After the first publications in preclinical studies in the 1980s1 and the approval by the FDA in 1993,2 the combination of clopidogrel and aspirin became the standard treatment for patients with coronary stent angioplasty.3 The antiplatelet effect of clopidogrel, from the thienopyridine family, occurs by inhibiting the binding of ADP to its receptor, P2Y12 and consequently, ADP platelet activation.3 In addition to non-hematological adverse effects such as diarrhea, vomiting, liver and skin toxicity,4–6 the medical literature reports the presence of hematological adverse effects such as thrombotic thrombocytopenic purpura, hemolytic-uremic syndrome and bone marrow suppression with aplastic anemia, thrombocytopenia and neutropenia.3,7,8 Here we report the case of a patient who developed neutropenia after the onset of clopidogrel therapy because of a coronary event, her management and clinical evolution.
Case reportAn 84-year-old female patient was diagnosed with a previous, asymptomatic acute myocardial infarction during a routine visit to her cardiologist in early November 2019. She had a previous history of colon cancer in 2015, managed with surgery, chemotherapy and capecitabine (with remission of the tumor), as well as comorbidities such as arterial hypertension, type 2 diabetes mellitus and pulmonary emphysema due to smoking habit until the diagnosis of the coronary event. She had been taking losartan, metformin, ciprofibrate and inhaled umeclidinium + vilanterol. Aspirin 100 mg/day and clopidogrel 75 mg/day were started on the consultation with her cardiologist. A cineangiocoronariography was requested immediately, but she was submitted to the procedure only on 16/12/2019 when she received a coronary stent.
A complete blood count (CBC) on 11/11/2019, soon after the cardiological consultation and the start of the antiplatelets agents, showed hemoglobin (Hgb) of 12 g/dl, white blood cells (WBC) of 7000/mm3 and platelets (Plt) of 238,000/mm3. On the day after angioplasty (about 40 days after the beginning of clopidogrel), the patient presented Hgb of 8.9 g/dl and WBC of 970/mm3 (WBC differential count was not provided, nor the Plt count). At her first visit to our service on 20/12/2019, the patient complained of tiredness to great and medium efforts, she denied fever, symptoms suggestive of infection or bleeding. She had stopped smoking and was taking the medication above. The physical exam was inexpressive, with only mild cutaneomucosal pallor, no lymph node enlargement or visceromegaly. CBC on that day showed a Hgb of 10.5 g/dl, WBC of 1290/mm3 with 100 neutrophils/mm3 and Plt of 137,000/mm3. New laboratory exams were requested to assess the possible association with infectious conditions. CBC on 21/12/2019 showed similar results with Hgb of 10.2 g/dl, WBC of 1.020/mm3, 140 neutrophils/mm3 and Plt of 140,000/mm3. There were no immature cells in the peripheral blood. The liver function tests (LFT) were normal, serum creatinine was of 1.4 mg/dl (since before angioplasty), LDH of 283 U/L, folic acid of 9.2 ng/ml and vitamin B12 of 265 pg/ml. Dosages of immunoglobulins and light chains were normal and serology for hepatitis B and C, HIV, HTLV I/II were negative, and for toxoplasmosis, EBV, CMV, Herpes Simplex, all showed positivity for IgG and IgM non-reagent.
In view of the absence of other diagnostic hypotheses that could explain the sudden decrease of WBC (neutrophils) and also in the Hgb, we hypothesized the association with the beginning of clopidogrel.
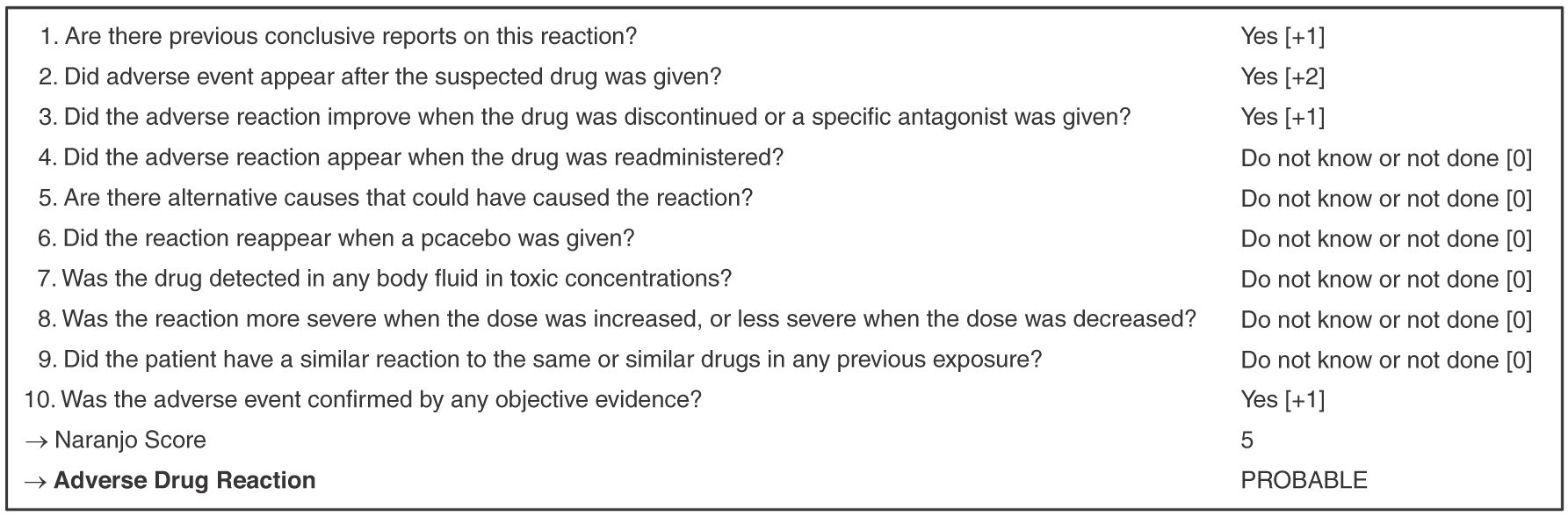
Applying the Naranjo et al. (1981) algorithm to the case of our patient, we verified the probable relationship between clopidogrel and neutropenia, as shown in Figure 1. The score 0 attributed to question number 5 results from the absence of any other diagnosis or evidence that could be compatible with the hypotheses raised in the first consultation, before or after the event.9
Based on these assumptions it has been suggested to her cardiologist to change the antiplatelet agent to ticagrelor which was accomplished on 22/12/2019. On 26/12/2019, four days after the medication switch the patient presented WBC of 2420/mm3 with 800 neutrophils/mm3 and 250.000 platelets/mm3; on 02/01/2020 (after 12 days), both had increased to WBC of 4440/mm3 and neutrophils of 2620/mm3, and the Plt were of 237.000/mm3. She remained with mild anemia of 10 g/dl of Hgb and kept serum creatinine of 1.4 mg/dl. Erythropoietin replacement was started because the patient still complained of tiredness to great and medium efforts. On 03/02/2020, the patient showed an increase in Hgb to 11.3 g/dl, WBC to 6280/mm3, neutrophils to 4.180/mm3 with 192.000 platelets/mm3. She reported a slight improvement of tiredness to efforts.
DiscussionThe haematological toxicity of thienopyridines was confirmed in vitro and described by Maseneni et al. (2013). In this study, the authors demonstrated clearly the deleterious action of the metabolites of clopidogrel, ticlopidine and prasugrel after the action of myeloperoxidase present in neutrophils, leading to mitochondrial injury, loss of mitochondrial cytochrome c which activates caspase 9, leading to apoptosis. This whole process could be blocked by rutin, which inhibits the action of myeloperoxidase.10
With an incidence rate of less than 0.1%, several case reports have associated clopidogrel with the onset of neutropenia. A simple search on PubMed using the terms “clopidogrel + neutropenia” reveals 17 cases since 2000.8 Wu et al. (2016) summarizes 12 of those cases found so far including the two cases reported in that publication. The median age of patients was 65 years, with 58% of female gender. The indication to start clopidogrel was coronary artery disease in more than 80% of patients and the dose of 75 mg/day was the most used. The median time to the onset of neutropenia was 22 days, and 5 days for recovery after drug withdrawal. The median neutrophil count for these patients was 131 cells/mm3. Our patient, 20 years older than the reported median age, had her first blood count available about 40 days after the start of clopidogrel, shortly after undergoing angioplasty, when there was already leukopenia of <1000 cells/mm3. It is not possible, therefore, to state the exact moment of the onset of neutropenia in this case. Recovery of neutrophil counts occurred within the reported median time reported, reaching more than 500 cells/mm3 after just four days of clopidogrel withdrawal. Neutrophil count was normal after 12 days. At no time did the patient receive G-CSF that could have interfered with the normalization of neutropenia.
Nevertheless, the possibilities of bone marrow hipoplasia or infiltration were raised in the first consultation. However, due to the relatively good general condition of the patient, the absence of fever or bleeding and the absence of immature cells in the peripheral blood, we chose not to do bone marrow aspiration and biopsy immediately. In fact, just four days after switching from clopidogrel to ticagrelor, the blood count had already shown an increase in neutrophils and platelets. This rapid improvement contributed to discard the above hypotheses.
Still, one of the most frequent problems in clinical practice is determining the causal relationship between a drug and an adverse reaction. Naranjo et al. contributed significantly to the understanding of this issue by developing an algorithm that estimates the probability of this cause and effect relationship that when applied in the case of our patient, contributed to the establishment of this relationship.9
The high cardiovascular risk of these patients, however, requires a new antiplatelet drug to be started, from a different family from thienopyridines. Our option (in agreement with her cardiologist) was for ticagrelor, first of a new class of antiplatelet drugs, cyclopentyltriazolpyrimidines, an ATP analogue that does not require activation of hepatic cytochrome P450, resulting in a faster onset of action and greater inhibition of ADP-induced aggregation.3 We believe that the anemia of the patient could also be explained by the chronic non-dialysis renal failure that she already presented before the present event.
In conclusion, the present case shows that although neutropenia is a rare adverse event in patients using clopidogrel, the drug should be remembered as a possibility associated with the event after a detailed drug history. In addition, in patients at high cardiovascular risk, ticagrelor seems to be a safe alternative.