Diversity in Classical Hematology Research
More infoAlthough not mandatory, medical residency has become a sine qua non condition for practicing in most medical specialties in Brazil. Residency programs are hosted mainly by university accredited academic centers and hospitals in the national public healthcare system, under guidance and accreditation by a national commission. Despite the importance of these programs for the development of the hematology workforce, few studies have addressed their characteristics and impact on society.
MethodsWe performed a comprehensive cross-sectional survey of a 35-year alumni cohort from a hematology academic residency program in Brazil.
ResultsIn total, 86/98 (87.8%) responded to the survey. The mean age at residency completion was 28.5 years, 60.5% of the alumni were women and sixty-four (74.4%) self-declared their skin color as white. Higher rates of parental education attainment and low rates of trainee financial dependence were observed and these patterns were stable over time. While the proportion of trainees from other states increased steadily, the number of hematologists practicing in other states remained stable. Approximately half of the alumni worked both in the private and public sectors, mainly in malignant hematology and in outpatient clinics. Twenty-five percent of the alumni reported prior leadership and teaching positions, mainly as directors of transfusion services.
ConclusionOur results provide data that can be potentially useful for policymakers and curricular development in the planning of strategies concerning the future workforce of hematologists.
In Brazil, the obtention of a medical degree after a six-year medical course allows doctors to start independent medical practice. However, although not formally required, engagement in clinical and surgical specialties is normally preceded by an additional 2 to 5 years of residency. In fact, due to the increasing compartmentalization of medical knowledge, along with the need for additional competencies related to patient care, communication and professionalism, participation in a residency program virtually became a sine qua non condition for practice in most medical specialties.1 Currently, most of these programs are offered by public institutions as part of a national public healthcare program (Sistema Unico de Saude, or “SUS”).
Accordingly, residency programs evolved as a critical part of medical training in Brazil, not only in medical specialties, but also in more general areas, such as internal medicine, pediatrics and family medicine. The programs are regulated by federal legislation and certified on a regular basis by a national commission linked to the Ministry of Education.2
In Brazil, hematology residency programs (whose scope overlap with fellowship programs in some areas) encompass benign and malignant hematology and transfusion medicine. There are currently 52 active hematology residency programs (HRPs) in Brazil, offering 180 positions every year (Brazilian Association of Hematology, Hemotherapy and Cellular Therapy (ABHH), personal communication, July 5, 2021). Unlike some international services, Brazilian hematology residency programs cover training in transfusion medicine and, in contrast to the US, only hematology residency includes training in malignant hematology, while oncology residency only encompasses non-hematologic malignant solid tumors. Although residency programs are regulated by federal legislation and have evolved into critical parts of medical training in Brazil, very little data is available on the trainee demographics and diversity, as well as on the impact of these programs on career paths.
Moreover, according to the Brazilian Medical Association (AMB), the 478,010 physicians registered in Brazil (2.27 per 1,000 inhabitants) are unevenly distributed throughout the country, with Sao Paulo state, which alone represents 22% of the Brazilian population, comprising 26% of this workforce, as well as the highest concentration of hematologists.1
In the present study, we described demographic, socioeconomic and educational characteristics of former hematology trainees and explore their association with career paths in hematology in a 35-year cohort of alumni from an academic HRP in Brazil.
MethodsStudy design and study populationWe performed a cross-sectional survey of an alumni cohort of an academic residency program in hematology. This is a public residency program held by the University of Campinas, in Campinas, Sao Paulo, Brazil, active since 1985. The alumni were identified by a list provided by the residency program office. The number of residents admitted per year varied from 2 to 6. Until 2002, medical school graduates were eligible for the program immediately after graduation and the program included a first year of internal medicine rotations. From 2003 onwards, a two-year residency in internal medicine became mandatory prior to enrollment in an HRP. The admission process to the program did not vary substantially during the study period and included aptitude tests and a semi-structured interview. The aptitude evaluation consisted of multiple-choice tests, focused on core areas or internal medicine, and a clinical competence evaluation, in the form of “long case” discussion until 2002, and of an objective-structured clinical examination test with simulated patients after 2003. The semi-structured interview focused mainly on the candidate's CV. The study was performed in accordance with the Declaration of Helsinki and was approved by our local Institutional Review Board (IRB). Participants provided written informed consent prior to answering the survey.
Data collectionThe survey was elaborated by the investigators, encompassing the following domains: (i) demographic data, including social and economic information, (ii) academic background prior to admission and (iii) career choices and paths after residency. After a pilot survey with six hematologists from the University of Campinas, the final survey was used in the study. We used the REDCap3 to present the survey to study participants and to collect data. Question formats were multiple-choice, yes/no and stratified questions (some encompassing more than one possibility). Spaces for open comments were available in all questions. The survey was sent to participants on August 19, 2020, along with an invitation signed by the investigators and an informed consent term. Non-respondents were contacted two more times by email or text messages. After a period of 3 months, the database was closed for analysis.
Statistical analysisData was extracted from the REDCap into an Excel file and analyzed using the IBM SPSS version 20.0. Data were presented as means ± standard deviation or medians and range, as specified. We performed the analysis using descriptive statistics.
ResultsThe list provided by the residency program office of the University of Campinas included 102 former residents, of whom 98 had valid emails for contact, who were invited to participate. Of these, 86 responded to the survey, yielding a response rate of 87.8%.
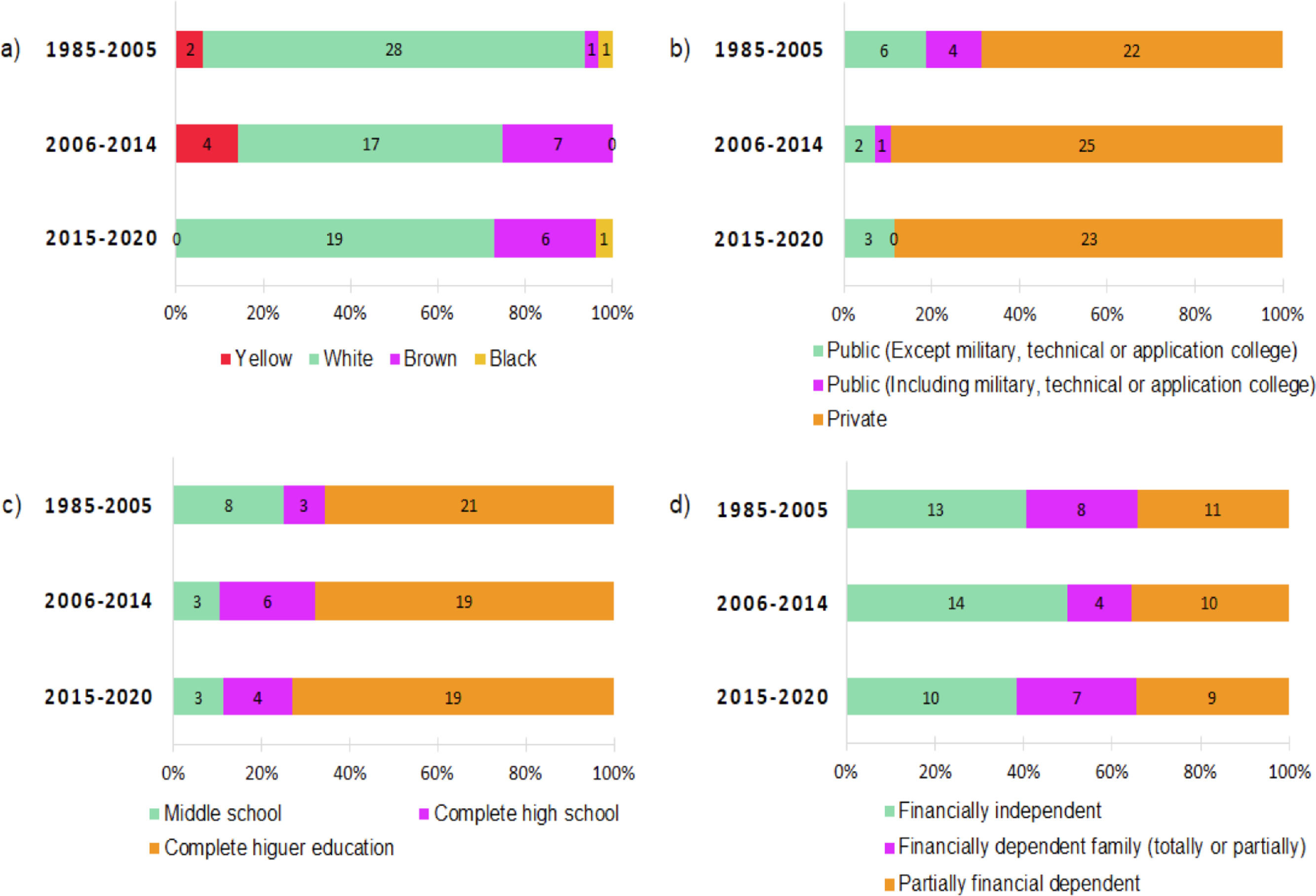
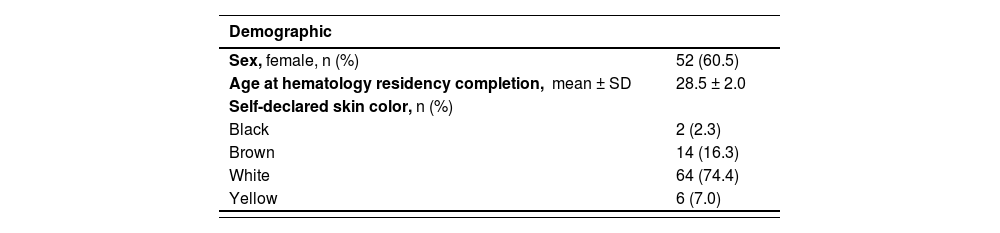
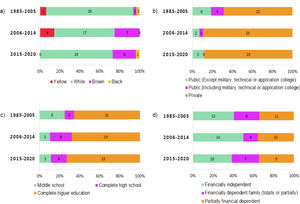
Characteristics of the study population and their career pathsDemographics, ethnic diversity and socioeconomic characteristicsThese indicators are shown in Table 1. Of the 86 alumni who responded to the survey, 60.5% were women. The mean age at hematology residency completion was 28.5 years. Sixty-four (74.4%) self-declared their skin color as white. A slight increase in the number of alumni who self-declared their skin color as non-white was observed in the first tertile of the follow-up (1985 - 2005), but this trend was not maintained thereafter (Figure 1). In regard to socioeconomic status, 37 (43%) did not require any financial support from their families, while 30 (35%) presented some degree of financial dependence. We did not observe any significant change in this aspect during the study period. Regarding parental (father's) education, 59 (68.6%) had completed higher education, a figure that remained stable during the study. Only three residents (3.5%) required support from government social programs during their training. Trends in some of the main indicators are presented in Figure 1.
Characteristics of the study population
| Demographic | |
|---|---|
| Sex, female, n (%) | 52 (60.5) |
| Age at hematology residency completion, mean ± SD | 28.5 ± 2.0 |
| Self-declared skin color, n (%) | |
| Black | 2 (2.3) |
| Brown | 14 (16.3) |
| White | 64 (74.4) |
| Yellow | 6 (7.0) |
| Paternal education, n (%) | |
|---|---|
| Middle schoola | 14 (16.3) |
| High schoolb | 13 (15.1) |
| Higher education | 59 (68.6) |
| Use of government social programs during residency yes, n (%) | 3 (3.5) |
| Academic background | |
| High school (institution type), n (%) | |
| Publicc | 8 (9.3) |
| Publicd | 8 (9.3) |
| Private | 70 (81.4) |
| Medical degree (institution type), n (%) | |
| Public | 75 (87.2) |
| Private | 11 (12.8) |
| Internal medicine residency (institution type)e, n (%) | |
| Public | 55 (64) |
| Private | 4 (4.7) |
| Previous involvement in research activities, yes, n (%) | |
| During internal medicine residency | 45 (52.3) |
| During hematology residency | 57 (66.2) |
| Knowledge of English at the time of residency admission | 69 (80.2) |
Temporal trends of selected demographic, socioeconomic and educational characteristics of the study population. For the purpose of these analyses, the study was divided into three periods with similar number of alumni per period. (a) Skin color; (b) Type of school of high school graduation; (c) Parental educational attainment (father's); (d) Financial status at the time of residency admission.
Most participants (70; 81.4%) had completed high school at a private institution. In contrast, only 11 (12.8%) residents obtained their medical degree from private institutions. Similarly, of the 59 alumni who completed an independent residency program in internal medicine before hematology, the vast majority (55) did so at a public institution. In regard to research experience, 57 (66.2%) reported participation in research activities during the hematology residency. Since a large portion of the hematology technical literature is in English, we also explored this skill, with 80% of alumni reporting English fluency at the time of the hematology residency admission.
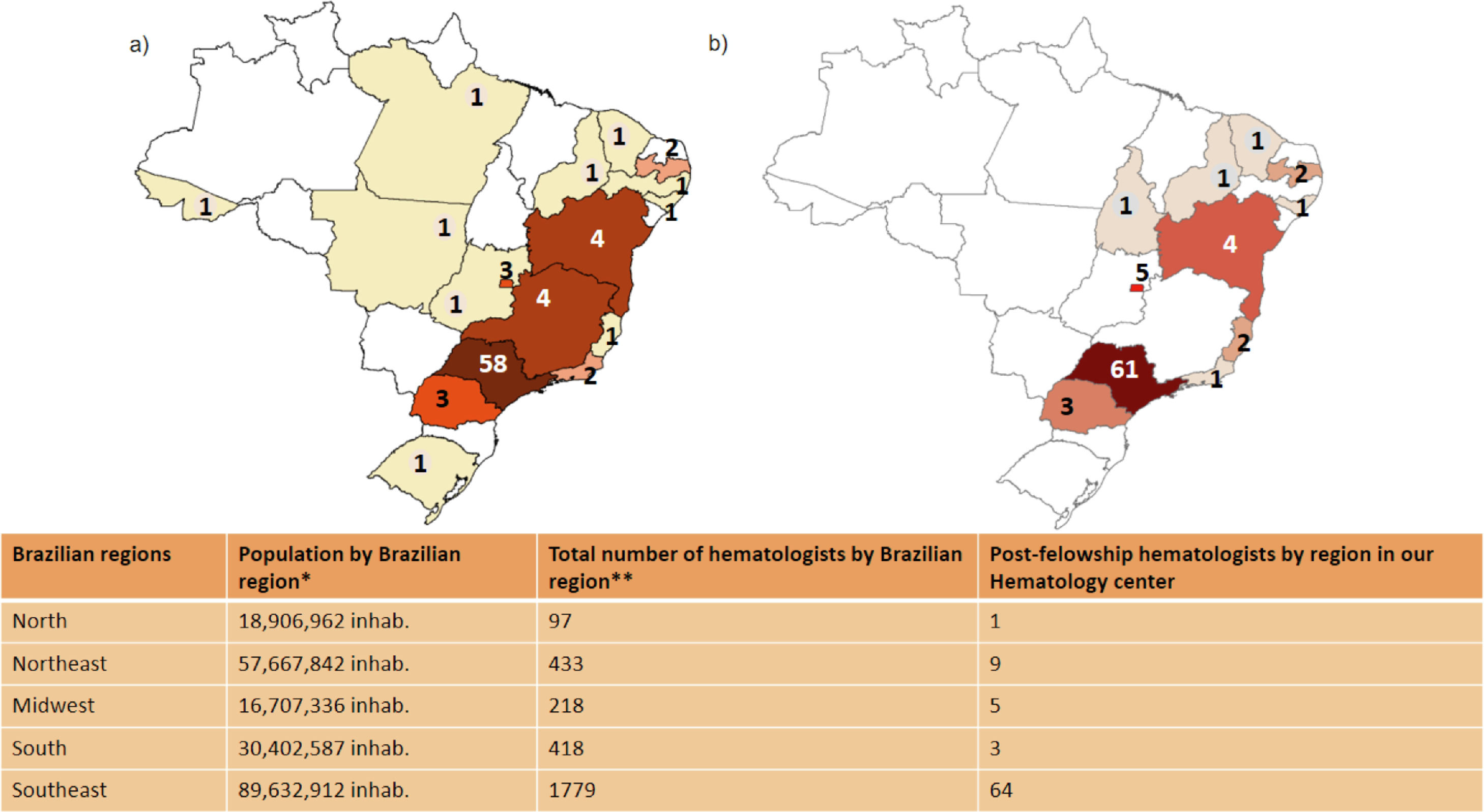
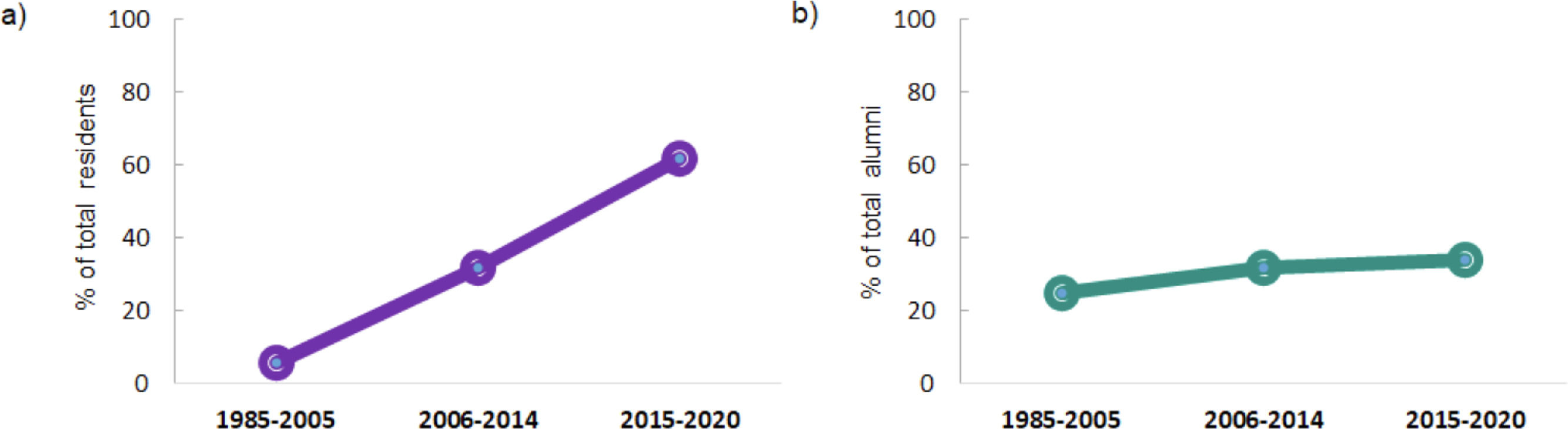
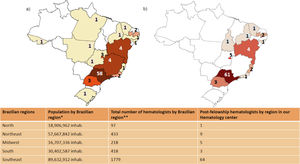
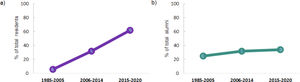
Geographic distributionFifty-eight (67.4%) participants obtained their medical degree from schools in the same state of their residency program (Sao Paulo). Twenty-four (29.26%) of the alumni work in a different state from where they graduated. Detailed data are shown in Figure 2. We also explored post-residency geographic distribution, which demonstrated an even more homogenous pattern, with Sao Paulo state as the current practice site for 61 (70.9%) of the alumni. Of note, 4.6% of the alumni are currently working outside Brazil. To assess whether this distribution pattern changed over time, we plotted the percentage of residents who obtained their medical degree in states other than Sao Paulo, as well as the percentage of residents currently practicing there across three different time periods, with a similar number of respondents. As shown in Figure 3, while the proportion of residents from other states rose from less than 5% to more than 60%, the proportion of residents practicing elsewhere remained stable, approximately 20 to 30% (Figure 3).
(a) Geographic distribution of sites of obtention of medical degree and of (b) current professional activity. The table shows general and demographic data from the five different geographic regions of Brazil. * Brazilian National Institute of Geography and Statistics (IBGE), year 20214; ** The Medical Demography Study in Brazil, 20201.
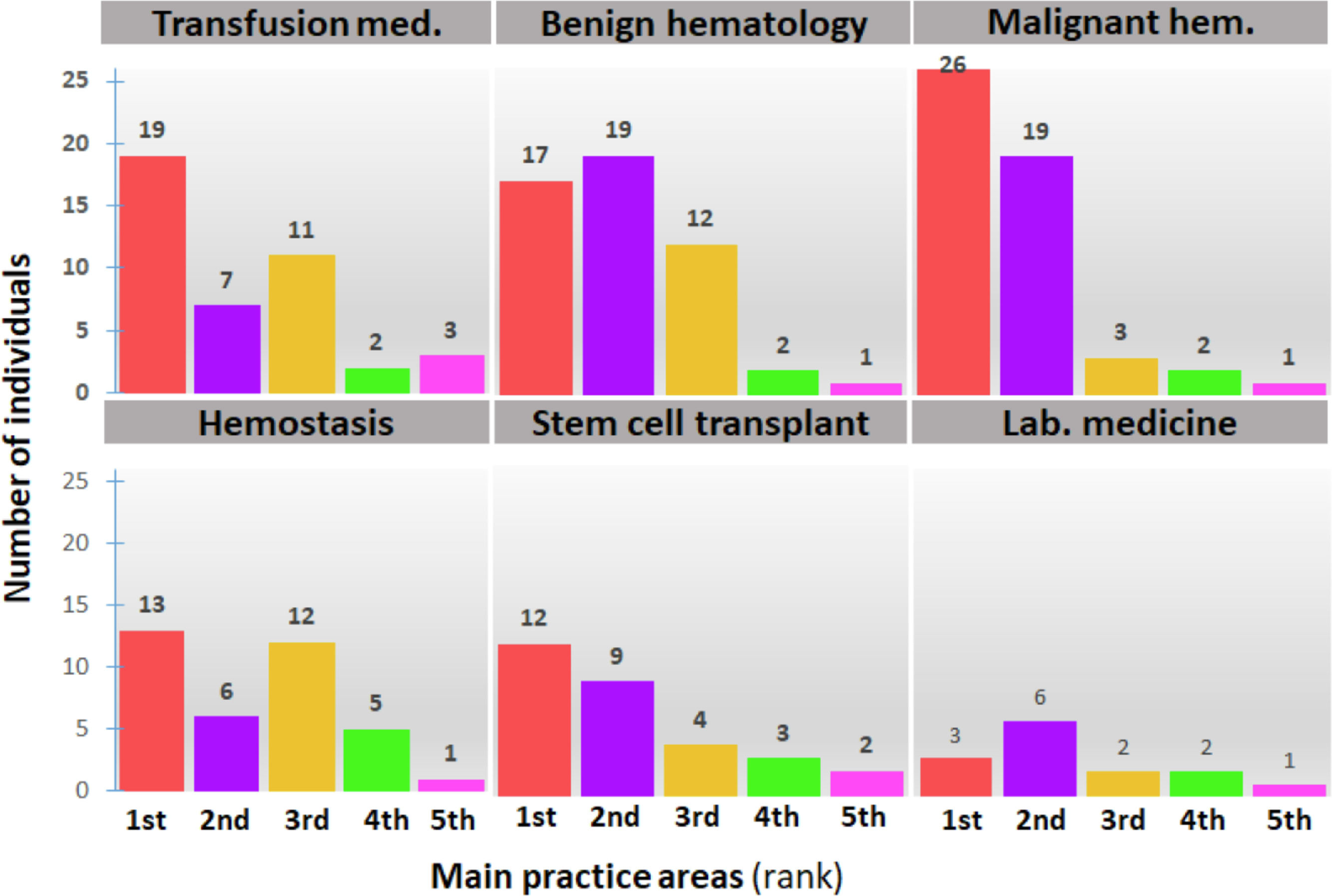
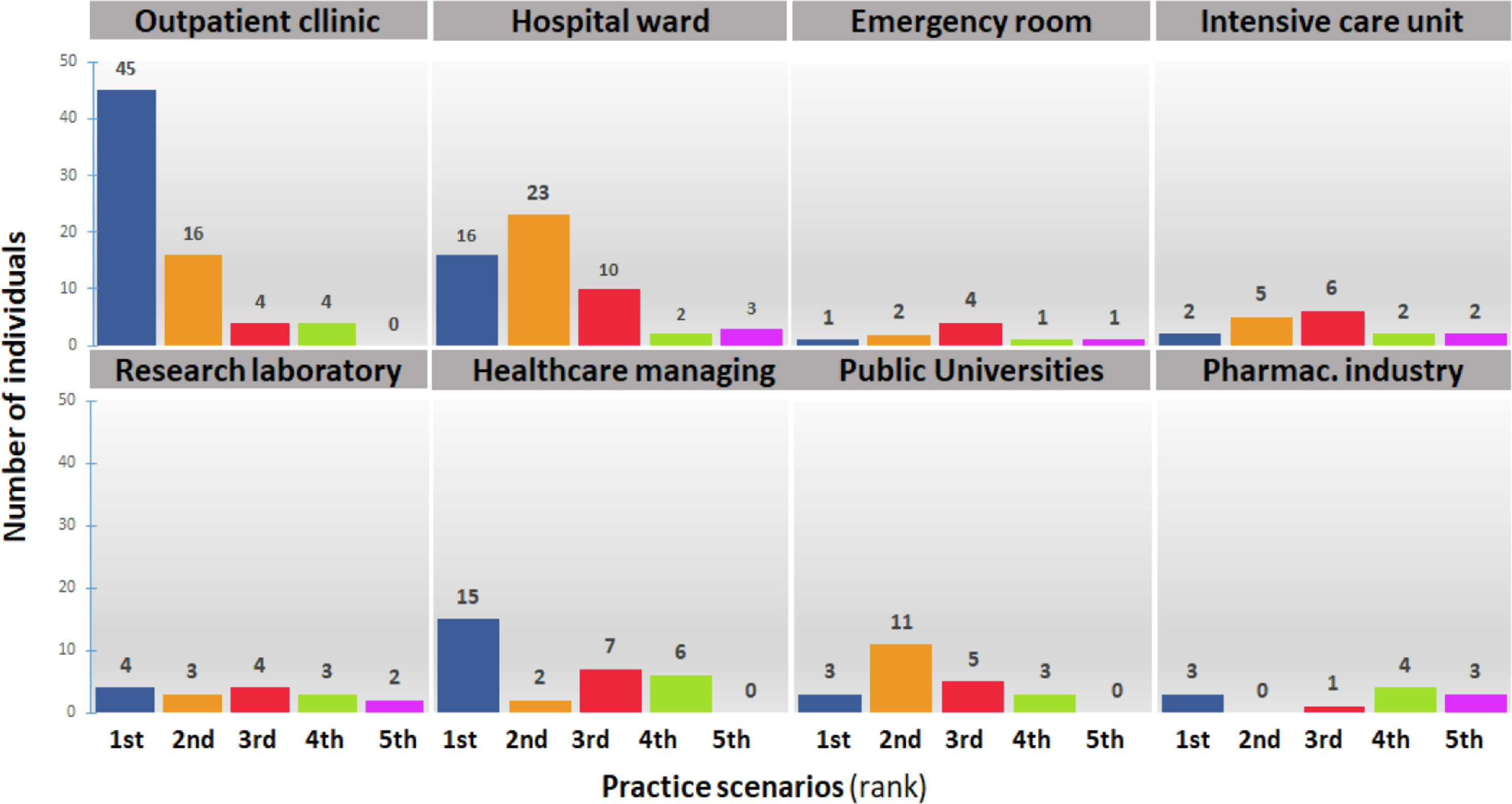
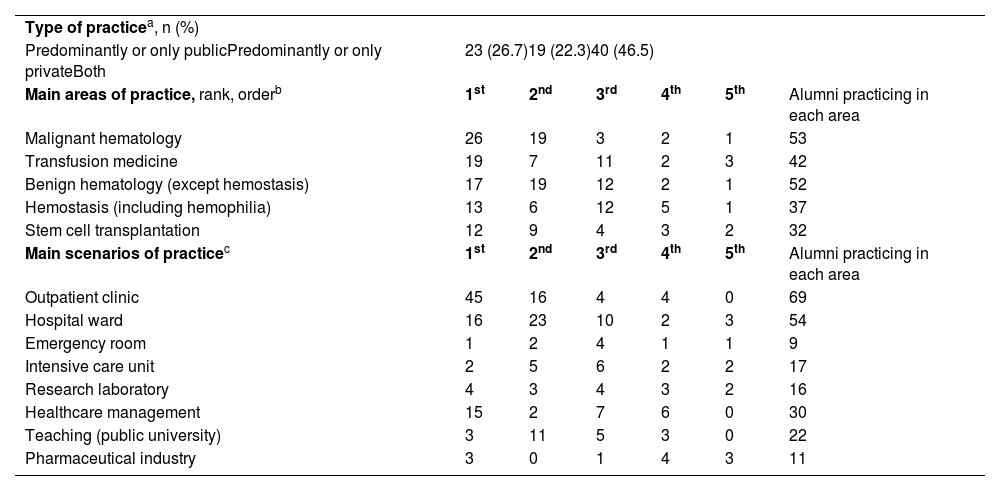
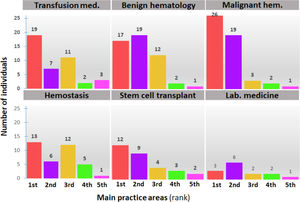
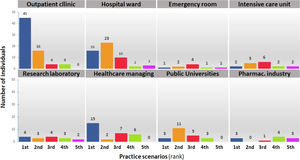
We next explored the characteristics of current medical practice in order to obtain a broader view of the different career paths from the study population. As shown in Table 2, approximately half of the alumni work both in the private and public sectors, with the remaining participants equally distributed between these sectors. Regarding the main areas of practice, malignant hematology, benign hematology, transfusion medicine and hemostasis were ranked first. A graphical view of these data is shown in Figure 4. Likewise, the alumni were asked to select the scenarios of practice of their current practice (Table 2). Outpatient clinics were listed as the main scenario by 52%, followed by hospital wards and healthcare management by 18% and 17% of participants, respectively. These results are depicted in Figure 5.
Characteristics of current medical practice
| Type of practicea, n (%) | ||||||
| Predominantly or only publicPredominantly or only privateBoth | 23 (26.7)19 (22.3)40 (46.5) | |||||
| Main areas of practice, rank, orderb | 1st | 2nd | 3rd | 4th | 5th | Alumni practicing in each area |
| Malignant hematology | 26 | 19 | 3 | 2 | 1 | 53 |
| Transfusion medicine | 19 | 7 | 11 | 2 | 3 | 42 |
| Benign hematology (except hemostasis) | 17 | 19 | 12 | 2 | 1 | 52 |
| Hemostasis (including hemophilia) | 13 | 6 | 12 | 5 | 1 | 37 |
| Stem cell transplantation | 12 | 9 | 4 | 3 | 2 | 32 |
| Main scenarios of practicec | 1st | 2nd | 3rd | 4th | 5th | Alumni practicing in each area |
| Outpatient clinic | 45 | 16 | 4 | 4 | 0 | 69 |
| Hospital ward | 16 | 23 | 10 | 2 | 3 | 54 |
| Emergency room | 1 | 2 | 4 | 1 | 1 | 9 |
| Intensive care unit | 2 | 5 | 6 | 2 | 2 | 17 |
| Research laboratory | 4 | 3 | 4 | 3 | 2 | 16 |
| Healthcare management | 15 | 2 | 7 | 6 | 0 | 30 |
| Teaching (public university) | 3 | 11 | 5 | 3 | 0 | 22 |
| Pharmaceutical industry | 3 | 0 | 1 | 4 | 3 | 11 |
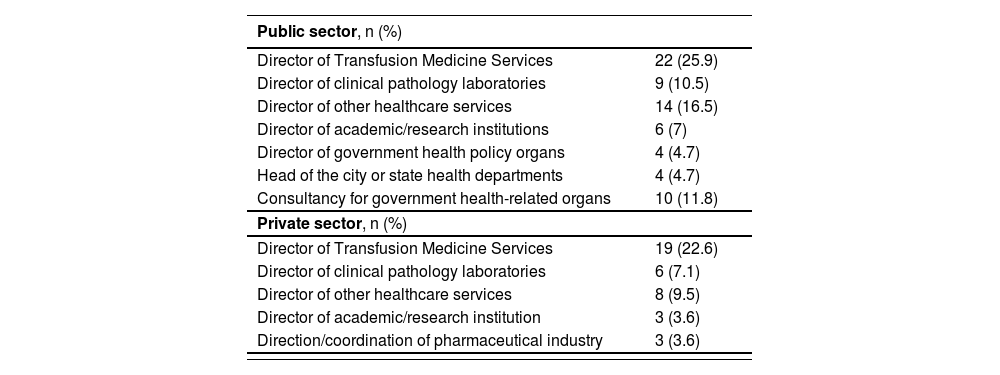
In order to obtain a clearer view of the participant career paths, as well as information about the social impact of the residency program, we inquired about positions involving leadership (defined as formally delegated positions) after residency. Results are shown in Table 3, demonstrating that more than 25% of the alumni reported these types of positions, with Director of Transfusion Medicine services ranking first in both the public and private sectors.
Leadership positions in hematology and hemotherapy
The term director encompasses formally delegated management positions; 2 alumni did not answer these questions.
Completion of a residency program is a key step in the training of hematologists in Brazil, offering approximately 180 positions every year. By providing a comprehensive set of data on career paths of a cohort of medical doctors who completed a hematology residency in an academic center spanning 35 years, our survey can contribute to the assessment and planning of residency programs, as well as to a more detailed perception of their social impact.
Most participants were female, following the national trend of Brazilian Hematology programs in which 62.8% of the students are women1. Compared to the international scenario, a higher percentage of men in onco-hematology residency programs has been reported in the USA,5 as well as in Canada.6 Our data is also consistent with the feminization process observed in Brazilian medicine, mainly from 2009, culminating in 2019 in a population of 55% of female residents out of a total of 53,776.1
Regarding the age of completion, the average was 28.5 ± 2 years, illustrating the time required for these professionals to initiate their hematology practice. National data indicate that 44.2% of the economically active Brazilian population enter the labor market before 14 years old in informal jobs, highlighting that training in hematology involves a significant delay that needs to be accommodated by trainees and their families. In contrast, recent job shortages are also operating in the opposite direction and a trend has been reported of increasing age until the first formal job in Brazil, which in 2017 reached 28.6 years old. If this trend persists, the gap between training time in medicine and other areas can become less significant.7,8
The vast majority (74.4%) of the participants declared their skin color as white, which is even higher than the percentage (67.1%) of medical students who took the Brazilian National Exam on Student Performance (ENADE) in their last year of medical school in 2019.9 According to the most recent statistics, the proportion on Brazilians who report their skin color as non-white is 42.7%.10 These figures reinforce the inequality in the access to medical school in Brazil and suggest that this gap could be even higher in residency programs, as demonstrated in other areas.11,12 Interestingly, we observed a slight increase in the number of participants who declared themselves non-white, comparing the period of 1985 - 2005 to the period of 2006 - 2014, but this trend was not maintained in recent years.
Policies to promote diversity in access to higher education have been implemented in Brazil since 2000, becoming mandatory in federal institutions in 2012, but recent admission data suggest that they had little impact on admissions to medical schools.13,14 While isolated efforts to increase the reach of these policies have been successful,15 only the long-term follow-up will be sufficient to assess their impact on the long desired increase16,17 in the ethnic diversity of the medical workforce in Brazil in general and in hematology, specifically.
One of the main objectives of our survey was to gather information about the socioeconomic status of hematology residency graduates. First, we observed that only 22% of participants needed to provide resources for their family during the residency program. This differs from data obtained in the USA where, despite a similar average age entry into the onco-hematology residency (30 years), most residents are providers for their families.18 We also noted that only 3.5% of the participants reported the use of government social programs. In addition, our population was characterized by a high proportion (68.6%) of participants whose fathers had a higher education degree, even surpassing the figure for medical students in Brazil in 2019 of 57.7%.9 While this association can be partially explained by the effect of parental education on the choice of a career in medicine,19,20 it is well-known that parental educational attainment is one of the most sensitive and broad indicators of socioeconomic status.21,22 Of note, no temporal change was observed in these two indicators during the 35-year time span encompassed in our survey. Together, these data clearly indicate that access to residency programs is characterized by underrepresentation of less privileged classes, not only mirroring, but possibly deepening the pattern of inequality that characterizes the access to higher education in Brazil. Other characteristics, such as the high proportion of private high school graduates and fluency in English as a second language, further support this impression.
We also explored the geographic distribution of the participants, as the distribution of the medical workforce in a country with continental dimensions like Brazil is a challenge.23 More than 70% of the alumni remained in the state of São Paulo, demonstrating a clear concentration of the hematology workforce, even for participants who obtained their medical degrees in another state. Moreover, this concentration pattern did not change over time, presenting an apparent increase in more recent years. According to a recent report on the demographics of the medical practice in Brazil, 60.4% of the hematologists work in the southeastern region (where São Paulo state is located), with only 14.7% in the Northeast and 3.3% in the northern region of Brazil.1 We tried to explore the potential impact on the geographic distribution of hematologists of changes in the Brazilian infrastructure of transfusional medicine services that occurred in the late 1980’s and early 1990´s and that consisted in the creation of institutions dedicated to blood transfusion in each Brazilian state (“Hemocentros”). However, less than 10% (n = 6) of our sample finished the residency before these changes were fully implemented, so that it is difficult to explore the likely effect of these changes (which resulted in a demand for hematologists in other states) on our results. Altogether, our data highlight that promoting a more even distribution of hematologists in the country is a challenge that needs to be addressed.
Another topic explored in our survey was the direct participation in scientific activities during the residency training, which was reported by more than half of the participants. In a survey conducted by Horn et al. to determine factors associated with career choices by hematology residents trained at academic institutions in the US, it was shown that the trainees who published or presented scientific papers were more likely to pursue academic careers,24 which may be associated with the relatively high proportion of the alumni in academic positions in our sample. However, participation in scientific activities should not be viewed solely as a step towards academic careers, but rather as a key element of medical training in an era in which the evolution of medicine requires continuing education at increasing paces. Accordingly, the appraisal of scientific data, critical reading of scientific literature and several other skills formerly associated with academic jobs are now considered core competencies of the medical education.25-27
Nearly half of respondents reported spending 50% of their time on activities in both public and private sectors, with the remaining participants evenly divided between the public and private sectors. This is in accordance with a recent demographic survey with more than 2,400 physicians in Brazil, in which dual professional practice was also reported by around 50% of the participants.1 The fact that only one quarter of the hematologists works exclusively in the public sector, which provides care for nearly 70% of the Brazilian population, highlights the lack of incentives and attractive careers in this area.28
In regard to areas of practice, malignant hematology, transfusion medicine and benign hematology were the most cited areas, probably reflecting the job market for hematologists in Brazil, coupled with a specific characteristic of the HRP of the University of Campinas, which has historically emphasized the formation in hemotherapy and benign hematology, along with malignant hematology. While it is of no surprise that these activities were mainly performed in outpatient clinics and hospital wards, we observed with interest that healthcare management and teaching at public universities emerged as the next top-cited scenarios of practice. Of note, the preference for malignant hematology over other areas of hematology is not specific to Brazil, being also reported in a recent survey of 86 graduates from a Hematology-Oncology program in the USA, but with a much wider gap, with only 10% of the time of the participants devoted to clinical practice in non-malignant hematology. Of note, the time spent on education and administration by American hematologists was also much lower (5.2% in each activity) than in Brazil, highlighting important differences in the post-residency job market between these countries.29 Similarly, private practice and administration activities were much less frequently reported by Canadian hematologists.6
We finally explored the participation of the alumni in leadership positions in both private and public sectors. While we are not able to provide a benchmark for comparison, leadership positions were reported by more than 25% of the participants, with directorship of transfusion medicine services as the most cited position. While only 53.6% of the participants reported being affiliated with national medical associations, we observed a relatively high engagement (32.6%) of former residents in international scientific associations.
The main limitation of our study is the fact that it was obtained from a population of residents from a single academic center, which also results in a limited sample size, so that results are not automatically generalizable to the entire population of hematologists in Brazil. However, it should be noted that to date, hematology residency programs are still concentrated in the Southeast of Brazil, with academic centers, such as the University of Campinas, representing the type of institutions providing more residency training positions. Therefore, while additional studies are warranted to confirm whether the pattern observed in our study is reproduced in other areas of Brazil, we believe that our demographic and socioeconomic data, as well as the characteristics of the job market reported in this survey, are fair representations of the current status of hematology practice in Brazil. Nonetheless, similar surveys encompassing a nationwide sample could certainly generate valuable data to improve hematology residency training in Brazil, which is a topic that has recently gained the attention of the ABHH.30
ConclusionsOur results provide a comprehensive overview encompassing a 35-year time span of demographic and socioeconomic data and career paths of graduates of an HRP from an academic center that can contribute to the planning and assessment of hematology training in Brazil.
We thank Drs. Irene Lorand-Metze and Marina P. Colella for providing feedback on the survey instrument.