Laboratory findings in severe coronavirus disease (COVID)-19 may include lymphopenia, elevated D-dimer, lactate dehydrogenase (LDH), C-reactive protein (CRP), and ferritin.1 Several quantitative and functional abnormalities in lymphocyte populations have been reported in patients with SARS-CoV-2 infection, with evidence of depletion of cytotoxic T-lymphocytes and natural killer cells.2 Lymphopenia has been identified as a prognostic marker for poor outcomes as it could be in correlation with cytokine storm.1 Though numerically depleted, circulating reactive lymphocytes were detectable in a consistent proportion of patients, some of them with a lymphoplasmacytic phenotype.3,4 Whether this cell population is related to polyclonal or monoclonal hypergammaglobulinemia is still unknown.
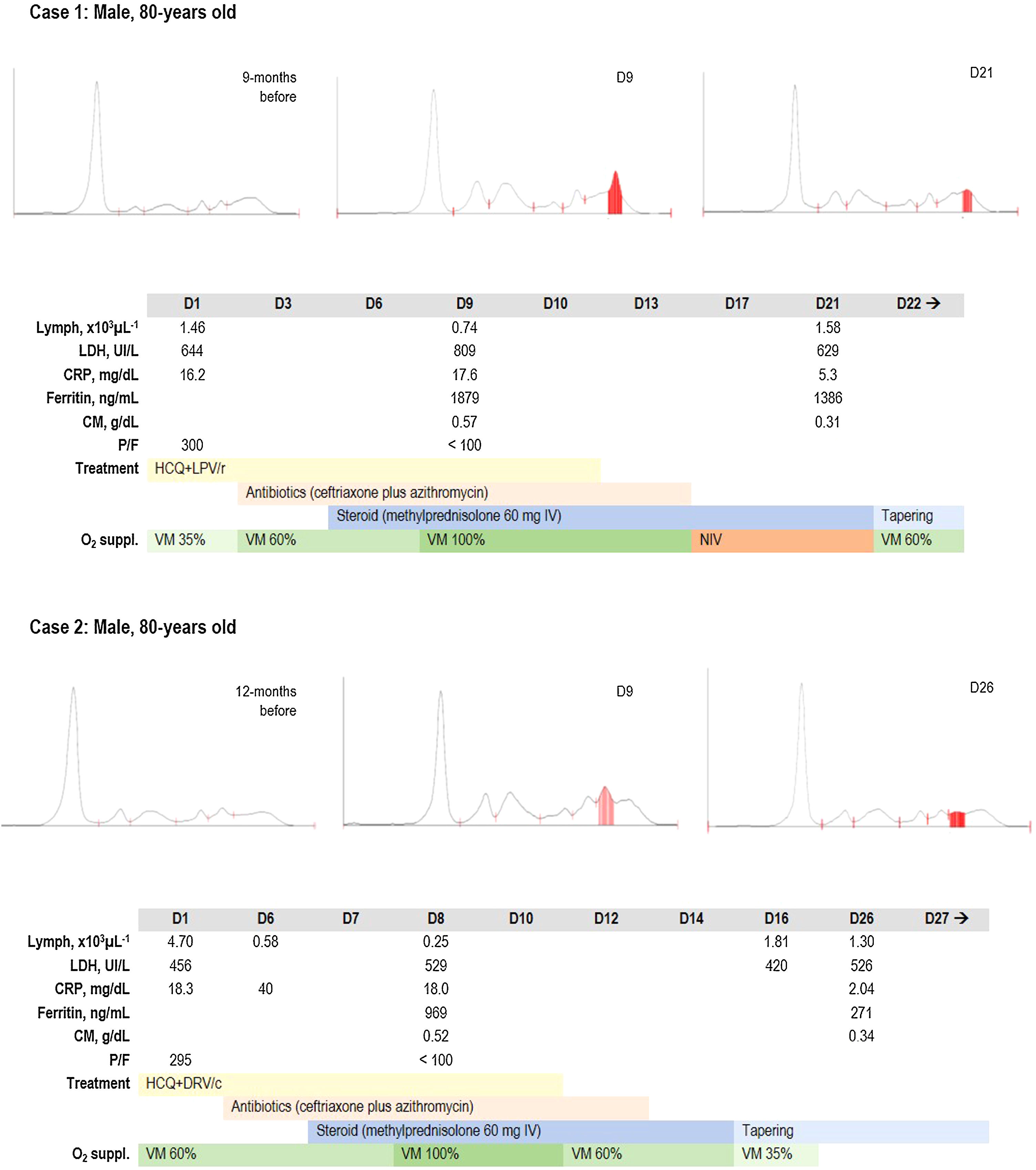
During SARS-CoV-2 outbreak in our region, we observed the case of an 80-year old man with severe COVID-19 and evidence of a transient monoclonal gamma-globulin spike (Figure 1, case 1). He had no previous evidence of monoclonal gammopathy and his serum protein electrophoresis (SPEP) was normal 9-month before. He was admitted to our COVID ward because of fever, malaise and increasing dyspnea. His nasopharyngeal swab was positive for SARS-CoV-2 RNA. Chest high-resolution computed tomography (HRCT) revealed bilateral ground-glass opacities and interlobular septal thickening. Treatment with hydroxychloroquine, lopinavir/ritonavir and antibiotics was given, with no significant improvement. At D9 blood tests revealed lymphopenia (740μL−1), increased LDH (809UI/L), ferritin (1879ng/mL), and CRP (17.6mg/dL). Prothrombin time was slightly prolonged (14.1s), whereas platelet count (489×109L–1) and fibrinogen (>900mg/dL) were increased. A monoclonal band was found on SPEP and it was characterized as IgG-lambda by immunofixation. Steroid treatment was added, and non-invasive ventilation was necessary from D17 to D21, when initial improvement in his respiratory status was observed. A repeated SPEP showed a significant decrease in M-protein, in parallel with reduction of inflammatory biomarkers and lymphocyte reconstitution. He then developed sepsis sustained by P. aeruginosa, successfully treated with piperacillin/tazobactam. His condition gradually improved and supplemental oxygen was stopped at D52. He was still in hospital for respiratory rehabilitation at time of manuscript preparation.
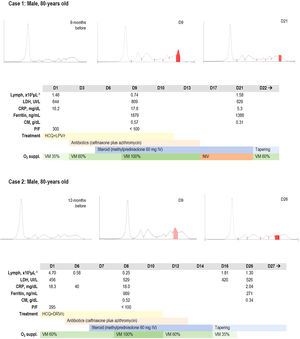
Even though SPEP was not systematically incorporated for COVID-19 evaluation at our Department, we observed similar findings in another 80-years old patient with COVID-19 related pneumonia who had a severe course of disease (Figure 1, case 2). He was admitted to our COVID Unit because of fever and non-productive cough. Bilateral patchy consolidations were seen on HRCT. His medical history included arterial hypertension, hypothyroidism and previous carotid thromboendarterectomy. No monoclonal spikes were observed in a past SPEP. Treatment with hydroxychloroquine, darunavir/cobicistat and antibiotics was given but his respiratory status continued to deteriorate. High-flow oxygen was administered through a non-rebreather face mask and steroid treatment was started. At D8, there was severe lymphopenia (250μL−1), increased LDH (529 UI/L), ferritin (959ng/mL), fibrinogen (797mg/dL), and CRP (17.9mg/dL). Platelet count and prothrombin time were within the normal range, whereas D-dimer was markedly increased (14,794ng/mL) without clinical or echographic evidence of venous thromboembolism. An IgG-kappa monoclonal band was found in his SPEP. The subsequent clinical course was favorable, allowing a gradual reduction in oxygen therapy and steroid tapering. The monoclonal component was significantly decreased in a repeated SPEP at D26, together with normalization of lymphocyte count, ferritin and CRP. Supplemental oxygen was discontinued at D17 and the patient was discharged after 13 days.
Monoclonal gammopathy results from clonal proliferation of plasma cells or antibody secreting B-cells, producing large amounts of homogenous immunoglobulin or light chain fragments. An “acute” or transitory monoclonal spike has been reported in association with a spectrum of acute and chronic inflammatory illnesses, including viral infections. In severe COVID-19 there is a massive release of IL-6, which is associated with adverse clinical outcomes.5 IL-6 has been recognized as a crucial growth factor for B-cell differentiation and terminal maturation into plasma cells,6 thus providing a mechanistic between severe COVID-19 and gamma-globulin peak production. Lymphocyte depletion could also result in a loss of regulatory T cell-mediated suppression of aberrant B-cell clones, with consequent dysregulated antibody production, which often regress after immune-restoration, as observed in our patients. It should be noted that both cases were recorded in elderly subjects, in which underlying aging-related subclinical plasma cells disorders are more frequent and could represent a prerequisite for dysregulated antibody production during SARS-CoV-2 infection.
In conclusion, based on these data it could be hypothesized that the presence of a monoclonal spike during the inflammatory phase could reflect the degree of immune hyperactivation in patients with severe COVID-19. Further studies are needed to evaluate its frequency, long-term evolution and prognostic role in this clinical setting.
ContributorshipAll authors managed the patient. NV was responsible for writing, NV and SO for the figure and FD for the literature search.
Conflicts of interestThe authors declare no conflicts of interest.