The novel coronavirus disease has disrupted blood transfusion services worldwide. Despite blood transfusion services taking several precautionary measures to minimize the risks of COVID-19 during blood donations, donors became anxious regarding the risk of the COVID-19 infection during the donation and the blood transfusion services was facing the inevitable hazard of blood shortage.
MethodsThe study was conducted at a tertiary care oncology hospital-based blood transfusion services and included analysis of blood donations, packed red blood cell units requirements, and packed red blood cell inventory in the pre lockdown and lockdown phase. New COVID-19 standard operating procedures with enhanced safety guidelines and donor confidence-building measures were implemented at the blood transfusion services.
ResultsThe total number of average monthly blood donations decreased in lockdown but the decrease was not statistically significant (238.5 vs. 197.8, P = 0.391). The requisitions for the packed red blood cell cross-matches (722.5 vs. 329.0, P = 0.001) and the packed red blood cell utilization (176.5 vs. 103.3, P = 0.028) for the hospital patients also decreased significantly due to the lockdown. In the lockdown phase, an expressive number of packed red blood cell units were outdated due to the unprecedented fall in the number of patients. In the post-lockdown phase, the packed red blood cell inventory was optimized with decreased outdating via a comprehensive approach. A special emphasis was given to the in-house donations. A second partial lockdown also decreased the blood donations.
ConclusionConfidence-building in blood donors and the resolution of logistical issues were crucial for the efficient packed red blood cell inventory management in the lockdown. Implementation of COVID-19 preventive measures helped in the blood donor and blood transfusion services staff safety.
The novel coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was pronounced a pandemic by the World Health Organization on March 11, 2020.1 The first case of COVID-19 in India was reported on January 30, 2020 and to limit the spread of the infection, the Government of India had declared a complete national lockdown from March 25, 2020, to May 31, 2020.2 The controlled opening started on June 1, 2020, but major restrictions were in place until July 2020.2 With the enforcement of the lockdown, only essential grocery and medical facilities were allowed to remain open to the general population. As of August 5, 2020 with nearly 2 million cases, India had the third highest COVID-19 disease burden in the world, only behind the United States of America and Brazil.3
Round-the-clock news channels and social media created a sense of panic in the general population, including the blood donors, who became very apprehensive regarding the risk of contracting the SARS-CoV-2 infection during the blood donation. Moreover, the blood donation activities were thought to be against the social distancing protocols encouraged by the government. As all corporate and educational institutes were closed, the Blood Transfusion Services (BTS) were having a difficult time arranging the outdoor blood drives. With this pre-context, most of the BTS were facing the inevitable danger of blood shortage.
The packed red blood cell units (PRBC), with additive solutions, have a shelf life of 42 days and a sudden interruption of blood donations may not cause an immediate blood shortage, but continuous blood donation is needed to maintain the PRBC inventory for regular blood transfusions, as well as emergencies. Our hospital is a tertiary care oncology center, specialized in Hematopoietic Stem Cell transplants (HSCT), with many patients requiring routine and emergency transfusions.
The present study aimed to analyze the impact of the lockdown on the BTS with the PRBC utilization pattern and PRBC inventory management in the pandemic. The authors also sought to analyze the measures implemented at the BTS to decrease the impact of the lockdown.
MethodsThe study was conducted at a tertiary care oncology hospital-based BTS from January to July 2020. This was a combined prospective and retrospective analysis of blood donations, PRBC requirements and PRBC inventory in the pre-lockdown and lockdown phases. All the data was retrieved from the BTS records. The two PRBC utilization indexes, issuable stock index (ISI) and wastage as a percentage of issue (WAPI), were calculated. The issuable stock index (ISI) or days’ worth of stock is derived by dividing the issuable stock level by the nominal stock value. The issuable stock level is the number of unreserved PRBCs and the nominal stock value is the number of PRBCs transfused in a month, divided by the number of days. The WAPI is calculated using total PRBC wastage as a percentage of the PRBC issues, being the sum of the wastage PRBCs for the time/sum of the PRBCs issued for the same time × 100.
All the blood donations in the lockdown phase were performed as per the department's new COVID-19 standard operating procedures, with enhanced safety guidelines, as mentioned below.
Various methods implemented for PRBC inventory management1. Measures implemented to increase the number of voluntary blood donors
An appeal was made to all the voluntary blood donor organizers (VBDO) about the shortage and continuous need for blood components, even during the COVID-19 pandemic, and they were also informed about the steps to be taken by the BTS to ensure the prevention of the possible spread of the SARS-CoV-2 infection.
As the voluntary blood donor database decreased during the lockdown, the patient’s family members and friends were requested to come forward and donate blood in this time of crisis. No coercion was used for the blood donation. To relieve the anxiety and apprehensions in the general population regarding the blood donation process, mass media and social media were utilized to transfer information, education and awareness about safety measures implemented to prevent the possible spread of the SARS-CoV-2 infection.
2. Steps to increase donor safety
a. Implementation of a supplementary donor health questionnaire
A modified donor health questionnaire supplement was implemented following the guidelines of the apex national body of blood transfusion, the National Blood Transfusion Council (NBTC).4 The addendum included questions regarding donors/close contacts travel and contact history with a confirmed or suspected case of COVID-19 and symptoms of active infection. In the case of positive history or symptoms, the donor was deferred and referred to a medical clinic.
b. Education for BTS staff members
The BTS staff was educated on the current COVID-19 crisis and important prevention measures, such as hand hygiene, cough etiquette, social distancing, etc. The importance of Universal Precautions and Good Laboratory Practices was re-emphasized. Staff members were advised to follow the AABB resource document for blood establishments regarding the COVID-19 outbreak, the World Health Organization guidance document on the safety of the healthcare professionals and the Indian national guidelines for infection prevention and control in healthcare facilities.5–7
c. Advice and instructions for the VBDOs and individual blood donors
Donor information, education and communication (IEC) material, with precautions to be taken during blood donations, was given to the VBDOs for the prior circulation among the members and potential donors. The VBDOs were informed to promote the self-deferral of any donor with fever, cough or cold symptoms or who had had close contact with anyone with these symptoms or had a history of travel outside India within the last 28 days. The non-essential VBDO members and persons accompanying donors were informed to keep their numbers at a minimum. Higher age group donors (>55–60 years) with an underlying medical condition, such as high blood pressure or diabetes, were advised to avoid blood donations.
3. The donor appointment letter (Supplementary Material-I)
A donor appointment letter was prepared as per the state blood transfusion council suggestions. The letter mentioned the donor name and expected date and time of blood donation and its scanned copy was sent to all the donors via WhatsApp. The letter was printed on the official BTS letterhead and was signed and stamped. The local authorities were informed and requested to allow the easy transport of blood donors during the lockdown.
4. Precaution by the BTS staff at the outdoor drives and in-house donations
The use of alcohol-based-hand-sanitizers by donors at a convenient area, such as the reception and refreshment areas, was ensured for hand hygiene. Namaste was the preferred mode of greetings instead of the handshake or the hug. Personal protective equipment, including the N95 mask, hand gloves, face shields, etc., was made mandatory for the BTS staff in the donation premises. Used gloves were cleansed with alcohol-based hand sanitizers before and after coming in contact with donors and frequently changed.
5. Social distancing while at blood donations
The staggering of donors, avoiding over four donors at a time, was implemented in consultation with the VBDOs. The donor couches and chairs were kept at least two meters apart and in the case of fixed structures, every alternate chair was kept empty.
6. The procedural changes at the BTS
a. The rotational duty of the BTS staff
As the workload was decreased, only 40–50% of the BTS staff was informed to work and even those in rotating groups. The proposed plan was that in the case that any member of the BTS staff were to get infected with SARS-CoV-2, then the entire group would be quarantined and the standby group would take over.
b. Cleaning measures taken in the donation premises
All the blood donation couches were cleaned with a 1% hypochlorite solution after each donation. The sphygmomanometer, stethoscope, tourniquets, etc., were also cleaned accordingly. All the door handles/knobs in the BTS were cleaned on an hourly basis. The fumigation frequency of the donation area was increased and was performed as per the requirement.
c. Food and the pantry facility for the staff
The main cafeteria of the institution was closed and only pre-packed food parcels were available. The staff was advised to bring homemade food. Staff members were asked to consume food in staggered groups, avoiding overcrowding and maintaining physical distancing among BTS staff members.
d. Logistical issues
The police and civil authorities were requested to allow the movement of the donors amid the lockdown and supplied them with all the necessary documents.8 Continuous communication was maintained between the BTS staff and the vendors of blood bags and related disposables so that any problem in the transport could be managed at the institutional level.
7. The decrease in the outdoor blood donation drive activities
For any BTS, workplaces and educational institutions are the prime venues in which to organize the blood drives. In 2019, 58.1% (25/43) of the outdoor drives were conducted in these venues. Due to the lockdown, all the educational institutions and offices were closed and ‘Work from Home’ was promoted. As a consequence, the eligible sites for the blood drives decreased significantly and only local community-based drives could be organized.
Statistical analysesData were directly captured on Microsoft Excel spreadsheets and statistical analysis was performed using the SPSS for Windows (Version 25.0, IBM Corp. USA). Descriptive statistics such as mean, standard deviation (SD) and range values were calculated for normally distributed continuous variables. The pre-lockdown and lockdown data were compared using the independent-samples t-test. A two-sided probability of the p-value <0.05 was considered to be statistically significant.
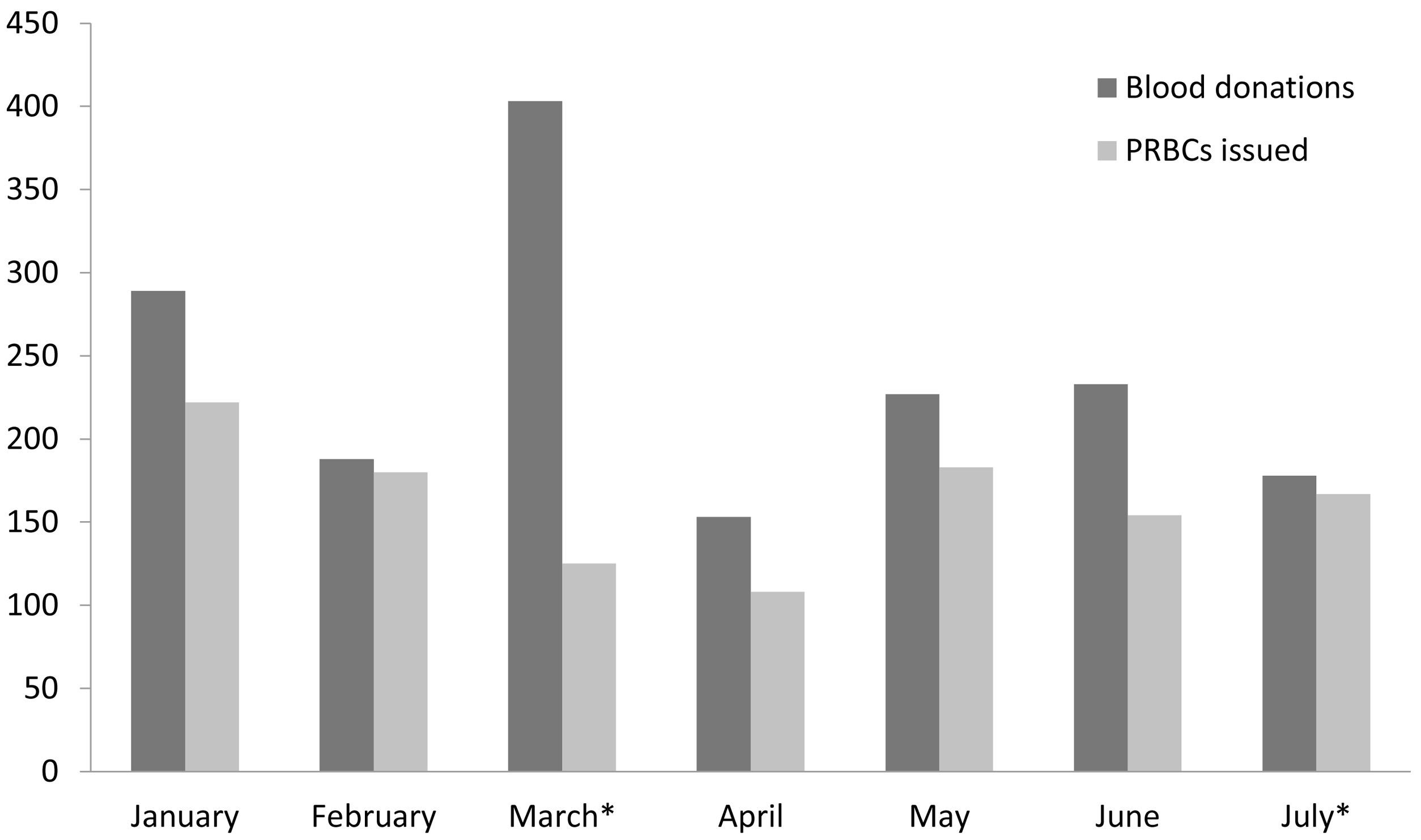
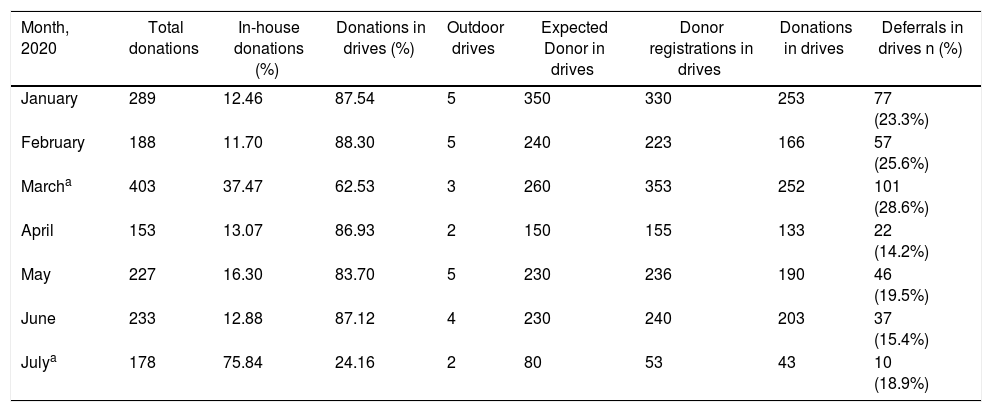
ResultsThe official lockdown was enforced on March 25, 2020, but social distancing was already the convention before that. Hence, the March data was not used for the comparisons. For the purpose of comparison, the data were grouped in January-February (pre-lockdown) and April-July (lockdown). All the data comparing the pre-lockdown and lockdown periods are the averages of both periods. The monthly average number of inpatients (498.5 vs. 222.5, p < 0.001) and outpatients (10,835.5 vs. 4545.3, p < 0.001) decreased significantly in the lockdown phase and the monthly average requisitions for the PRBC cross-matches also followed the same trend (722.5 vs. 329.0, p = 0.001). As all the elective surgeries were postponed, the monthly average PRBC cross-match requirements for surgeries also decreased considerably (529 vs. 226.3, p = 0.001). The same trend was also seen for the anemia cross-matches (193.5 vs. 102.8, p = 0.005). The monthly average PRBC utilization for the hospital patients also decreased significantly due to the lockdown (176.5 vs. 103.3, p = 0.028). The monthly PRBC cross-matches with the utilization pattern and the blood collection details are represented in Tables 1 and 2, respectively. The month-by-month blood donations and PRBC usage are represented in Figure 1. In April, an increased ISI was seen as a result of inflated inventory due to the panic about the imminent blood shortage and a high WAPI was seen due to the unprecedented fall in the number of patients and surgeries. The outdating of the PRBCs increased due to the lockdown (81.5 vs. 93.0, p = 0.735). In April (n = 140) and May (n = 112), a significant number of PRBC units was outdated due to the unprecedented fall in the number of patients. In June and July, a result of a comprehensive approach to the PRBC inventory management was seen and the inventory was optimized with decreased outdating.
Monthly PRBC cross-matches and the utilization pattern.
| Month, 2020 | Admitted patients | Out-patients | Total PRBC cross-matched | Cross-matches for surgery | Cross-matches for anemia | Total PRBC issued | PRBC issued in-house | PRBC units outdated | WAPI (%) | ISI |
|---|---|---|---|---|---|---|---|---|---|---|
| January | 514 | 11,113 | 738 | 526 | 212 | 222 | 186 | 89 | 40.09 | 32.6 |
| February | 483 | 10,558 | 707 | 532 | 175 | 180 | 167 | 74 | 41.11 | 25.05 |
| Marcha | 408 | 7238 | 607 | 496 | 111 | 125 | 114 | 31 | 24.8 | 59.88 |
| April | 245 | 4406 | 295 | 211 | 84 | 108 | 74 | 140 | 129.63 | 70.46 |
| May | 188 | 4028 | 273 | 173 | 100 | 183 | 92 | 112 | 61.20 | 35.31 |
| June | 227 | 4710 | 359 | 254 | 105 | 154 | 107 | 44 | 28.57 | 50.01 |
| Julya | 230 | 5037 | 389 | 267 | 122 | 167 | 140 | 76 | 45.51 | 36.38 |
ISI: Issuable stock index; PRBC: Packed red blood cell; WAPI: Wastage as a percentage of issue.
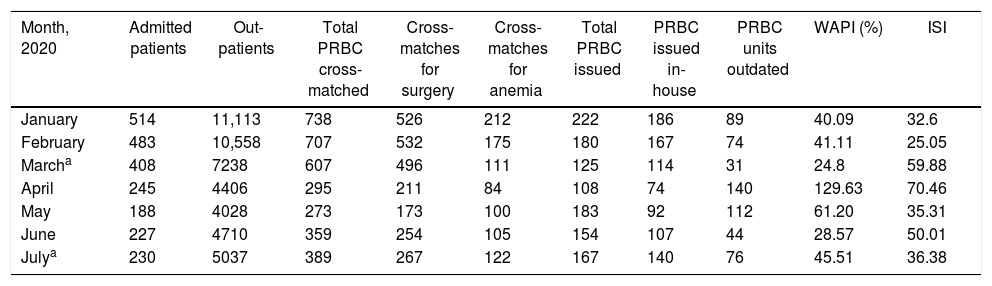
In-house donations and outdoor blood drives data.
| Month, 2020 | Total donations | In-house donations (%) | Donations in drives (%) | Outdoor drives | Expected Donor in drives | Donor registrations in drives | Donations in drives | Deferrals in drives n (%) |
|---|---|---|---|---|---|---|---|---|
| January | 289 | 12.46 | 87.54 | 5 | 350 | 330 | 253 | 77 (23.3%) |
| February | 188 | 11.70 | 88.30 | 5 | 240 | 223 | 166 | 57 (25.6%) |
| Marcha | 403 | 37.47 | 62.53 | 3 | 260 | 353 | 252 | 101 (28.6%) |
| April | 153 | 13.07 | 86.93 | 2 | 150 | 155 | 133 | 22 (14.2%) |
| May | 227 | 16.30 | 83.70 | 5 | 230 | 236 | 190 | 46 (19.5%) |
| June | 233 | 12.88 | 87.12 | 4 | 230 | 240 | 203 | 37 (15.4%) |
| Julya | 178 | 75.84 | 24.16 | 2 | 80 | 53 | 43 | 10 (18.9%) |
The total number of blood donations decreased in the lockdown, but the difference was not significant (238.5 vs. 197.8, p = 0.391). As an imminent shortage of blood was expected, blood donation was increased in March and special emphasis was given on the in-house donations. As no guidelines were available regarding the deferrals and the BTS was extra careful to exclude all the symptomatic and asymptomatic donors/carriers and the deferral rate increased considerably in March 2020 (101/353, 28.61%). After March, the guidelines became available and donors also started to self-defer, leading to the fall in deferral rates (14.2–19.5%). The institutional blood donor deferral rate for the year 2019 was approximately 18%. The donation decreased in April and results of measures implemented were seen and blood donations were normalized from May onwards. At the start of July, the local authorities imposed a 17-day lockdown in the city to limit the increasing number of COVID-19 cases. This had a direct impact on the BTS and the number of outdoor drives and total donations decreased in July.
DiscussionThe COVID-19 pandemic was a first-of-its-kind experience for the BTS and blood inventory management was a difficult task in these challenging times. The confidence-building in the blood donors and handling of the logistic issues were the most important factors for the efficient PRBC inventory management. In times of pandemic, implementations of measures that ensure the safety of the blood donors and BTS staff is the responsibility and social obligation of the BTS. Due to the implementation of infection prevention measures, none of the BTS staff or donors contracted the SARS-CoV-2 infection in the blood donation process.
Challenging differentiation between COVID-19 carriers and healthy blood donorsThe most common symptoms of COVID-19 included fever, dry cough, nasal congestions, sore throat and diarrhea9 and it was very difficult to differentiate healthy blood donors with these symptoms and COVID-19 patients or carriers. The average incubation period of COVID-19 is five days (range 1–14 days)9 and, in the incubation period, a carrier may not have any symptoms and may donate blood. The BTS must rely on the donor deferral policy to minimize the risk of potentially infected donors from entering the blood supply chain.
Risk of COVID-19 by blood transfusionRespiratory viruses, such as coronaviruses, are not ordinarily known to be transmitted by blood transfusion, the two previous coronaviruses (SARS and MERS) having been extensively investigated and no cases were ever reported by blood transfusion. The same may also hold true for SARS-CoV-2. Worldwide, more than 19 million3 cases of COVID-19 have been confirmed, but not a single case of transfusion-transmitted COVID-19 has been reported to date; still, there is a theoretical risk of transmission by blood transfusion.10,11 As SARS-CoV-2 is a new virus, its potential for transfusion transmission, even by an asymptomatic blood donor, is indeterminate. An initial study from the epicenter of the disease (Wuhan, China) reported that 15% of the clinically ill patients had RNA in their plasma or serum, but the authors emphasize that RNA is not synonymous with an infectious virus, which indicates there is no clear evidence for blood-borne transmission.12 A study by the Korean Red Cross Blood transfusion services also did not confirm SARS-CoV-2 infection in blood transfusion recipients who have received blood components from donors who were detected with SARS-CoV-2 infection after the blood donation.11 In a retrospective study in China by Chang and colleagues, COVID-19 was detected in four of the 4995 healthy blood donors.13 A recent study in northern India reported that 46 (3.7%) of the 1235 ‘healthy’ persons who had donated blood in the previous two weeks had the antibodies against SARS-CoV-2.14
Policy after the donor reports the COVID-19 infectionTo date, SARS-CoV-2 infection testing in blood donors has not been recommended by the NBTC. At the time of donation, the blood donors are advised and encouraged to inform the BTS in case of COVID-19 diagnosis, symptoms of COVID-19, or close contact with a COVID-19 patient up to 28 days post-donation. As per the national policy by the NBTC, the blood unit collected from such a donor must be recalled and discarded with all the precautions. And if such a blood component had been transfused into any patient, this obligatorily was to be informed to the patient’s attending physicians, as well as reported to the national hemovigilance system. This information would also have been useful to the BTS staff who came into contact with the donor in regard to their taking the necessary steps. In our study period, one donor reported COVID-19 7 days after donating and, as per the national guidelines, all the blood components of this collected unit were discarded.4
Fall in demand for the blood componentsAs most of the elective surgical procedures and non-urgent cases were postponed, the blood used at the hospital suddenly decreased and the BTS was facing an imminent danger of the outdating of PRBC units.
Comparison with similar studiesWith the start of the pandemic and lockdown, blood donations have decreased globally.15–21
Wang et al. reported that the number of whole blood donors dropped by 67% during the pandemic in China.15 Pagano et al. reported that the donor attendance decreased by 10–30% in the state of Washington, USA during the first two weeks of the COVID-19 pandemic.16 In the present study, donations were decreased by 17.1% in the lockdown phase. However, in the early stages of the pandemic, this decrease in blood donation was compensated by a reduction in blood utilization because of a decrease and/or postponement of elective surgeries and medical treatments.15–21 In India also, we have observed a similar trend and the blood donations (both outdoor and indoor) have decreased during the lockdown, but this has not affected the patient transfusions due to the decrease in the requirement.20,21
Transfer of blood components between the various BTSAs many of the hospitals were facing the acute shortage of the blood components and few hospitals were having a surplus of the blood components, the sharing and transfer of blood component was allowed by the NBTC among the licensed BTSs, so that the optimal use of precious blood components can be ensured. In April and May (Table 2), multiple units were transferred to other blood centres.
Transfusion requirements in COVID-19 patientsThe COVID-19 per se does not cause any illness that requires blood transfusion, but patients with pre-existing conditions may require the transfusion. At our oncology center, a few patients got infected with the SARS-CoV-2 and, as these patients had anemia and/or thrombocytopenia due to cancer or its treatment modalities, these patients required transfusions, but no extra measures were taken for these transfusions apart from the routine BTS procedures in COVID-19. Extra precautions were taken while receiving blood samples and requisitions from the COVID-19 patients.5–7
Role of the Hospital transfusion committee (HTC)The active meeting of the HTC was not organized to avoid gathering of persons, so the person-to-person communication occurred among the HTC members and the clinicians concerning the possible shortage of blood and effective blood utilization strategies. Clinician colleagues were also asked to motivate patient family members for voluntary blood donation and to follow the strict transfusion practices.
Push to the movement of patient blood management (PBM)The PBM is a concept that should be followed, irrespective of the pandemic. The COVID-19 crisis pushed the cause of PBM. As elective surgeries were postponed, there was sufficient time to increase the hemoglobin by dietary and/or medical methods in anemic patients. The use of alternative measures, instead of blood transfusion, was advocated and strict adherence to the transfusion guidelines was ensured.
Preparedness plan for future epidemicsEven after overcoming COVID-19, the situation may never return to what it was previous to the pandemic and the BTSs may have to learn to work with these ‘new normal’ conditions. The BTSs may inculcate this extra cautiousness in their routine and this may also have a positive impact on the donor population. It will be crucial to gather data and knowledge regarding the experience of different BTSs after the epidemic, which may help in formulating policies for blood and platelet inventory management in future pandemic events. National and international co-operation between the BTSs is very important to share knowledge and to learn from each other. BTSs must prepare standard operating procedures for these kinds of possible epidemics in the future. The current pandemic taught us that the BTS should make the policy and be ready to adapt to future natural or man-made calamities and the standard operating procedures should be in place for such unprecedented events. In this new era of globalization, a disease may not be confined to a geographical area and its worldwide spread is possibly imminent.
ConclusionsConfidence-building in blood donors and the resolution of logistical issues were crucial for the efficient PRBC inventory management in the pandemic lockdown. Implementation of measures to prevent SARS-CoV-2 infection contributed to the blood donor and BTS staff safety. The sharing of knowledge and experience is very important in such unprecedented events. This experience may be useful to other institutions if a similar pandemic lockdown occurs in the future.
Author’s contributionAll the authors contributed equally in concept design, acquisition of data, initial draft and final approval of the manuscript.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to acknowledge Dr. P Waghmare for the proof-reading and critical review of the manuscript.