Infection is a serious complication among patients with hematologic malignancies (HMs) and in hematopoietic cell transplant (HCT) recipients. In most centers, the management of these complications is provided by the hematologist in person, thus demanding a knowledge of basic aspects of infection.
MethodsTo evaluate the knowledge of the hematologist on infections, we invited clinicians to answer two questionnaires with 20 multiple-choice questions covering epidemiology, prophylaxis, diagnosis and treatment of infection in patients with HMs and HCT.
ResultsWe obtained 289 answers: 223 in survey 1 (febrile neutropenia) and 66 in survey 2 (infection in HCT). The median score was 5.0 in both surveys (range 0.5 - 9.0). In survey 1, the questions with the lowest number of correct answers were Q3 (8%), concerning the cefepime dose, and Q1 (9%), which asked about the epidemiologic link between the use of high dose cytarabine and viridans streptococcal bacteremia. In survey 2, two questions about cytomegalovirus (CMV) infection had the lowest percentage of correct answers (Q4, 12% and Q11, 18%). Clinicians attending to HCT recipients had higher scores, compared to clinicians attending to patients with HM only (median score of 5.0 and 4.5, p = 0.03, in survey 1 and 6.0 and 4.5, p = 0.001, in survey 2). In both surveys staff clinicians, residents and professors had similar scores.
ConclusionThis is the first study in Brazil assessing the knowledge of hematologists on infectious complications. The low median score overall indicates an urgent need for continuous education. Such initiatives will eventually result in better patient care.
Infection is a major complication in patients with hematologic malignancies (HMs) receiving intensive chemotherapy or hematopoietic cell transplantation (HCT), with high morbidity and mortality rates.1,2 Infection in this scenario may be caused by bacteria, fungi, viruses and parasites, with clinical manifestations that are usually non-specific. At most centers, the management of infectious complications is provided by the hematologist in person, thus demanding a knowledge of basic aspects of infection. However, hematologists are already overwhelmed by the large amount of new information regarding the management of the underlying hematologic disease. On the other hand, major advances in the management of infectious diseases have occurred, including improvements in culture and identification of microorganisms,3,4 new biomarkers and diagnostic tools,5 new antimicrobial drugs,6 concepts of pharmacokinetics and pharmacodynamics of antimicrobial agents7 and therapeutic drug monitoring,8 among others. Therefore, managing infection in hematologic patients represents a great challenge.
One of the most important activities to improve the quality of patient care is education. However, to promote adequate educational programs, it is important to know possible gaps in the knowledge of different aspects of infection to develop targeted educational activities. With this aim, we performed a web-based survey with two questionnaires to evaluate the level of knowledge of the hematology community on infectious complications in febrile neutropenia and HCT.
Materials and methodsStudy populationWe invited clinicians from different parts of Brazil to answer a survey to evaluate the level of knowledge on the management of infectious complications in high-risk hematologic patients. The clinicians had to have experience in treating patients with hematologic malignancies and/or patients undergoing HCT. The recruiting of responders was performed by an announcement in the ABHH (“Associação Brasileira de Hematologia e Hemoterapia” – Brazilian Society of Hematology and Blood Transfusions) website. The participation in the survey was voluntary and anonymous and included hematologists from public and private centers.
SurveyTwo questionnaires were developed, both with 20 multiple-choice questions covering areas of the epidemiology, prophylaxis, diagnosis and treatment of infectious complications in hematologic patients. The first questionnaire (survey 1) was intended to evaluate the knowledge of hematologists in the management of febrile neutropenia. This included the most frequent pathogens causing infection and the recognition of clinical syndromes and strategies of antibiotic and antifungal prophylaxis and treatment. The second questionnaire (survey 2) covered topics related to the management of infectious complications in autologous and allogeneic HCT. The questions were built by one of the authors (M.N.) and the selection of the correct answers was made by the same author, based on his personal experience. We also collected basic sociodemographic data on hematologists, such as age, gender, region, hospital type (public or private), clinician category (resident, staff clinician or professor) and the main area of clinical practice (HM or HCT). Each correct answer was scored as 0.5, up to the maximum score of 10 points. The full survey instrument is available in Supplementary files 1 and 2. The questionnaires were provided to hematologists as an online tool, using the Survey Monkey platform.
Statistical analysisWe calculated the median score obtained by each participant and compared scores according to the main area of clinical practice, clinician category and age group (< 30 years, 31 - 40, 41 - 50, 51 - 60 or > 61 years old). Categorical variables were expressed as absolute numbers and percentage and were compared using Chi-square or Fisher's exact test, as appropriate. Continuous variables were summarized as medians and ranges and compared using the Mann-Whitney and the Kruskal-Wallis test. A p-value < 0.05 was considered statistically significant. Database creation and statistical analyses were performed using the SPSS version 21.0 (IBM, Armonk, NY, USA). This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
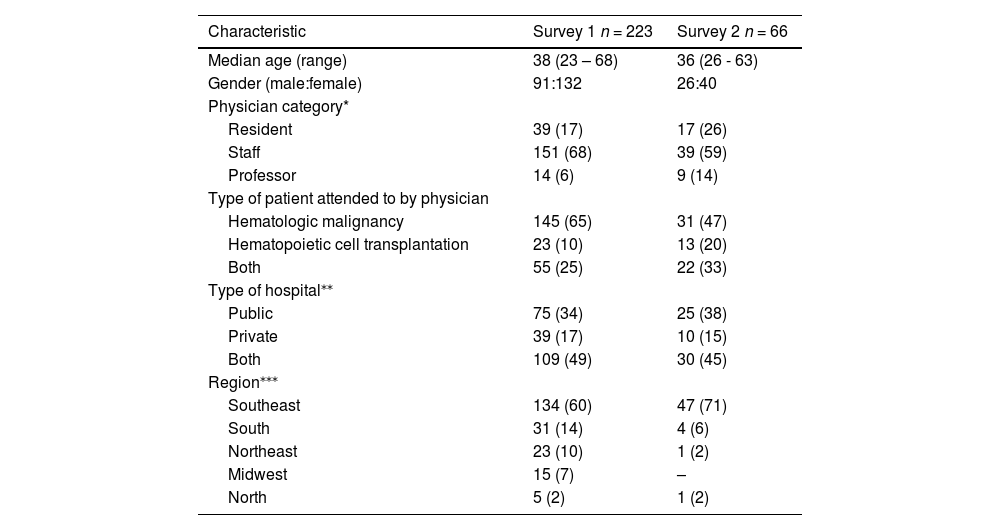
ResultsDuring the study period, we obtained 289 answers: 223 in survey 1 and 66 in survey 2. Demographic characteristics of participants are summarized in Table 1. The median age of participants in surveys 1 and 2 was 38 (range 23 - 68) and 36 (range 26 - 63), respectively. Most clinicians were staff physicians working with HM in both public and private hospitals. The majority of respondents were from the southeast region of Brazil. Overall, the median score was 5.0 in both surveys (range 0.5 - 9.0).
Demographic characteristics of participants.
| Characteristic | Survey 1 n = 223 | Survey 2 n = 66 |
|---|---|---|
| Median age (range) | 38 (23 – 68) | 36 (26 - 63) |
| Gender (male:female) | 91:132 | 26:40 |
| Physician category* | ||
| Resident | 39 (17) | 17 (26) |
| Staff | 151 (68) | 39 (59) |
| Professor | 14 (6) | 9 (14) |
| Type of patient attended to by physician | ||
| Hematologic malignancy | 145 (65) | 31 (47) |
| Hematopoietic cell transplantation | 23 (10) | 13 (20) |
| Both | 55 (25) | 22 (33) |
| Type of hospital⁎⁎ | ||
| Public | 75 (34) | 25 (38) |
| Private | 39 (17) | 10 (15) |
| Both | 109 (49) | 30 (45) |
| Region⁎⁎⁎ | ||
| Southeast | 134 (60) | 47 (71) |
| South | 31 (14) | 4 (6) |
| Northeast | 23 (10) | 1 (2) |
| Midwest | 15 (7) | – |
| North | 5 (2) | 1 (2) |
Numbers in parentheses represent percentages unless specified.
Overall, seven out of the 20 questions evaluated the knowledge of clinicians regarding the epidemiology, diagnosis and management of bacterial infections and 13 focused on invasive fungal diseases (IFDs). Among the seven questions dealing with bacterial disease, the lowest percentage of correct answers (8%) was question Q3. The question asked if cefepime should be given at a fixed dose and schedule or if the dose should be individualized, based on body weight and creatinine clearance. The second question with a low percentage of correct answers (9%) was question Q1, which asked about the epidemiologic link between the use of high-dose cytarabine and viridans streptococcal bacteremia.
Concerning IFDs, question Q20 had the lowest percentage of correct answers (16%). In this question, we asked if secondary prophylaxis was indicated for patients with a previous episode of candidemia. Most of the hematologists (83%) answered that secondary prophylaxis with fluconazole was needed. The question with the highest percentage of correct answers was Q7; 82% of clinicians answered that Pseudomonas aeruginosa, Klebsiella sp. e Escherichia coli are the leading agents of Gram-negative bacteremia in febrile neutropenia. The second questions with the highest percentage of correct answers (80%) tested the skills of clinicians in the management of patients with a positive blood culture for yeast (Q18) and Q14 (primary therapy for invasive aspergillosis).
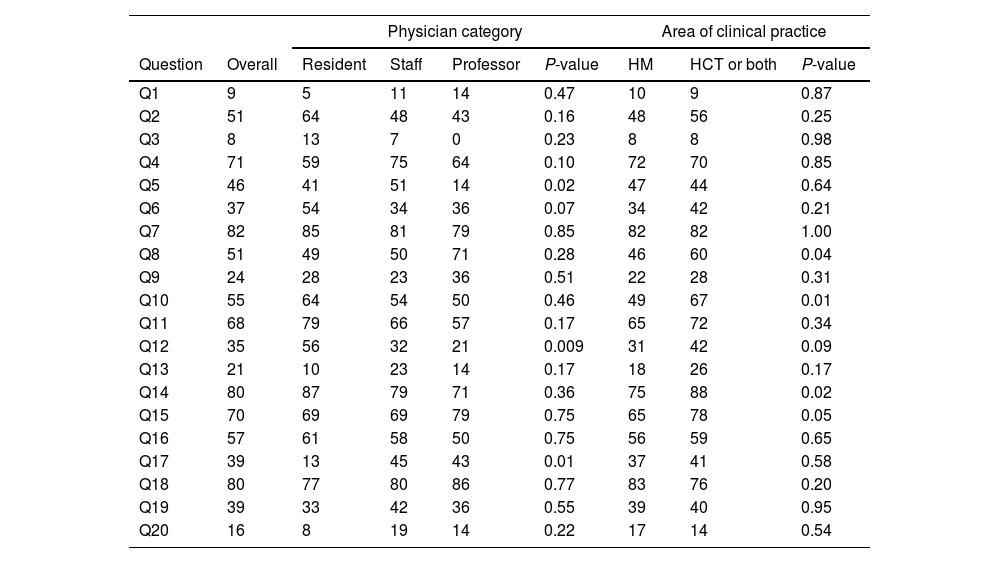
Overall, staff clinicians (4.5, range 0.5 - 9.0), residents (5.0, range 2.0 - 8.0) and professors had similar scores (4.0, range 1.5 - 7.5, p = 0.56). On the other hand, when we analyzed individual questions, some differences were observed. In Q12 (discontinuation of antibiotics after engraftment in autologous HCT) the rates of correct answers were 56%, 32% and 21% for residents, staff clinicians and professors, respectively (p = 0.009). Likewise, in Q5 (knowledge on characteristics of different antifungal agents), staff clinicians had the highest rates of correct answers (51%, compared to 47% for residents and only 14% for professors, p = 0.02) (Table 2).
Percentage of correct answers in survey 1 (febrile neutropenia) regarding physician category and main area of clinical practice.
HM = hematologic malignancy; HCT = hematopoietic cell transplantation.
The median scores of clinicians attending to HCT recipients were higher, compared to clinicians attending to patients with HM only (5.0, range 1.5 – 7.0 vs. 4.5, range 0.5 – 9.0, respectively, p = 0.03). As shown in Table 2, in four questions, clinicians attending to HCT recipients had significantly higher percentages of correct answers, compared to clinicians attending to HM only: question Q8, testing knowledge on amphotericin B (60% vs. 46%, p = 0.04); question Q10, which asked about the management of fever, skin rash and dyspnea in autologous HCT (67% vs. 49%, p = 0.01); question Q14 (primary therapy of invasive aspergillosis, 88% vs. 75%, p = 0.02), and; question Q15 (skin nodules representing the first clinical manifestation of invasive fusariosis (78% vs. 65%, p = 0.05).
We also observed a significant difference in the median scores by age group: 5.0 (range 2.0 - 8.0) for clinicians < 30 years old, 5.0 (range 1.5 - 9.0) for those between 31 and 40 years old, 4.5 (range 0.5 - 8.0) for those between 41 and 50 years, 4.0 (range 1.5 - 7.5) for those between 51 and 60 years and 3.0 (range 1.5 - 6.5) for clinicians > 60 years old (p < 0.001).
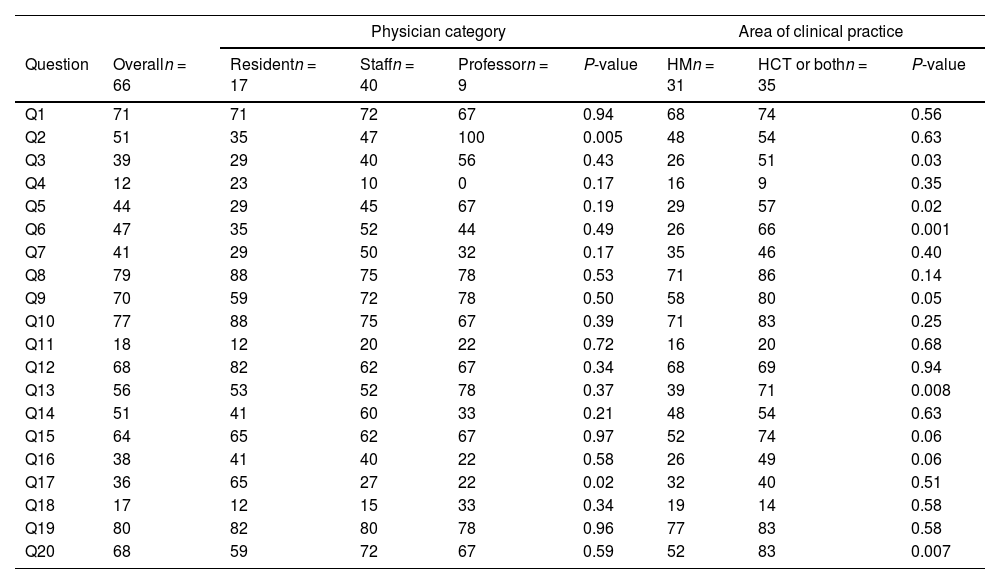
Survey 2: infectious complications in HCTThe 20 questions of survey 2 covered topics on bacterial (6 questions), fungal (7 questions) and viral (7 questions) infections. As shown in Table 3, among the three questions with the lowest percentages of correct answers, two tested the knowledge of clinicians on the management of cytomegalovirus (CMV) infection in HCT (Q4, 12% and Q11, 18%), the third being on the treatment of IFDs (Q18, 17%), and most respondents did not know that isavuconazole is an option for the primary treatment of mucormycosis. On the other hand, questions on the correct diagnosis of bacterial infections and antibiotic use had the highest percentages of correct answers: 80% in Q19 (proper diagnosis and management of neutropenic enterocolitis), 79% in Q8 (no activity of meropenem against methicillin-resistant Staphylococcus aureus) and 77% in Q10 (engraftment syndrome post autologous HCT).
Percentage of correct answers in survey 2 (infection in hematopoietic cell transplantation) regarding physician category and main area of clinical practice.
HM = hematologic malignancy; HCT = hematopoietic cell transplantation.
When we analyzed the scores across different groups, no statistically significant difference was observed, when comparing staff clinicians, residents and professors (5.0, range 0.5 - 9.0, 5.0, range 3.0 - 6.5, and 4.5, range 3.5 - 8.5, respectively, p = 0.93). However, looking at individual questions, some differences were observed (Table 3). In Q2 (positive blood culture for C. krusei), all nine professors answered correctly, compared to 47% of staff clinicians and 35% of residents (18%, p = 0.005).
Comparing clinicians working with HCT or HM only, the median scores were 6.0 (range 3.5 – 9.0) and 4.5 (range 0.5 – 9.0), respectively (p = 0.002). In three questions regarding viral infections, clinicians working with HCT had higher scores. These questions were Q6 (herpes zoster as the most frequent viral infection in the post-engraftment period of autologous HCT, 66% vs. 26%, p = 0.001), Q9 (risk factors for EBV reactivation, 80% vs. 58%, p = 0.05) and Q20 (respiratory viruses in allogeneic HCT, 83% vs. 52%, p = 0.007). Other questions with significant differences were Q13 (positive blood culture for a mold, 71% vs. 39%, p = 0.008), Q3 (risk factor for invasive aspergillosis after HCT, 51% vs. 26%, p = 0.03) and Q5 (causes of diffuse infiltrates in allogeneic HCT, 57% vs. 29%, p = 0.02).
Analyzing age groups, the median scores were: 5.0 (range 3.0 - 6.5) for those aged ≤ 30 years, 5.5 (range 1.0 - 9.0) for those between 31 and 40 years, 5.0 (0.5 - 8.5) for those between 41 and 50 years, 5.5 (range 2.5 - 7.5) for those between 51 and 60 years and 5.0 (range 4.5 - 5.5) for clinicians > 60 years old, p = 0.68.
DiscussionIn the present study, we observed that hematologists with daily practice in managing febrile neutropenia and infection in HCT had a low overall score, reflecting the urgent need for continuous education. In general, we identified gaps in the management of all types of infection (bacterial, fungal and viral), with wrong answers in diagnosis, treatment and prophylaxis.
Other studies have addressed the use of surveys to evaluate the level of the physician knowledge in different scenarios.9-12 This type of study is of great importance to identify gaps in the knowledge, helping to tailor educational activities to a certain community of physicians. Regarding infection in hematology, two studies used surveys to evaluate the practices of antimicrobial management in adults and children.13,14
Our study focused only on hematologists working with HM and HCT, yielding several findings regarding gaps in the knowledge of infectious complications. In survey 1, we observed that most clinicians did not know that the dose of betalactam antibiotics should be calculated on the basis of weight and creatinine clearance (Q3).15 In this regard, the use of a fixed dose may result in overexposure to the antibiotics, increasing the risks of adverse events, or underexposure, resulting in poor response to infection. We also noted a gap in the knowledge regarding the epidemiology of bacterial infections, as most clinicians were not aware that patients receiving high doses of cytarabine are at higher risk of developing viridans streptococci bacteremia. These bacteria are colonizers of the oral cavity and the presence of mucositis induced by high-dose cytarabine increases the risk of bloodstream infection by this pathogen.16,17
We also observed that clinicians had the mistaken idea that secondary antifungal prophylaxis is needed in all IFDs. The majority answered that secondary prophylaxis is indicated for patients with a previous episode of candidemia, when in fact, there is no data to indicate that secondary prophylaxis is needed.18 On the other hand, 80% of clinicians were aware that a positive blood culture for yeast in a patient with febrile neutropenia should prompt the immediate initiation of appropriate antifungal therapy.
In survey 2, the questions with the lowest rate of correct answers were on CMV infection, which might reflect the heterogeneity in current clinical practices across different institutions. In Q4, almost 30% of clinicians did not know that ganciclovir increases the risk of bacterial and fungal infection19 and 43% did not know that acyclovir at high doses may prevent CMV infection.20 Another aspect that deserves attention is the CMV surveillance in allogeneic HCT, as only 18% answered question Q11 correctly. The CMV surveillance after allogeneic HCT should be performed weekly, at least until day +100, and should be extended beyond day +100 in patients with graft-versus-host disease. Our survey also identified a gap in knowledge on new drugs to treat IFDs (Q7 and Q18). Isavuconazole is a broad-spectrum azole approved as primary therapy for both invasive aspergillosis and mucormycosis.21
Finally, we found some differences in knowledge when we analyzed scores across groups. In both surveys, although we did not find a statistically significant difference in overall scores between staff clinicians, residents and professors, we observed that in individual questions, staff clinicians seemed to have more experience than residents and professors. This might be explained by the fact that staff clinicians attend to a larger number of patients, which gives them more expertise. Furthermore, as we expected, hematologists working in both areas (HCT and HM) had the highest score. In addition, if we look into individual questions, hematologists working with HCT had the highest percentage of adequate answer regarding viral infections, probably because CMV and EBV infections are more common in this setting. Age groups were also analyzed and, in survey 1, we observed that clinicians < 40 years of age had the highest scores, probably reflecting the fact that younger hematologists, having graduated recently, may be more updated with new information.
In our survey, the questions and the selection of the correct answers were made by one of the authors, based on his personal experience in managing infection in hematologic patients in Brazil over 30 years. This likely reduced potential influences of local epidemiologic differences on the selection of correct answers by the participants.
A major limitation of our study is that since the participation was voluntary, clinicians with less expertise could have declined the invitation. In this regard, it is possible that the overall score could be even lower if there was no selection bias. Moreover, we did not have the information about the number of years of experience of clinicians in treating patients with HM and/or undergoing HCT.
ConclusionIn conclusion, our study allowed us to identify important gaps in the knowledge of Brazilian hematologists regarding the management of infectious complications in patients undergoing chemotherapy or HCT. These data indicate that there is an urgent need for continuous medical education in the field, as well as guidance for management of infection which takes into account local epidemiologic aspects. In this regard, the development of Brazilian guideline for the management of febrile neutropenia and the creation of an educational program addressing the management of infection in hematologic patients may improve clinician knowledge and patient care.
This study was presented in part at the European Hematology Association (EHA) Congress 2022 in June, Vienna, Austria.