The safety of a blood transfusion practice is anchored on safe blood from a healthy donor, while further protecting the donor from future harm. This study aimed to evaluate the hematological parameters of blood donors in view of their donor category to aid in assessing the safety threshold in terms of donation frequency.
MethodsThis study made use of the descriptive cross-sectional design. The blood donors were bled and their samples analyzed using a hematology autoanalyzer.
ResultsA total of 178 male blood donors were recruited. Most of the donors were aged 18 to 39 years and were mostly students. A greater part of them were repeat donors who had donated blood more than four times. First- and second-time donors constituted the majority of the voluntary donors. While the total red cell count was significantly lower in repeat third-time donors, the hemoglobin and hematocrit of the first-time donors were significantly higher than those of the repeat fourth-time donors. The mean corpuscular hemoglobin (MCH) and mean corpuscular hemoglobin concentration (MCHC) of the first-time donors were significantly higher than those of the repeat fifth-time donors. The red cell distribution width (RDW) and mean platelet volume (MPV) were significantly lower in the first-time donors from those of the sixth- and seventh-time donors, respectively. Most of the fifth-time donors have subclinical anemia. There was more subclinical anemia in commercial donors than in voluntary donors.
ConclusionRepeat donors more than fifth-time donors are at risk of donation-induced iron deficiency anemia.
Blood transfusion is an essential component of the health care system of every country and plays a pivotal role in medical and surgical management of patients.1,2 The practice hinges on the provision of safe blood from a healthy donor to the patient.3,4 In Nigeria, blood banks routinely test prospective donors for infections, such as hepatitis B and C, HIV and syphilis.5,6,7 The only hematological analysis routinely performed for screening prospective donors is hemoglobin (Hb) or packed cell volume (PCV)/hematocrit. The effectiveness of the transfusion process depends on the quality of the blood transfused and the safety of the donor thereafter. To access these qualities, one needs to go beyond Hb to access other hematological parameters that will give information on some latent physiological processes in the prospective donor. For instance, the Hb estimation is less sensitive in the early stages of iron deficiency.8
There have been reports on some physiological alterations arising from repeated blood donation.9,10 Donation-induced iron deficiency (DIID) is one of the complications of frequent blood donation.11 The development of iron deficiency involves three sequential events: iron depletion, iron-deficient erythropoiesis and finally, iron deficiency anemia.12,13 The event continues until the anemia becomes clinically apparent. Globally, the minimum interval between whole blood donations varies between 56 days (8 weeks) and 16 weeks, with the World Health Organization recommending not more than once every 2 months.11,14 The onset of donation-induced iron deficiency may be determined using the full blood count (complete blood count). The red cell indices and red cell distribution width are useful tools.11 In view of these, this study sought to evaluate the hematological parameters of first-time and repeat blood donors.
MethodStudy designThe study took a descriptive cross-sectional approach. The purposive sampling technique was used. The period studied was from October 2018 to November 2018.
Study locationThe study was performed at the Donor Clinic of the University of Calabar Teaching Hospital, Cross River State, Nigeria. The University of Calabar Teaching Hospital is a 410-bed tertiary health institution located in Calabar Metropolis, which is the fusion of the Calabar South and Calabar Municipal Local Government areas of Cross River State. Cross River State has an area of 21,787 km2 and a population of 2,892,988, as of the 2006 census.15,16,17
Study subjectsA total of 178 screened prospective donors who consented and presented themselves at the Donor Clinic of the University of Calabar Teaching Hospital were purposively recruited for the study. Donors who withheld consent were not enrolled.
Sample collection and analysisApproximately 5ml of blood was collected into an EDTA-anticoagulated bottle via the antecubital fossa. The full blood count (complete blood count) was analyzed within one hour of collection using the SYSMEX XN550 hematology analyzer. The autoanalyzer uses the Coulter principle, which is a validated method. The sample was collected from the opposing side of the arm intended for the proper blood donation.
Inter-donation intervalThe inter-donation interval used in the study center is ≥ 3 months. Hence, prospective donors are deferred if they fall short of the interval. However, the information is often provided by the prospective donor (when last donated), as there is no centralized donor database to validate this.
DefinitionsClinical anemia was defined using the World Health Organization cut-off point of < 13 g/dL for men and 12 g/dL for women, while subclinical anemia was defined as hemoglobin values of 13 to 13.9 g/dL for men and 12 to 12.9g/dL for women.18
Ethical considerationThe study was approved by the Health Research Ethics Committee of the University of Calabar Teaching Hospital Calabar. Informed consent was obtained from the subjects prior to patient enrolment and sample collection.
Statistical analysisThe generated categorical data were represented as frequencies and percentages, while the continuous data were presented as means and standard deviations. The Student's t-test and one-way analysis of variance (ANOVA) were used to determine the statistical difference among mean groups, while the chi-square test was used to determine univariate association. The Ducan post hoc analysis was used to classify mean groups. The linear-by-linear chi-square test was used in assessing trends. The receiver operator characteristic (ROC) curve was used to assess the suitability of predictive markers for diagnosis. The alpha value was kept at 0.05.
ResultsA total of 178 male donors were recruited for the study. Of these, the age ranges 18 to 28 years, 29 to 39 years and 40 to 50 years constituted 47.2%, 46.6% and 6.2%, respectively. The mean and median age of the donors were 29.8 years and 30 years, respectively (range: 20–47). Commercial donors constituted the majority (80.3%) of the donors. Approximately 42.7%, 21.9%, 6.7%, 18.0%, 2.8% and 7.9% of the donors were students, civil servants, applicants, traders, security agents/workers and skilled workers, respectively. First-time donors, second-time donors, third-time donors, fourth-time donors, fifth-time donors, sixth-time donors and seventh-time donors constituted 11.2%, 5.6%, 8.4%, 15.2%, 27.0%, 23.6% and 9.0%, respectively, of the blood donors (Table 1).
Demographic characteristics of the blood donors studied.
| Characteristics | Frequency (%) |
|---|---|
| Age range (years) | |
| 18 - 28 | 84 (47.2) |
| 29 - 39 | 83 (46.6) |
| 40 - 50 | 11 (6.2) |
| Type of donor | |
| Voluntary | 35 (19.7) |
| Commercial | 143 (80.3) |
| Number of donations | |
| 1st time donors | 20 (11.2) |
| 2nd time donors | 10 (5.6) |
| 3rd time donors | 15 (8.4) |
| 4th time donors | 27 (15.2) |
| 5th time donors | 48 (27.0) |
| 6th time donors | 42 (23.6) |
| 7th time donors | 16 (9.0) |
| Occupation | |
| Students | 76 (42.7) |
| Civil servants | 39 (21.9) |
| Applicants | 12 (6.7) |
| Traders | 32 (18.0) |
| Security agents/workersa | 5 (2.8) |
| Skilled workers | 14 (7.9) |
Table 2 shows the analysis of some demographic characteristics with the donor type. While the majority of each of the age ranges were commercial donors, the age range 18 to 28 years represented the bulk (85.7%) of the voluntary donors and the age range 29 to 39 years represented the majority (55.2%) of the commercial donors. The difference in the distribution among the various age groups were found to be statistically significant (p < 0.05). Most of the first-time donors (100.0%) and second-time donors (90.0%) were voluntary donors and represented 57.1% and 25.7% of the voluntary donor population, respectively. The distribution of the number of donation times and donor types (voluntary or commercial) was found to statistically differ (p < 0.05). Most (59.2%) of the students were commercial donors. However, they also represented the bulk (88.6%) of the voluntary donor population. All the applicants, skilled workers, security agents and workers were commercial donors.
Analysis of the association of some of the demographic characteristics with the type of donor.
| Variable | Voluntary donors (%) | Commercial donors (%) | Statistics |
|---|---|---|---|
| Age range (years) | |||
| 18 - 28 | 30 (35.7) | 54 (64.3) | X2(2) = 26.056 |
| 29 - 39 | 4 (4.8) | 79 (95.2) | p < 0.01 |
| 40 - 50 | 1 (9.1) | 10 (90.9) | |
| Number of donations | |||
| 1st time donors | 20 (100.0) | 0 (0.0) | X2(6) = 149.513 |
| 2nd time donors | 9 (90.0) | 1 (10.0) | p < 0.01 |
| 3rd time donors | 6 (40.0) | 9 (60.0) | |
| 4th time donors | 0 (0.0) | 27 (100.0) | |
| 5th time donors | 0 (0.0) | 48 (100.0) | |
| 6th time donors | 0 (0.0) | 42 (100.0) | |
| 7th time donors | 0 (0.0) | 16 (100.0) | |
| Occupation | |||
| Students | 31 (40.8) | 45 (59.2) | X2(2) = 36.755 |
| Civil servants | 2 (5.1) | 37 (94.9) | p < 0.01 |
| Applicants | 0 (0.0) | 12 (100.0) | |
| Traders | 2 (6.3) | 30 (93.7) | |
| Security agents/workersa | 0 (0.0) | 5 (100.0) | |
| Skilled workers | 0 (0.0) | 14 (100.0) |
Table 3 shows the comparison of some hematological parameters among the donors, based on the number of donations. The total white blood cell count of the control subjects (first-time donors) was found to be comparable to the test group (repeat donors). Post hoc analysis showed statistical differences among the test groups; the second-, fourth-, fifth- and sixth-time donors had a significantly lower total white blood cell (TWBC) count than that of the third-time donor. The red cell count of the controls (first-time donors) was significantly higher (p < 0.05) than that of the repeat donors. Post hoc analysis showed that the red cell count of first-time donors was comparable to that of the second-time donors, but significantly higher than that of the third-, fourth-, fifth-, sixth- and seventh-time donors. The hemoglobin (Hb) and hematocrit of the first-time donors were comparable to those of the second- and third-time donors, while significantly higher than those of the repeat fourth-time donors. The mean corpuscular hemoglobin (MCH) and mean corpuscular hemoglobin concentration (MCHC) of the first-time donors were comparable to those of the second-, third- and fourth-time donors, but significantly higher than those of the repeat fifth-time donors. The mean cell volume (MCV) of the first-time donors was comparable to that of the repeat donors up to the sixth-time donors, while significantly higher than that of the seventh-time donor. Similarly. The red cell distribution width (RDW) of the first-time donors was comparable to that of the repeat donors up to the fifth-time donors, while significantly lower than that of that of the sixth- and seventh-time donors The mean platelet volume of the first-time donors was comparable to that of the second-, third-, fourth-, fifth- and sixth-time donors, but significantly different from that of the seventh-time donors. The platelet count of all the first-time donors is comparable to that of the repeat donors.
Comparison of hematological parameters among donors based on the number of donations.
TWBC: Total white blood cell; RBC: Red blood cell; Hb: Hemoglobin; HCT: Hematocrit; MCV: Mean corpuscular volume; MCH: Mean corpuscular hemoglobin; MCHC: Mean corpuscular hemoglobin concentration; RDW: Red cell distribution width; MPV: Mean platelet volume.
Means with same letter superscripts belong to the same mean group.
Table 4 shows the proportion of the study subjects that have clinical and subclinical anemia. None of the subjects had clinical anemia, as only those who passed the hemoglobin screening were selected. However, 55.6% of the subjects had subclinical anemia. Among these, 66.6%, 40.7%, 60.4%, 83.3% and 87.5% of the third-, fourth-, fifth-, sixth- and seventh-time donors had subclinical anemia. No subclinical anemia was observed in the first- and second-time donors.
Proportion of study participants with subclinical anemia.
Table 5 shows proportion of donors with anemia, using red cell indices based on the number of donations. Anemia was not observed in first- to third-time donors, using the MCHC and RDW. However, a small proportion was present in first- and second-time donors, using the MCV and MCH. The majority of the repeat donors from the fourth-time donors upwards showed anemia, using all four parameters. The proportion of anemia increases as the number of donations increases, as seen by linear-by-linear analysis, using red cell indices.
Proportion of donors with anemia using red cell indices based on the number of donations.
X2: Chi square; X2L: Linear-by-linear Chi-square).
Reference range: MCV: 80 – 100fL.
MCH: 27 – 32pg.
MCHC: 30 – 35g/dL.
RDW: 11 – 16SDfL.
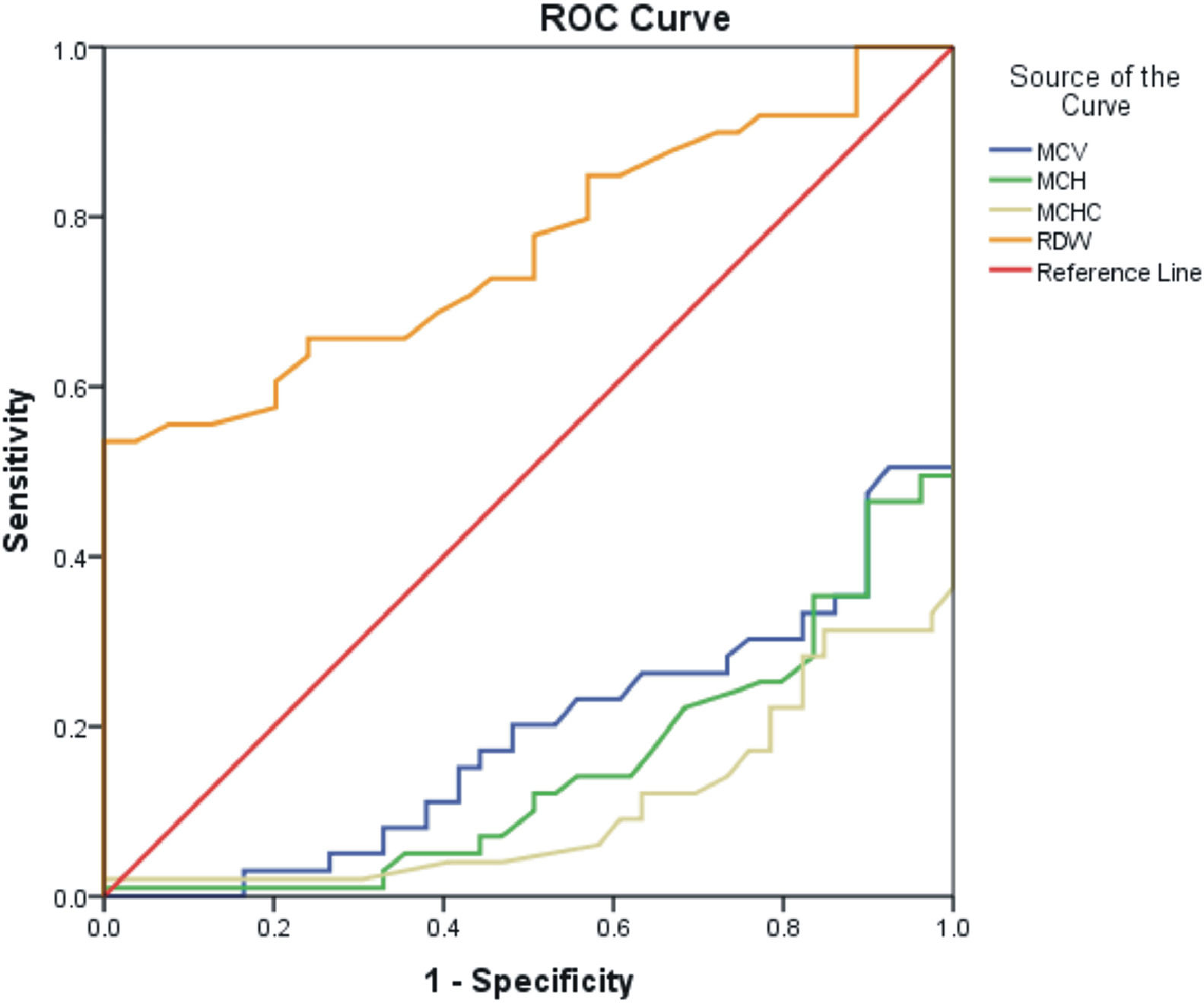
Figure 1 shows the comparison of the suitability of the red cell indices for predicting subclinical anemia among the studied population. The RDW performed better than the other red cell indices, with an area under the curve of 0.764 and a cutoff point of 14.70SDfL (at 65.70%% sensitivity and 75.90% specificity), showing good predicting power. The MCV, MCH and MCHC had cutoff points of 85.85fL, 29.95pg and 34.05g/dL, respectively, with poor predicting power (small area under the curve) (Table 6).
Comparison of the suitability of the red cell indices in predicting subclinical anemia.
The mean and median ages of the donors studied were 29.8 ± 6.4 years and 30 years, respectively. Additionally, the majority (94.9%) of the donors were between 18 and 39 years old. This finding is a reflection of the demographic structure of Nigeria, a developing country characterized by a relatively young population, in comparison to developed countries.5,19,20 Moreover, young people, being savvier with information technology and relatively better informed, are more likely to join the donor recruitment campaign.5 All the donors recruited within the study period were males. Male-dominated donor pools are prevalent in Nigeria and in other Sub-Saharan countries.21,22,23,24 This has been attributed to another cultural dogma that women should abstain from blood donation because of their monthly menstrual cycles.7 Donor type analysis in this study showed that commercial donors comprised the majority of the donors. This trend is consistent with previous reports in Nigeria.25,26,27 Voluntary blood donation has been lagging in Nigeria over the years owing to logistic constraints and other bureaucratic hitches associated with the national blood transfusion service. Consequently, this has created a scenario where commercial donors are the major donor types. Similarly, the challenges of voluntary blood donation cuts across the Sub-Saharan countries. For instance, in the western African Sub-Sahara, only Togo (98.3%), Senegal (79.4%), Benin (92.1%), and Cape Verde (77.3%) reported an elevated number of voluntary non-remunerated donors in a World Health Organization (WHO) survey.28,29 The WHO campaign on an effective and efficient blood transfusion service is anchored on voluntary non-remunerated donation. Remunerated blood donors have been classified as high-risk groups, as they have been documented to express higher seropositivity for transfusion-transmissible infections than voluntary donors.7,25,26 The bulk of the donors (65.7%) were at least on their fourth donation, a result of the donor pool being mainly commercial donors. Students represented the largest portion of the donor population. A similar trend has been reported in Ethiopia,30 Zimbabwe31 and China.32 The vast access to information by students could possibly aid in their support of blood donation campaigns.5
The largest proportion of voluntary donors were found among the age range of 18 to 28 years. Moreover, students constituted the majority of the voluntary blood donors. People of young age and those in school are most likely to gain access to information on blood drives. Most blood drives in Nigeria happen at schools. The bulk of the voluntary blood donors are first- and second-time blood donors. Commercial donors are more likely to donate often, sometimes under the recommended inter donation lag. These donors are motivated by the financial remuneration arising from the donation, without recourse to the health implications.
The total red cell count, hemoglobin and hematocrit of the first-time donors were significantly higher than those of the repeat third- and fourth-time donors, even though the two latter were within the reference range. This finding is consistent with previous reports.9,10 Frequent donation poses the risk of iron deficiency and would subsequently reflect on the hemoglobin and other red cell indices. Similarly, repeat fifth-time donors had a significantly lower MCH and MCHC and significantly higher RDW (in the sixth-time donors) than that of the first-time donors (control), while seventh-time donors had a significantly lower MCV than that of the first-time donors. Furthermore, a large proportion of the repeat donors had subclinical anemia, as well as morphological anemias, as evidenced by their MCV, MCH, MCHC and RDW, especially from fourth-time donors upwards. The MCV, MCH, MCHC and RDW have been documented as good proxy markers for iron deficiency, even in a latent stage.33,34,35 The linear-by-linear analysis showed that as the number of donations increases, the greater the chances of morphological anemia arising. Despite the fact that all the donors were judged non-anemic based on the Hb value, the findings of this study pose the concern and the need to look beyond the pre-donation Hb benchmark, especially in those who have donated more than three times to protect the donors from iron depletion. The primary role of blood bank is to protect the donor, while providing safe blood to the patient (recipient).
Comparison of the suitability of the red cell indices to predict subclinical anemia in the studied population showed the RDW as being a good proxy marker for detection of subclinical anemia. This is in synchronization with the literature previously reported.12
ConclusionThe principal finding of this study was that donors who have donated blood more than four times have significantly lower MCH and MCHC and significantly higher RDW, while those who have donated up to seven times have significantly lower MCV. The proportion of subclinical anemia recorded in the study points to the fact that these repeat donors are at great risk of iron deficiency. Considering the number of morphological anemias observed among donors above the donation Hb cutoff, we suggest complete blood count analysis for prospective donors. Moreover, in line with the postulation of Alvarez-Ossoria and colleagues,36 we suggest that serum ferritin estimation be performed for donors who have donated blood more than three times, with an iron supplementation follow-up in cases of iron deficiency at blood donation centers.
Study limitationWe used surrogate markers for the iron store analysis of this study. However, it is pertinent to state that serum ferritin is the confirmatory gold standard for iron store analysis.
Author's contributionsCOO: conceived the study, performed sample analysis, performed literature search, performed data curation and wrote and edited the manuscript draft. DCO: supervised the work, performed sample analysis and edited the manuscript draft. HUO: performed literature search, performed statistical analysis and wrote the initial manuscript draft. IMO: performed the literature search and edited the initial manuscript draft. All authors read and approved the final manuscript.