Anti- M is a naturally occurring antibody of the MNS blood group system. This antibody is the most reactive at temperatures below 37°C, with an optimum temperature of 4°C and is considered to be clinically insignificant. However, there are few studies that have reported anti-M as a mixture of IgG and IgM antibodies. In these cases, anti-M capability to react at 37°C and in anti-human globulin (AHG) phase make it clinically significant.1–7 Here, we report for the first time in Iran, three cases with discrepancy in ABO blood grouping due to anti-M.
Case 1An 11-year-old female child with a diagnosis of hepatic disease was admitted in the hospital. The ABO forward grouping of the patient was group B while the reverse grouping was group O, by tube technique. The blood grouping was repeated, and we found the same reaction. A direct antiglobulin test (DAT) was performed using polyspecific antiglobulin reagents (anti IgG and C3d) and was found to be negative. The auto control was also negative. Antibody screening was then performed with a commercially available three-cell panel (Immucor) and the antibody was found to be positive with one example of M-positive RBC and negative with two examples of M-negative RBCs. Antibody identification performed using as 11-cell panel from Immucor was suggestive of anti-M. In order to determine the immunoglobulin class of the antibody, treatment of the sera with dithiothreitol (DTT) was done. The antibody persisted after the serum was treated with DTT suggesting the presence of an IgG component along with IgM. Red cell phenotype of the patient showed the absence of the M antigen. Since there was no history of the transfusion, and the antibody reacted at 37°C and in the AHG phase, we concluded that the anti-M antibody detected was a naturally occurring antibody with an IgG component.
Case 2A 54-year-old male was admitted to the hospital for coronary bypass operation, and his blood sample was sent to the blood bank laboratory for routine blood grouping and antibody screening prior to the surgery. Blood grouping was performed by the conventional tube method which showed discrepant results. On forward grouping, the patient's red cells showed reaction with anti-B, but on reverse blood grouping, the serum showed reactivity with both A1 cells and B cells. The case was referred to immunohematology reference laboratories (IRLs) for further work-up. DAT and auto control were negative. An indirect antiglobulin test (IAT) was performed using a three-cell panel and it showed a pattern of reaction compatible with anti-M. Using an 11-cell panel, the antibody was identified as anti-M. The antibody was active at room temperature (RT), 37°C and AHG phase. DTT treatment was performed and indicated the presence of both IgG and IgM. History of patient confirmed that he had not received any kind of transfusion. On phenotype, using commercially available anti-M antisera (DiaClon), it was confirmed that the patient was negative for M antigen. To confirm the presence of anti-M, the 3-cell rule was used. Three cells positive with M antigen showing a +4 reaction and three cells negative with M antigen showing a negative reaction. Reverse blood grouping was repeated using M antigen-negative reagent red cells and this time, there was reaction to only A cells, confirming that the patient's blood group was B Rh-positive.
Case 3A 25-year-old pregnant woman with history of abortion was admitted in the hospital because of preterm rupture of membrane. Her blood sample was sent to the blood bank for routine blood grouping and cross-matching. The blood sample showed unexpected agglutination reaction, with forward grouping A while reverse grouping ‘O’. To rule out technical errors, we repeated the test with a new sample, but the reactions were the same. The history of her blood transfusion was checked and found that she never received any blood transfusion in past. The DAT and auto control were negative by the conventional test tube. The IAT using a three-cell panel showed a pattern of reaction compatible with anti-M. On testing the thermal amplitude, the antibody was found to be 4+ reactive at temperatures below 37°C, but also showed 4+ reactivity at 37°C and AHG phase. Using an 11-cell panel, the antibody was confirmed as anti-M. On phenotype the red cells, the patient was found to be negative for M antigen. This patient's blood group was confirmed to be A Rh-positive using M antigen-negative. To determine the immunoglobulin class of the antibody, the serum was treated with DTT, and an IAT was subsequently performed. The reactivity persisted after DTT treatment, but the reaction strength decreased, suggesting the presence of IgG along with IgM. As one component of the antibody was IgG, the patient was transfused with M antigen-negative A group RBC unit.
DiscussionIn the present study, ABO discrepancy that affected serum testing due to presence of additional antibody other than A or B were found in all cases. Antibody screening and antibody identification were performed and anti- M was identified. As there was not history of transfusion, most probably anti-M was naturally occurring. Further tests were performed to find that anti-M is IgM alone or a mixture of IgG and IgM. Activity at 37°C and DTT treatment indicated the presence of both IgG and IgM. Therefore, in all three cases, we gave M antigen-negative RBC to the patients.
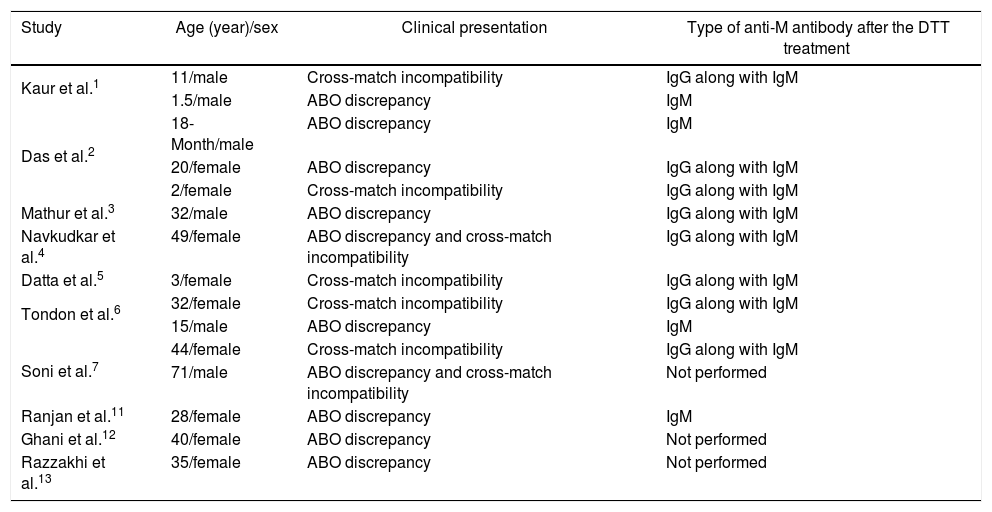
Because of rarity of anti-M, only case reports have been published in the literature (Table 1). Moreover, there are case reports of delayed HTR8 and HDN9 due to anti-M antibody. In a study by Nolan et al.,10 a case has described with anti-M antibody (IgM+ IgG nature) that was responsible for neonatal red cell aplasia with considerable reduction in proliferation of erythroid cells in culture. The authors have proposed that anti-M may cause HDN by destroying erythroid progenitors, like anti-K. Therefore, all these case reports indicate that anti-M antibodies can have varied presentations.
Case reports with anti-M in the literature.
| Study | Age (year)/sex | Clinical presentation | Type of anti-M antibody after the DTT treatment |
|---|---|---|---|
| Kaur et al.1 | 11/male | Cross-match incompatibility | IgG along with IgM |
| 1.5/male | ABO discrepancy | IgM | |
| Das et al.2 | 18-Month/male | ABO discrepancy | IgM |
| 20/female | ABO discrepancy | IgG along with IgM | |
| 2/female | Cross-match incompatibility | IgG along with IgM | |
| Mathur et al.3 | 32/male | ABO discrepancy | IgG along with IgM |
| Navkudkar et al.4 | 49/female | ABO discrepancy and cross-match incompatibility | IgG along with IgM |
| Datta et al.5 | 3/female | Cross-match incompatibility | IgG along with IgM |
| Tondon et al.6 | 32/female | Cross-match incompatibility | IgG along with IgM |
| 15/male | ABO discrepancy | IgM | |
| Soni et al.7 | 44/female | Cross-match incompatibility | IgG along with IgM |
| 71/male | ABO discrepancy and cross-match incompatibility | Not performed | |
| Ranjan et al.11 | 28/female | ABO discrepancy | IgM |
| Ghani et al.12 | 40/female | ABO discrepancy | Not performed |
| Razzakhi et al.13 | 35/female | ABO discrepancy | Not performed |
Anti-M is a naturally occurring antibody that may be IgM or IgG. It can not only cause discrepancy in blood grouping but may also be of clinical significance if it is reactive at 37°C. In all such cases an immunohematology card must be issued by mentioning the type and nature of the antibody and the patient advised about future blood transfusions. Patients with such antibody require blood transfusion with M antigen negative compatible RBCs.
Conflicts of interestThe author declares no conflicts of interest.