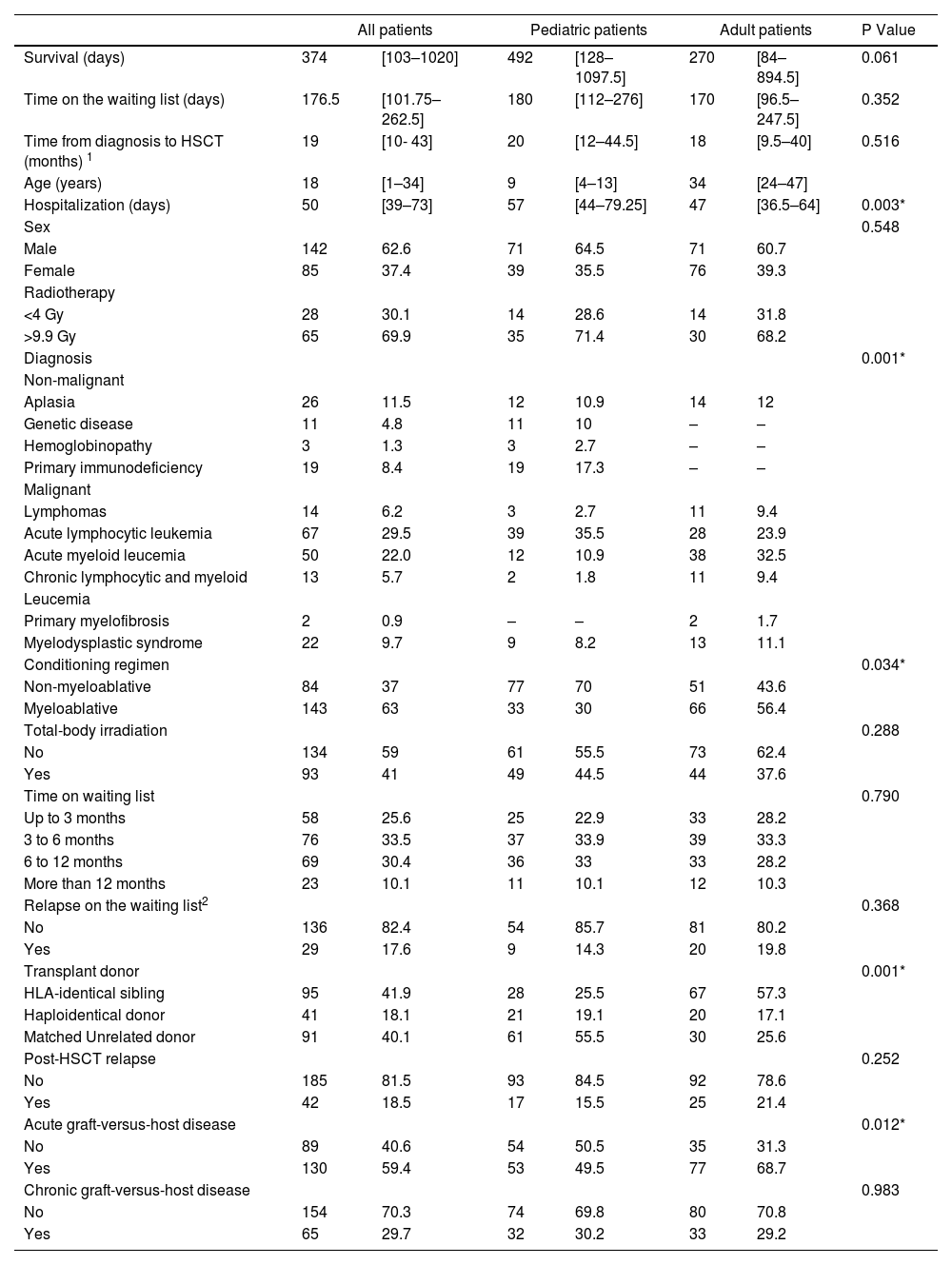
ResultsDuring the period reviewed, 227 patients underwent a transplant (110 pediatric patients and 117 adult patients). The median time from diagnosis to HSCT was 19 months (IQR, 10 to 43), of which 6 months (IQR, 3 to 9) were spent on the waitlist. A total of 168 patients (74%) had a diagnosis of malignancy (Table 1).
Baseline characteristics of the patients.
Data presented as absolute number and% or as median and P25-P75. HSCT: hematopoietic stem-cell transplantation. 1Time from the date of the first diagnosis to the first HSCT; 2only for malignancies. *Significant difference in the comparison between adult and pediatric patients.
When assessed according to type of transplant, the median time from diagnosis to HSCT was 12 months (interquartile range, 8 to 30) in patients undergoing HLA-identical sibling HSCT, 18 months (interquartile range, 9 to 47) in patients undergoing HLA-haploidentical donor HSCT and 25 months (95% confidence interval [CI], 15 to 50) in those undergoing matched unrelated donor HSCT, with a significant difference only between HLA-identical sibling and matched unrelated donor HSCTs (p < 0.001 by the Kruskal-Wallis test). We observed a similar scenario when the analysis was limited to time on the waitlist, with a median waiting time of 5 months (interquartile range, 3 to 7) for HLA-identical sibling and HLA-haploidentical donor HSCTs and of 8 months (interquartile range, 4 to 11) for matched unrelated donor HSCT (p < 0.001 by the Mann-Whitney test).
The patients with acute lymphoblastic leukemia (ALL) (n = 67) remained on the waitlist for approximately 7.5 months (IQR, 5.75 to 10.25) and had a median post-HSCT survival of 10.5 months (IQR, 3.2 to 17.7), whereas those with acute myeloid leukemia (AML) (n = 50) remained on the waitlist for approximately 6 months (IQR, 4 to 7) and had a median post-HSCT survival of 7.6 months (IQR, 3.3 to 26.7). Among all patients with malignant diseases (n = 168), we observed a difference between their disease status upon being placed on the waitlist and at the time of transplant (p < 0.001 by the chi-square test). The HSCT was performed upon the worsening of the underlying disease in 12.4% of patients with malignancies who were in CR1 upon being placed on the waitlist. Considering the patients in CR1 or in CR2 or later remission (n = 168), 17.7% relapsed while on the waitlist, requiring a new treatment line. Patients with malignancies who relapsed while on the waitlist had a 2-fold higher risk of reduced post-HSCT survival than those who did not relapse (relative risk, 1.58; 95%CI, 1.3 to 2.00).
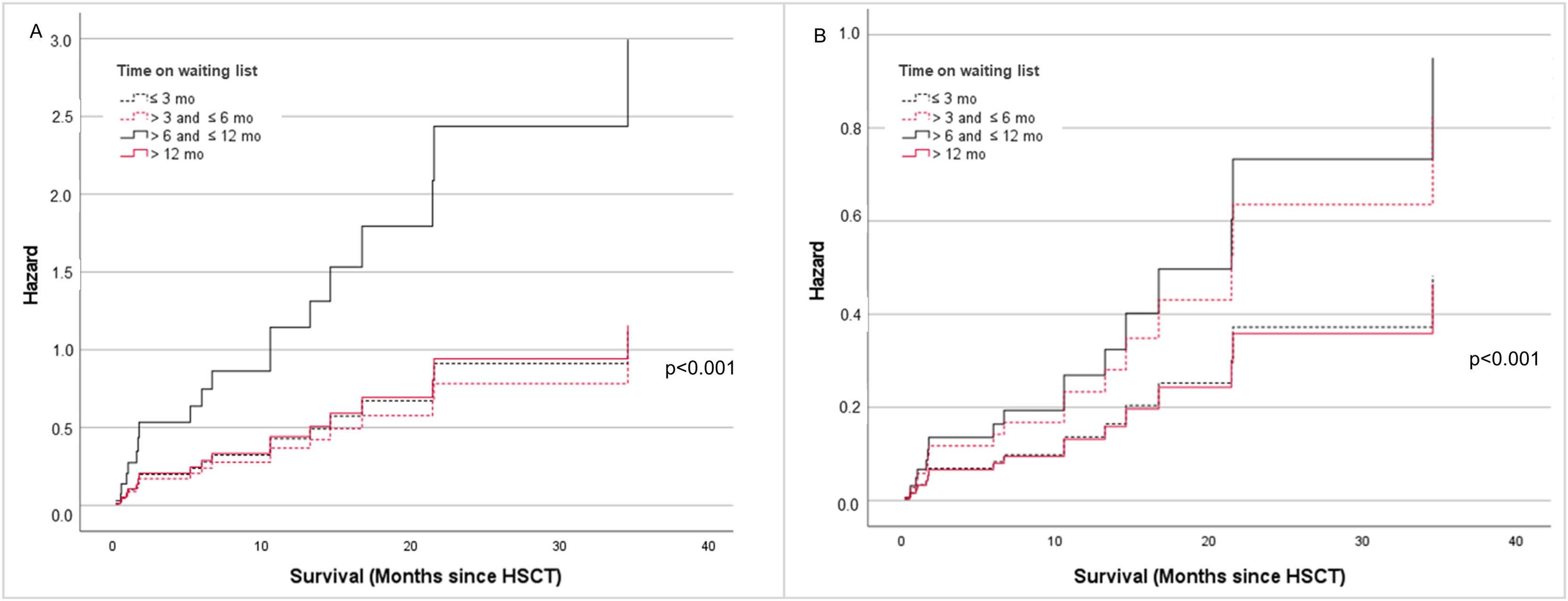
The median post-HSCT survival of the cohort was 12.5 months (IQR, 3.5 to 34). The analysis of the survival by time on the waitlist showed a benefit for patients undergoing HSCT within 3 months of placement on the waitlist (median survival, 28.5 months; IQR, 4.4 to 53.6) (Figure 1B). Survival did not differ significantly among patients undergoing HSCT from 3 to 12 months (median survival, 11 months [IQR, 4 to 26.2] and 11.8 months [IQR, 3 to 27], respectively). Patients on the waitlist for more than 1 year had a median survival of 8 months (IQR, 2 to 25.3). The difference between the subgroups divided by time on the waitlist was greater in early survival (p = 0.035 by the log-rank test) than in long-term survival (p = 0.78 by the Tarone-Ware test). In this cohort, the type of transplant did not influence the post-HSCT survival (p = 0.873 by the log-rank test). Considering the reality of the Brazilian Public Health System, we created 3 scenarios to assess the post-HSCT survival according to time on the waitlist with an identified donor: an ideal scenario (up to 3 months), the most common current scenario (approximately 6 months) and an unfavorable scenario (more than 12 months) (Figure 2). Based on these scenarios, we observed that patients who undergo a transplant within 3 months have an overall survival (OS) of 60%. However, after 12 months on the waitlist, the OS drops to 30%, with 62.5% of patients dying in the first 100 days after the HSCT and 37.5%, after that period. The most common causes of death in this group were infection (81.3%) and disease progression (12.5%).
Graphic representation of possible scenarios. The gray area represents the time of transplant. In the ideal scenario, transplant was performed at most 3 months after a donor had been identified and the patient had been placed on the waiting list. In the most common scenario, transplant was performed about 6 months after the patient had been placed on the waiting list. The range of gray shades represent the IQR (25th to 75th percentile, 3 to 9 months). Patients on the waiting list for more than 12 months had the lowest survival rate. HSCT: hematopoietic stem cell transplantation; mo: months.
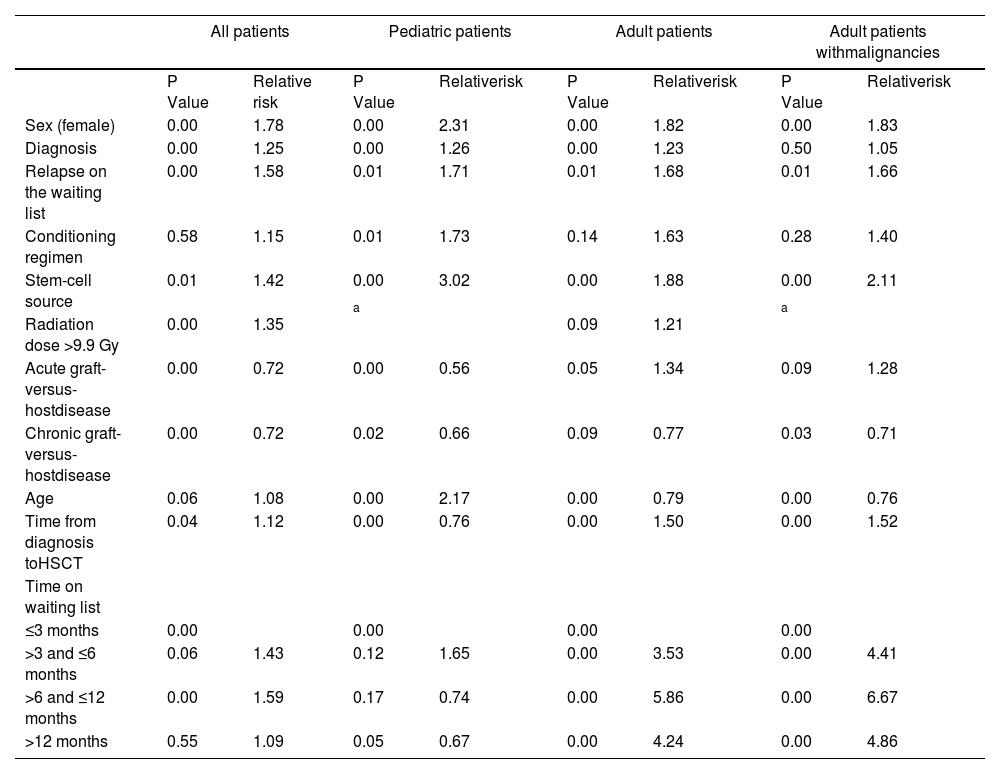
We performed an analysis including all variables that influenced survival to confirm whether time on the waitlist was an independent predictor of the post-HSCT survival. Table 2 shows the association of predictor variables (log-rank p-value > 0.005) with the post-HSCT survival. Multivariate models showed that variables influencing the post-HSCT survival are associated with the characteristics of the patient and that time on the waitlist appeared to influence mainly the survival of adult patients (older than 18 years of age) with an increasing risk according to the time spent on the waitlist for the HSCT (relative risk, 3.53 and 95%CI, 1.81 to 6.88 for > 3 and ≤ 6 months; relative risk, 5.86 and 95%CI, 3.26 to 10.53 for > 6 and ≤ 12 months, and; relative risk, 4.24 and 95%CI, 2.32 to 7.75 for > 12 months). We observed differences in survival between the subgroups divided by time on the waitlist throughout the follow-up (p = 0.037 by the log-rank test and p = 0.037 by Tarone-Ware test) (Figure 3A). None of the adult patients who waited more than 12 months for a transplant had a post-HSCT survival greater than 3 years (median survival, 3.3 months; IQR, 2 to 11.3).
Multivariate analysis of the association of predictor variables with post-HSCT survival.
Cox regression model adjusted for sex, diagnosis, whether the patient relapsed while on the waiting list, conditioning regimen, stem-cell source (bone marrow, peripheral-blood stem cells, and cord blood), radiation dose, presence of acute and chronic graft-versus-host disease, age (years), and time from diagnosis to HSCT (days). a constant covariate. P values of less than 0.005 were considered significant.
HSCT: Hematopoietic stem cell transplantation; Mo: Months. A: Adult patients (n = 117). B: Adult patients with malignancies (n = 103). Cox regression model adjusted for sex, diagnosis, whether the patient relapsed while on the waiting list, conditioning regimen, stem-cell source (bone marrow, peripheral-blood stem cells, and cord blood), radiation dose, presence of acute and chronic GVHD, age (years), and time from diagnosis to HSCT (days). P values of less than 0.05 were considered significant.
Adult patients with malignancies had an even worse prognosis, with a median survival of 7 months (IQR, 2.3 to 20.2) and a significant increasing risk for the waiting times > 3 and ≤ 6 months (relative risk, 4.41; 95%CI, 2.26 to 8.61); > 6 and ≤ 12 months (relative risk, 6.67; 95%CI, 3.72 to 11.97), and; > 12 months (relative risk, 4.86; 95%CI, 2.66 to 8.89) compared to patients undergoing the HSCT within 3 months. Pediatric patients, regardless of the diagnosis, did not have a significant risk of reduced survival with increasing time on the waitlist (relative risk, 1.65 and 95%CI, 0.87 to 3.11 for > 3 and ≤ 6 months; relative risk, 0.74 and 95%CI, 0.48 to 1.13 for > 6 and ≤ 12 months, and; relative risk, 0.67 and 95%CI, 0.46 to 0.99 for > 12 months) (Table 2).
DiscussionThis is the first study to assess the impact of the time elapsed on the waitlist on the post-transplant survival in patients undergoing allogeneic HSCT. We identified the time on the waitlist as an independent factor that impacts survival and overall mortality after the HSCT, which can be seen as a decisive factor in maintaining the indication for transplant, given that overall survival decreases to 30% after 12 months on the waitlist.
The main finding from this study was that most patients waited a median of 6 months for a transplant, whereas a waiting time of less than 3 months was associated with better survival. There is no previous data for comparison with other centers, as only data on the time from diagnosis to transplant have been reported. In Brazil, the median time from the diagnosis to the allogeneic HSCT was 10 months (range, 1 to 161) for primary myelodysplastic syndrome9 and 24 months (range, 8 to 186) for advanced indolent lymphoproliferative disorders.10 In a study conducted between 1994 and 2013 at the same institution, the average time from the diagnosis to the allogeneic HSCT was 26.8 months,11 which is quite different from the median time of 19.0 months (IQR, 10.0 to 43.0) we observed in our sample.
This difference may be explained by changes in the characteristics of the patients, as previously 40.6% of the sample consisted of patients with chronic myeloid leukemia, with no haplo-HSCTs and few matched unrelated donor hematopoietic stem cell transplantations (MUD-HSCTs) since the MUD and haplo-HSCTs started to be performed at the institution only in 2005 and 2014, respectively.
Studies in high-income countries have reported a shorter median time from the diagnosis to the HSCT. A study of the European Group for Blood and Marrow Transplantation reported a median time from the diagnosis to the HSCT of 195 days (range, 139 to 379) with a reduction in the overall mortality when the HSCT was performed within 142 days in a sample of patients with AML predominantly in CR1.12 The median time from diagnosis to transplant was longer in patients in CR2 or more or with underlying diseases requiring longer protocols, such as ALL.13 This makes the interval from the diagnosis to the transplant of doubtful use for assessing issues, such as the access to health services and the health system saturation.
When indicated, the HSCT should be performed as early as possible.14 However, the waiting time in each transplant center will depend on the type of health system used in the country and on the institution where the transplant center is located. It is important to note that, while we have observed a saturation of our health system, the fact that every Brazilian citizen has the right to access health services through a single, universal public health system is still a favorable scenario, compared to other health systems in which citizens without private health insurance do not even have access to the initial treatment for the underlying disease. The difference in time from the diagnosis to the HSCT between donor types we observed in this study may also be related to the time required to search for a donor and the donor availability, a difference that has already been described in previous studies.15–17 The HLA-identical sibling HSCT has the advantage of a donor available in the family, in which case the search process takes approximately 1 month.17 The haploidentical donor HSCT emerged precisely to make transplant feasible in patients who do not have an identical donor, but urgently need a transplant due to the high risk of relapse of the underlying disease, the reason for which they cannot wait much longer for a matched unrelated donor.16,17 Although the process of identifying a matched unrelated donor has advanced historically, the search time for this donor type takes about 3 to 4 months, in most cases17 due to the steps inherent to the search process, which is affected by factors, such as the HLA representation in ethnic minorities and the identification, acceptance and availability of the voluntary donor for hematopoietic stem cell collection.17 The longer time from the diagnosis to the matched unrelated donor HSCT we observed in this study may be explained by the fact that our transplant center is the only public reference center for this type of transplant in the state, also serving patients from a nearby state that does not have a center authorized to perform matched unrelated donor HSCTs. In addition, until 2017, our center was also the only reference center in the state for matched unrelated donor HSCTs performed through the private health insurance system.
Therefore, time from the diagnosis to the HSCT appears to be correlated, not only with the limited number of HSCT-specific beds, but also with the access to treatment, which will depend on multiple factors that include the ethnic, cultural and socioeconomic backgrounds, patient preferences and the structure of the public and private health systems.18–20 The unavailability of the identified donor to donate or the recipient unsuitability for transplant are also factors that may have influenced the waiting time we observed in this study, thus causing the transplant to be postponed even with an available bed. Although the criteria used in Brazil for prioritizing cases on the waitlist for HSCT establish that additional points are assigned to children younger than 13 years of age, the waiting time for the HSCT did not differ between adult and pediatric patients, i.e., the prioritization criteria used in the current scenario is not prioritizing children, as expected. This finding may be related to the increased number of children on the waitlist, in relation to the number of beds available at the institution. It should be noted that these criteria were introduced in 2009 and have not been updated as yet and the current scenario may no longer represent the scenario analyzed at the time of the study. Although pediatric and adult patients had similar waiting times, no reduction in the post-HSCT survival was observed in children according to time spent on the waitlist. This may be explained by the higher OS reported for children after the HSCT21 and by a higher proportion of benign diseases in children than in adults in our sample. It is worth mentioning that the HSCT was not performed in some cases because the patient died or the indication for transplant was withdrawn due to disease progression while on the waitlist. In addition, between 2016 and 2019, in a research project in partnership with the Brazilian Ministry of Health, 26 patients from the public hospital of this study and included in this sample underwent the HSCT at a partner philanthropic institution, which may have reduced the waiting time to perform the HSCT.
ConclusionIn this study, we were able to analyze the impact of the time elapsed on the waitlist on the survival of patients undergoing the HSCT, providing evidence that performing a transplant within 3 months promotes a higher overall survival. These data are of interest for HSCT centers that use transplant waitlists and for healthcare managers, as increasing the number of HSCT-specific beds is one of the factors that could reduce the transplant waiting time and possibly lead to higher post-HSCT survival rates.
ContributionsTSS conceived the project and participated in all phases of the manuscript preparation; CCA, DFV, ITSS, LBK and FB conceived the project; JDCH, MPP and CND wrote the first draft; JDCH conducted the data analyses; CND, ITSS, LBK, LDCR, GOZ, TDF, FLT, FFS, JCP, EEF, POS, AAP, LED and CCA participated in the data collection, data interpretation and helped write the manuscript. All authors were primarily responsible for revising the drafts for publication and reviewed the final version of the manuscript.
FundingThe data were obtained in partnership with the General Coordination Office of the National Transplant System-Brazilian Ministry of Health (CGSNT-MS) through the Institutional Development Support Program of the Brazilian Public Health System (PROADI-SUS).
We would like to thank the General Coordination Office of the Brazilian National Transplant System (CGSNT-MS), the Department of Specialized and Thematic Care and the Specialized Health Care Office of the Brazilian Ministry of Health staff.