Blood transfusion-transmitted infections in individuals suffering from beta-thalassemia have been reported in Pakistan, but the information on their sociodemographic and clinical determinants is lacking. This study aims to describe the prevalence, as well as the factors, contributing in blood transfusion-transmitted infections.
MethodBetween December 2011 and December 2013, in a non-probable sampling, 350 thalassemia patients were recruited in Lahore, Multan, Karachi and Peshawar, Pakistan. Subjects were screened for transfusion-transmitted infections.
ResultsA seropositive rate of 36.5% was observed; males (94, 73.4%) and females (34, 26.6%). Among several risk factors associated with transfusion-transmitted infections, province (p=0.001), gender (p=0.003), age (p<0.03), education (p<0.00), degree of consanguinity (p=0.05), age at fetal blood test (p=0.005), fetal hemoglobin levels (p=0.005), death due to thalassemia (p=0.001) and iron-related complications (p=0.04) showed significant correlation. Participants with an age >10 years were significantly more prone to seropositivity than those aged ≤10 years. Moreover, the ferritin level was also significantly higher in those aged >10 years than in those ≤10 years. It was observed that males had a higher seroprevalence rate (94, 73.4%) than females (34, 26.6%). The most prevalent transfusion-transmitted infections was the hepatitis C virus, with 115 cases (89.8%).
ConclusionA high prevalence rate of HCV in subjects with transfusion-dependent thalassemia is linked with insufficient facilities, poor management and compromised socioeconomic status. Therefore, more multicenter studies covering cities from different regions of the country are needed in order to develop preventive measurements at the regional and national level.
An estimated 1.5% of the global population are thalassemia carriers, with varying clinical heterogeneity.1 Thalassemia is considered a major public health problem in Pakistan, with a carrier rate of approximately 5%. Over 5000 new cases of beta-thalassemia major (TM) are diagnosed annually.2 In an approximate population of 182 million people in Pakistan, there are six major ethnic groups: Punjabi (53.5%), Pashtun (Pathan) (15%), Sindhi (14%), Muhajirs (7.5%), Balochi (3.5%) and others (6.5%).3
The hepatitis B virus (HBV) and hepatitis C virus (HCV) are the most common transfusion-transmitted infectious agents which became known in 1963 and 1975, respectively.4 Globally,2 billion people are positive for HBV. The World Health Organization (WHO) has declared South Asia as a high-risk area for HCV, with a prevalence rate of 2.1%.5 In Pakistan, the prevalence rate of HBV is 3–5% and of HCV, 4–5%.6 The asymptomatic spread via parental transmission is the root cause of its transmission in early childhood. There is a strong belief that lack of implementation of international standards for blood transfusion and its practices, including syringes and shared equipment, such as shaving kits, and percutaneous injuries are the main contributors toward their widespread infection.7
Failure in the prevention of thalassemia has resulted in an ever-growing demand for blood transfusions. High transfusions rates increase TTI risks, thereby limiting the life expectancy.8,9 Limited resources and lack of awareness are constantly hindering the improvement in the current alarming situation. Therefore, better practices in both governmental and private sectors are required. A national vaccination campaign against HBV has been initiated, principally at the neonatal level, with approximately 73% of the neonates having been vaccinated.10 Frequent vaccination is an utmost necessity for its prevention, but unfortunately, scarce studies have been reported to date from rural areas of Pakistan.8,9,11 In thalassemia major, regular blood transfusion is required to keep a pre-transfusion hemoglobin (Hb) level at 9–10.5g/dL.12 Therefore, iron chelation therapy is obligatory to avoid fatal organ damage.
The WHO has reported an approximate 1.5 million annual blood transfusions in Pakistan.13 It is our social dilemma that most of the donors hide their health status from relatives and willingly contribute to blood donation. However, donors must be repeatedly checked for negative results for bloodborne pathogens.8 Careful selection criteria for donors, proper blood screening and standardized safe procedures for blood storage and maintenance are some of the measures that can be adopted to minimize viral transmissions. Although public health authorities are raising awareness among the general and high-risk populations, with the assistance of electronic and print media, yet these efforts are not practiced in most Pakistani rural areas.9,11,14 Therefore, this study, in addition to determining the seroprevalence, also aims to identify those sociodemographic and clinical pitfalls that have contributed to the persistent prevalence of TTIs, regardless of the presence of safe transfusion guidelines.
Materials and methodsStudy populationA non-probable sampling was made for this study. Initially, 350 thalassemia major subjects of different age groups were recruited from transfusion centers in Lahore, Multan, Karachi and Peshawar (162 from Lahore, 64 from Multan, 71 from Karachi and 53 from Peshawar) between December 2011 and December 2013. At these centers, instead of whole blood, specific blood components (red cells) are transfused at an optimized dose, using Thalassemia International Federation guidelines. Red cells are stored at an optimum temperature (4°C). This study was performed according to the World Medical Association (Declaration of Helsinki) code of ethics. Approval for this study was obtained from the Ethics committee of the School of Biological Sciences, University of the Punjab, Lahore, Pakistan.
Primary analysisParticipants were primarily selected based on inclusion and exclusion criteria. Participants diagnosed with TM that were registered at a blood transfusion center were included. Any participant who was non-thalassemic, reluctant to participate, transfusion-independent or in necessity of less than 6 RBC transfusions per year and/or who had severe clinical conditions that made him/her unavailable for the study was excluded. An informed consent was obtained from the subjects or from their parents/attendants before the blood collection.
Blood sample analysisBlood samples were collected from thalassemia subjects following the standard procedure of the National Committee for Clinical Laboratory Standards (NCCLS).15 All subjects were screened for the presence of antigens or antibodies for HBV, HCV and the human immunodeficiency virus (HIV), using the one-step device (Acu-check®), as per the manufacturer guidelines. These are simple, easy and ready-to-use immune chromatographic tests (ICTs). The results were recorded by visually observing the color change in membrane-based kits, depending upon the presence or absence of antibodies or antigens, with a sensitivity of 1ng/mL.
Demographic and clinical analysisA questionnaire was designed to collect information on demographic traits (i.e., age, gender, origin, ethnicity, etc.), the clinical picture (i.e., type of thalassemia, age of diagnosis, number of blood transfusions and medical complications) and the family history (i.e., parental consanguinity, number of thalassemia subjects in the family and morbidity and mortality of the sibship with thalassemia).
Statistical analysisData was analyzed by both descriptive and analytic statistics, using the ANOVA, SPSS version 20.0. Baseline characteristics of participants were described as percentages. A p-value less than 0.05 was considered as significant. Subjects were studied across different time frames by dividing the whole sample into two groups; one with ≤10 years of age and the other one with >10 years of age and subcategorizing them into seropositive and seronegative samples. This strategy will be helpful in highlighting the persistent causes and outcomes of precautionary health measures taken against TTIs over the course of time.
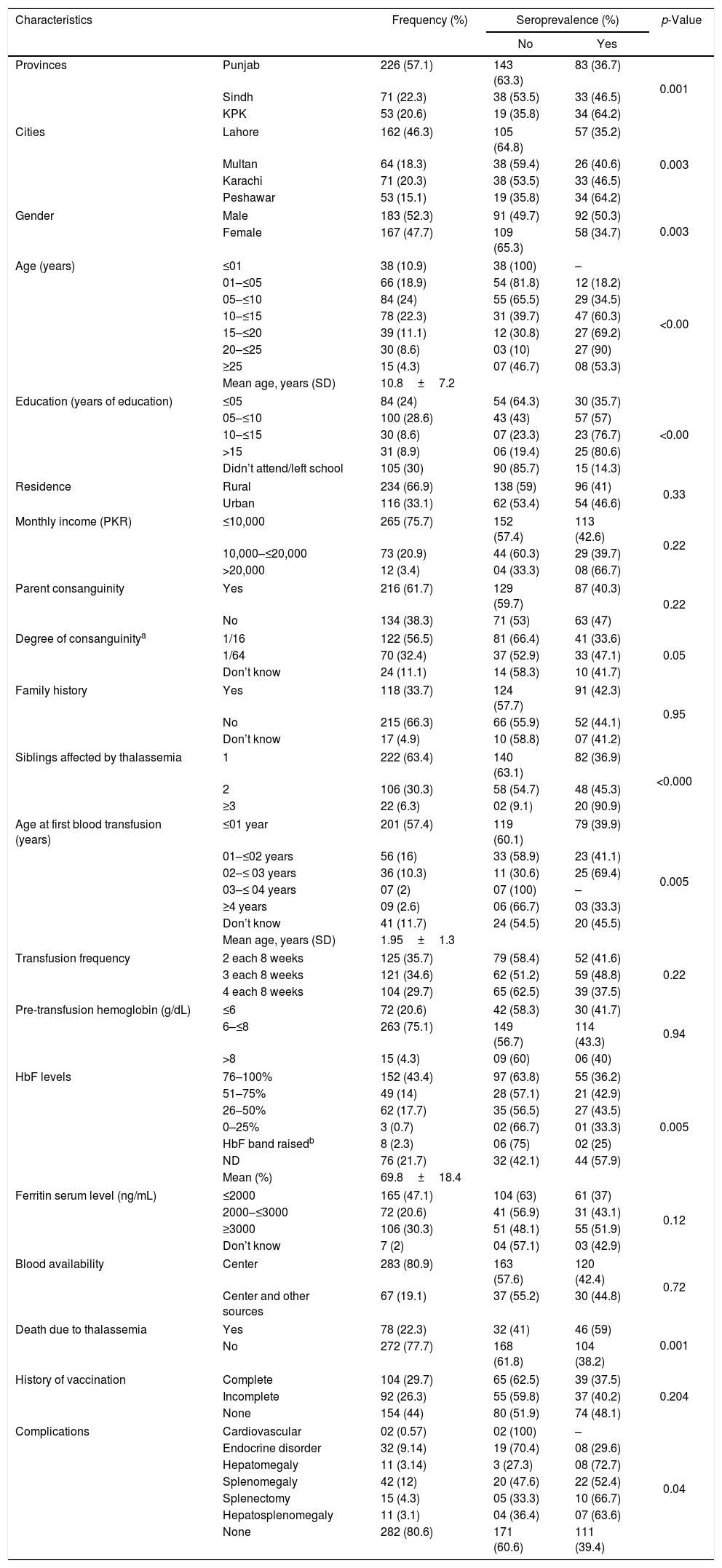
ResultsDemographic dataThe general characteristics of the population studied are presented in Table 1. Among the 350 regularly transfused beta-thalassemia subjects, 183 (52.3%) were male. Their mean age was 10.8±7.2 years (minimum 0.5 years old; maximum 28 years old). A total of 226 (57.1%) individuals belonged to the Punjab ethnic group (46.3%% from Lahore; 18.3% from Multan), 71 (22.3%), to the Sindh (Karachi only) and 53 (20.6%), to the Khyber Pakhtunkhwa (KPK) (Peshawar only). Nearly half of the subjects (46.3%) were 6–10 years old and most had 10 years of educations (28.6%). A total of 234 subjects (66.9%) belonged to the rural area. A total of 265 (75.7%) had a low income of ≤10,000 Pakistani rupees (PKR) (75.7%). A high parental consanguinity rate (61.7%) was observed, with an almost equal degree of consanguinity rate, i.e. 1/16 (56.5%) and 1/64 (32.4%), respectively. There were 215 subjects (66.3%) who have no previous family history of thalassemia. However, 17 (4.9%) did not have knowledge of their previous family history. Most families (63.4%) had only the proband as a thalassemic patient.
Distribution of sociodemographic and clinical features in seronegative and seropositive thalassemia participants.
| Characteristics | Frequency (%) | Seroprevalence (%) | p-Value | ||
|---|---|---|---|---|---|
| No | Yes | ||||
| Provinces | Punjab | 226 (57.1) | 143 (63.3) | 83 (36.7) | 0.001 |
| Sindh | 71 (22.3) | 38 (53.5) | 33 (46.5) | ||
| KPK | 53 (20.6) | 19 (35.8) | 34 (64.2) | ||
| Cities | Lahore | 162 (46.3) | 105 (64.8) | 57 (35.2) | 0.003 |
| Multan | 64 (18.3) | 38 (59.4) | 26 (40.6) | ||
| Karachi | 71 (20.3) | 38 (53.5) | 33 (46.5) | ||
| Peshawar | 53 (15.1) | 19 (35.8) | 34 (64.2) | ||
| Gender | Male | 183 (52.3) | 91 (49.7) | 92 (50.3) | 0.003 |
| Female | 167 (47.7) | 109 (65.3) | 58 (34.7) | ||
| Age (years) | ≤01 | 38 (10.9) | 38 (100) | – | <0.00 |
| 01–≤05 | 66 (18.9) | 54 (81.8) | 12 (18.2) | ||
| 05–≤10 | 84 (24) | 55 (65.5) | 29 (34.5) | ||
| 10–≤15 | 78 (22.3) | 31 (39.7) | 47 (60.3) | ||
| 15–≤20 | 39 (11.1) | 12 (30.8) | 27 (69.2) | ||
| 20–≤25 | 30 (8.6) | 03 (10) | 27 (90) | ||
| ≥25 | 15 (4.3) | 07 (46.7) | 08 (53.3) | ||
| Mean age, years (SD) | 10.8±7.2 | ||||
| Education (years of education) | ≤05 | 84 (24) | 54 (64.3) | 30 (35.7) | <0.00 |
| 05–≤10 | 100 (28.6) | 43 (43) | 57 (57) | ||
| 10–≤15 | 30 (8.6) | 07 (23.3) | 23 (76.7) | ||
| >15 | 31 (8.9) | 06 (19.4) | 25 (80.6) | ||
| Didn’t attend/left school | 105 (30) | 90 (85.7) | 15 (14.3) | ||
| Residence | Rural | 234 (66.9) | 138 (59) | 96 (41) | 0.33 |
| Urban | 116 (33.1) | 62 (53.4) | 54 (46.6) | ||
| Monthly income (PKR) | ≤10,000 | 265 (75.7) | 152 (57.4) | 113 (42.6) | 0.22 |
| 10,000–≤20,000 | 73 (20.9) | 44 (60.3) | 29 (39.7) | ||
| >20,000 | 12 (3.4) | 04 (33.3) | 08 (66.7) | ||
| Parent consanguinity | Yes | 216 (61.7) | 129 (59.7) | 87 (40.3) | 0.22 |
| No | 134 (38.3) | 71 (53) | 63 (47) | ||
| Degree of consanguinitya | 1/16 | 122 (56.5) | 81 (66.4) | 41 (33.6) | 0.05 |
| 1/64 | 70 (32.4) | 37 (52.9) | 33 (47.1) | ||
| Don’t know | 24 (11.1) | 14 (58.3) | 10 (41.7) | ||
| Family history | Yes | 118 (33.7) | 124 (57.7) | 91 (42.3) | 0.95 |
| No | 215 (66.3) | 66 (55.9) | 52 (44.1) | ||
| Don’t know | 17 (4.9) | 10 (58.8) | 07 (41.2) | ||
| Siblings affected by thalassemia | 1 | 222 (63.4) | 140 (63.1) | 82 (36.9) | <0.000 |
| 2 | 106 (30.3) | 58 (54.7) | 48 (45.3) | ||
| ≥3 | 22 (6.3) | 02 (9.1) | 20 (90.9) | ||
| Age at first blood transfusion (years) | ≤01 year | 201 (57.4) | 119 (60.1) | 79 (39.9) | 0.005 |
| 01–≤02 years | 56 (16) | 33 (58.9) | 23 (41.1) | ||
| 02–≤ 03 years | 36 (10.3) | 11 (30.6) | 25 (69.4) | ||
| 03–≤ 04 years | 07 (2) | 07 (100) | – | ||
| ≥4 years | 09 (2.6) | 06 (66.7) | 03 (33.3) | ||
| Don’t know | 41 (11.7) | 24 (54.5) | 20 (45.5) | ||
| Mean age, years (SD) | 1.95±1.3 | ||||
| Transfusion frequency | 2 each 8 weeks | 125 (35.7) | 79 (58.4) | 52 (41.6) | 0.22 |
| 3 each 8 weeks | 121 (34.6) | 62 (51.2) | 59 (48.8) | ||
| 4 each 8 weeks | 104 (29.7) | 65 (62.5) | 39 (37.5) | ||
| Pre-transfusion hemoglobin (g/dL) | ≤6 | 72 (20.6) | 42 (58.3) | 30 (41.7) | 0.94 |
| 6–≤8 | 263 (75.1) | 149 (56.7) | 114 (43.3) | ||
| >8 | 15 (4.3) | 09 (60) | 06 (40) | ||
| HbF levels | 76–100% | 152 (43.4) | 97 (63.8) | 55 (36.2) | 0.005 |
| 51–75% | 49 (14) | 28 (57.1) | 21 (42.9) | ||
| 26–50% | 62 (17.7) | 35 (56.5) | 27 (43.5) | ||
| 0–25% | 3 (0.7) | 02 (66.7) | 01 (33.3) | ||
| HbF band raisedb | 8 (2.3) | 06 (75) | 02 (25) | ||
| ND | 76 (21.7) | 32 (42.1) | 44 (57.9) | ||
| Mean (%) | 69.8±18.4 | ||||
| Ferritin serum level (ng/mL) | ≤2000 | 165 (47.1) | 104 (63) | 61 (37) | 0.12 |
| 2000–≤3000 | 72 (20.6) | 41 (56.9) | 31 (43.1) | ||
| ≥3000 | 106 (30.3) | 51 (48.1) | 55 (51.9) | ||
| Don’t know | 7 (2) | 04 (57.1) | 03 (42.9) | ||
| Blood availability | Center | 283 (80.9) | 163 (57.6) | 120 (42.4) | 0.72 |
| Center and other sources | 67 (19.1) | 37 (55.2) | 30 (44.8) | ||
| Death due to thalassemia | Yes | 78 (22.3) | 32 (41) | 46 (59) | 0.001 |
| No | 272 (77.7) | 168 (61.8) | 104 (38.2) | ||
| History of vaccination | Complete | 104 (29.7) | 65 (62.5) | 39 (37.5) | 0.204 |
| Incomplete | 92 (26.3) | 55 (59.8) | 37 (40.2) | ||
| None | 154 (44) | 80 (51.9) | 74 (48.1) | ||
| Complications | Cardiovascular | 02 (0.57) | 02 (100) | – | 0.04 |
| Endocrine disorder | 32 (9.14) | 19 (70.4) | 08 (29.6) | ||
| Hepatomegaly | 11 (3.14) | 3 (27.3) | 08 (72.7) | ||
| Splenomegaly | 42 (12) | 20 (47.6) | 22 (52.4) | ||
| Splenectomy | 15 (4.3) | 05 (33.3) | 10 (66.7) | ||
| Hepatosplenomegaly | 11 (3.1) | 04 (36.4) | 07 (63.6) | ||
| None | 282 (80.6) | 171 (60.6) | 111 (39.4) | ||
ND: not determined; KPK: Khyber Pakhtunkhwa; SD: standard deviation; PKR: Pakistani currency.
During the first years of age (mean age of 1.95±1.3 years; minimum 1 year; maximum 6 years), 201 (57.4%) subjects received their first red blood cell (RBC) transfusion (Table 1). The patient RBC transfusion occurred every eight weeks, with 125 (35.7%) receiving 2 RBC units and 121 (34.6%) receiving 3 RBC units. A comparative proportion of 104 subjects (29.7%) had 4 transfusions every 8 weeks to maintain the pre-transfusion Hb level at ≥8g/dL. Similarly, only a small number of subjects, i.e. 15 (4.3%) had pre-transfusion Hb above 8g/dL, while 263 (75.1%) subjects had 6–8g/dL, indicating their high transfusion demands. The mean fetal hemoglobin (HbF) was 69.8±18.4%, ranging from 23% to 100%. One hundred and fifty-two subjects (43.4%) had an HbF level between 76 and 100%. Unfortunately, 76 (21.7%) had no record of their HbF levels. The ferritin level in 165 (47.1%) subjects was ≤1000 and in 106 (30.3%) subjects, it was ≥3000ng/mL. Only one transfusion center had free blood availability, while at other three centers, access to blood was limited (61.4%) and they had to seek their own blood donors. Deaths due to thalassemia in the family were reported for 78 (22.3%) subjects. Unfortunately, the vaccination situation for HCV is not very good. Vaccination is available only for HBV. However, 154 (44%) subjects had not started vaccination yet, either because they were too young to start vaccination, or because they were subject to financial instability. Only 104 (29.1%) subjects had completed their vaccination course and 59 (16.9%) had incomplete vaccination status. As there is no HCV vaccine available, the risk of HCV infection has increased.
Frequent transfusion with irregular iron chelation therapy increases the likelihood of the iron overload-related complications. Thirty-two subjects (9.14%) had endocrine disorders (short stature and/or delayed puberty). Other complications reported were: cardiovascular problems (0.57%), hepatomegaly (3.14%), splenectomy (4.3%), splenomegaly (12%) and hepatosplenomegaly (3.1%).
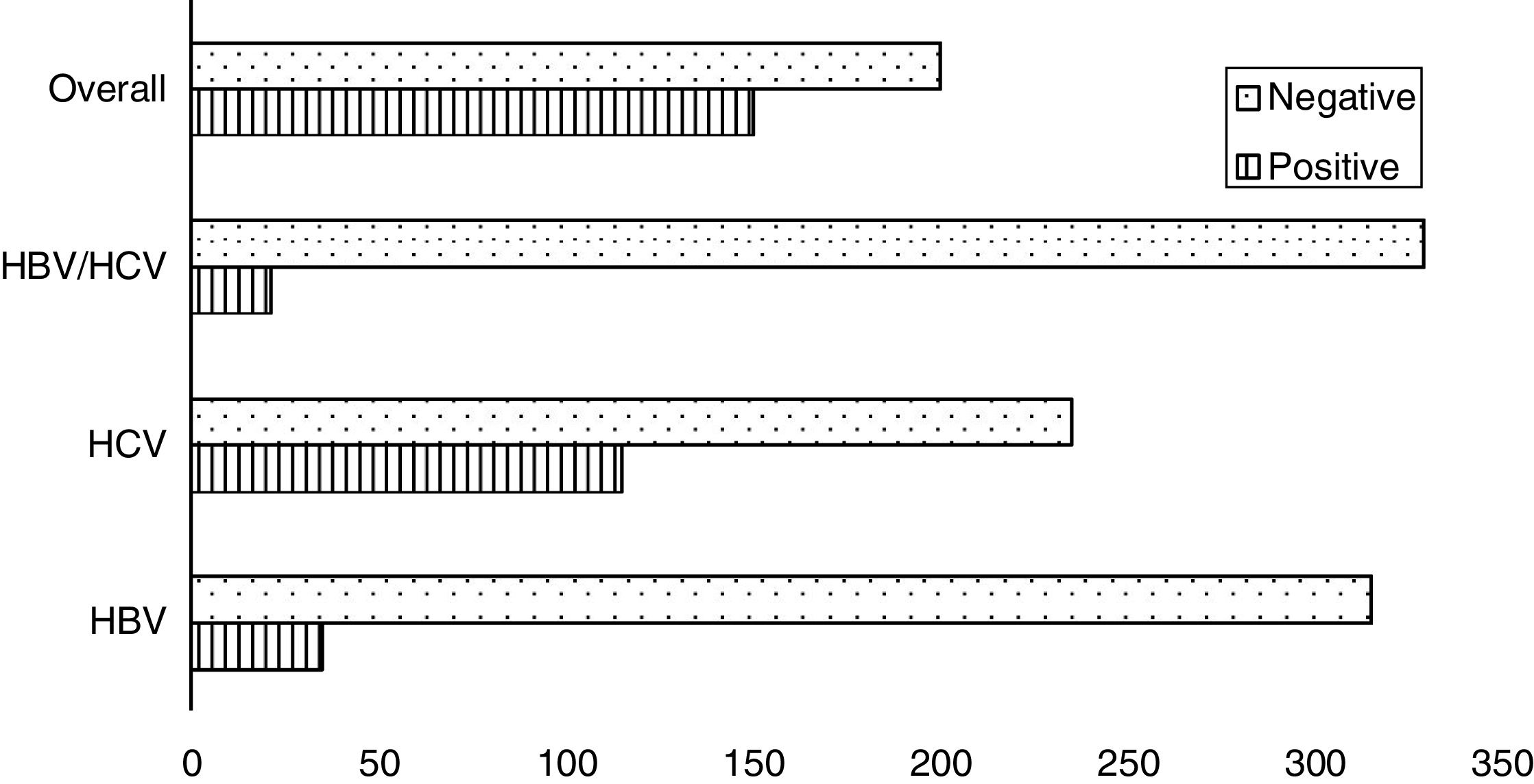
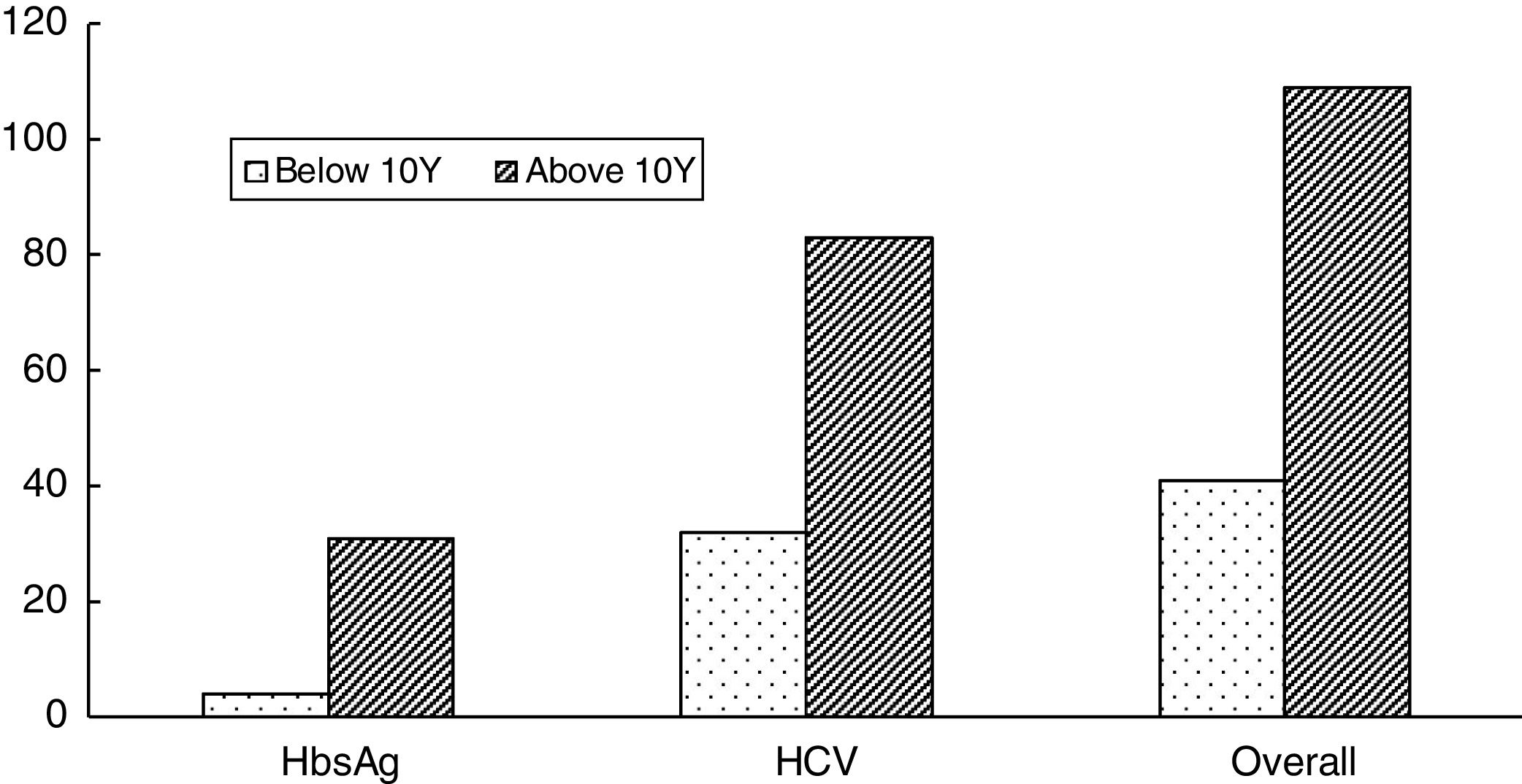
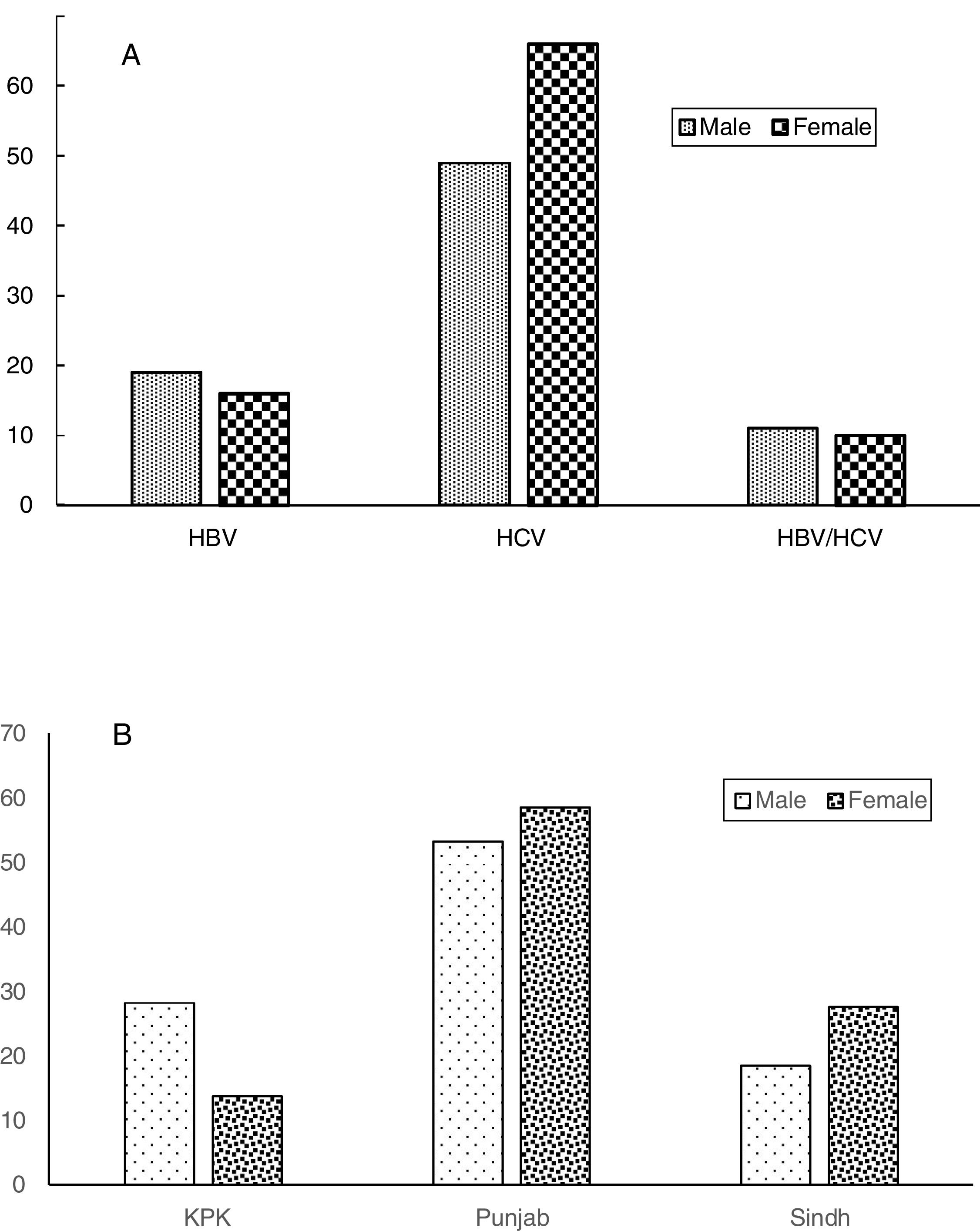
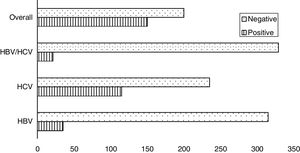
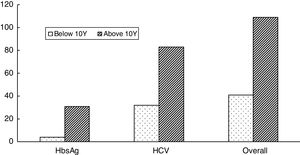
Seroprevalence dataAmong the 350 transfusion-dependent thalassemia (TDT) subjects, 150 (42.8%) were seropositive; HBV infected (26, 7.4%), HCV infected (103, 29.4%) and co-infected (21, 6%). The prevalence of HBV infection was lower than that of HCV infection (Figure 1). This small number can be attributed to the availability of the vaccine against HBV. When the sociodemographic and clinical features of the study subjects were distributed based on the presence and absence of hepatitis infection, a statistically significant relationship between seroprevalence and province (p=0.001) was found (Figure 2). High seroprevalence rates were present in KPK (64.2%), followed by Sindh (46.5%) and Punjab (36.7%). Interestingly, males (50.3%) were significantly more seropositive than females (34.7%) (p=0.003) (Figure 3). A significant increase in older subjects was present, when observed across different age groups (p<0.000). It was observed that the seroprevalence was high in probands that have other siblings suffering from thalassemia, e.g. a frequency of 90.9% in subjects having ≥3 siblings suffering from thalassemia, compared to 36.9% in subjects who were the only affected child (36.9%) (p-value<0.000). This elevated risk of trans-transmission among family members also indicates the poor hygienic practices that have also contributed toward the failure in prevention of seroprevalence. It was seen that seroprevalence was significantly distributed in the different age groups in which the first blood transfusion (FBT) occurs (p=0.005). Similarly, a significant difference in the degree of consanguinity (p=0.05) and iron-related complications (p=0.04) were also present.
Inadequate blood screening is considered the main source of TTIs. Unfortunately, no statistically significant difference was observed between subjects who receive blood solely from transfusion centers and those who receive blood from cenetes, as well as from personal donors. This may be due to the small sample size and unequal distribution of samples in our study. Subjects who had a history of familial death due to thalassemia had a seropositive rate significantly higher (59%) than the subjects with no previous history (38.2%). Liver- (72.7%) and spleen- (52.4%) related complications (hepatomegaly and splenomegaly) had a higher seropositive ratio, compared to other complications, i.e. cardiovascular and endocrine (29.6%), as well as being significantly related to the seroprevalence (p=0.04). In subjects ≤10 years of age, there was a significant decrease in the number of deaths (p=0.001), degree of consanguinity (p=0.05) and gender differences (p=0.03) (Figure 2). Moreover, in recent years the number of consanguine marriages has decreased to 22.2% (for the group of individuals>10 years) from 45.7% (for the group of individuals>10 years).
DiscussionThalassemia is the prevailing single-gene disorder in more than 60 countries in the world. Regular transfusion is the only available approach, in addition to bone marrow transplantation (BMT). Inefficacy in preventing thalassemia has been constantly increasing the demand for blood transfusions and therefore, the chances of developing TTIs, as well.8,9 The risk of TTIs is the main concern for both practitioners and subjects. As recommended by the World Health Organization (WHO), the screening of blood or blood products should be performed at least for HCV, HIV, HBV, malarial parasites and syphilis.13,16 There are not many studies from Pakistan that determine the TTI seroprevalence rates and their contributing factors. Therefore, a multicenter study representing different localities and analyzing them for various aspects would be of interest in awareness regarding the functionality of blood safety measures. Seroprevalence rates of 10% for HBV and 32.9% for HCV were comparable to those of previous studies.8,9,14,17 The incidence rates can be correlated with the fact that, due to transfusion, TDT subjects are usually more prone to HBV infections. However, with the advances in HBV vaccination, a dramatic decrease in the global incidence rate has occurred.9,14,18
Statistically significant (p=0.001) differences among seroprevalence rates in different provinces support the earlier findings that different ethnicities and cultures and their underlying differences are also considered as risk factors.19,20 In the present study, the prevalence of TTIs in all three provinces might be due to poor hygienic and health conditions at home.21 A high consanguinity rate is one of the substantial factors in the spread of thalassemia. Resembling the previous reports, this study also observed that males (51.4%) were significantly (p-value=0.003) more affected than females (20.4%). A high prevalence of viral infections is due to the poor provision of basic necessities, particularly access to clean water and proper sanitary setups for common people.18,22
The presence of hepatitis infection puts obvious financial strain on the families. The elevated risk of trans-transmission among family members was similar to that previously reported by Din et al.,9 and Qurat-ul-Ain et al.,23. Likewise, Saeed et al.,17 found that the first child in a family suffering from thalassemia was seropositive in a higher number of instances. Thalassemia subjects coming for transfusion at the different transfusion centers in Pakistan were initially screened for seroprevalence.
The TTI seroprevalence was higher in individuals at a transfusion center that was not self-sufficient in its blood supply. This is due to the fact that blood is supplied by volunteer donors (replacement donors), in most cases close relatives. This frequent practice may have played a vital role in TTIs. Behavior-based donor selection will be helpful in sensibly minimizing this risk. Therefore, repetitive negative screening for TTIs in blood donors should be included. Unfortunately, all of these practices rely on the honest disclosure of risk behavior, putting aside all fear of stigmatization. Therefore, in addition to assessing TTIs, measures should also target the awareness, attitude and behavior of blood donors and recipients. This will be helpful in setting special measurements and priorities, according to region studied, for the implementation of preventive strategies. This would ultimately improve the public health and, hence, would lead to a rise in blood safety and quality for donors, recipients and transfusion centers.20,21 The low rate (78, 22.3%) of thalassemia-related deaths in family histories reflects the insufficient public awareness of the clinical picture of thalassemia in past.
A comparatively high demand for transfusion is due to poor clinical management, increased iron overload, splenomegaly, very distant transfusion centers and/or an inadequate blood supply. As reported in previous studies, seroprevalence in our study was high in subjects ≥10 years of age due to an increased transfusion frequency leading to iron-related complications.9,17 High transfusion frequency (p=0.043) and increased ferritin levels (p=0.003) are significantly associated with TTI seropositivity, as also observed in earlier studies.8 A major improvement in the public sector is thus required. Implementation of good practices along with increased public awareness will subsequently lessen the TTI burden, as it was observed that the number of seropositive subjects was lower in the ≤10 years of age group compared to the ≥10 years age group. However, it is also a fact that the low number of transfusions in the ≤10 years old of age group compared to the ≥10 years old contributed to the low frequency of TTIs. Meanwhile, productive outcomes are turning up, such as the adoption of the HBV screening program initiative in 1994, which was evidenced by the decreased number of cases reported in a group of subjects with FBT at age ≤10 years.9,14 Similarly, with frequent transfusions (4/8 weeks), the number of thalassemia subjects with HCV and/or HBV infections has increased twofold, but this association was non-significant.17
The results in the present study were in accordance with previous reports, however minor differences could be due to the sample size, region studied and blood source availability and systems implemented for its screening and transfer to the subjects. The differences can be attributed to the confidence interval (CI) that is not narrow. Asymptomatic spread via parental transmission is the main transmission route in early childhood. In addition, lack of implementation of international standards in blood transfusion and its practices, unsterilized syringes, shared equipment, such as shaving kits, and percutaneous injuries have also contributed to its widespread occurrence.8,11 In the absence of any available treatment for thalassemia, standardized health codes assure better health settings. TTI-infected subjects must be periodically monitored and awareness campaigns must be conducted to increase understanding of the epidemiological pattern and risk associated with its spread.8
ConclusionThe HCV is the most prevalent TTI in thalassemia major in our study. Therefore, a self-sufficient and safe blood supply with improved blood screening and donor selection is required to minimize TTIs.Furthermore, raising awareness with the assistance of electronic and printed media will also be beneficial.
Conflicts of interestThe authors declare no conflicts of interest.
The authors thanks Imran Qadeer, Syed Waseem Qadri, medical staff of transfusion centre and participants who gave their in blood sample. This work is the part of thesis of Ms. Humaira Yasmeen.