The West African region has been lagging in terms of the availability of, and accessibility to, safe blood. According to the 2016 World Health Organization (WHO) Global Status Report on Blood Safety and Availability, none of the West African countries met the WHO benchmark of 10 blood units per 1000 inhabitants. This study is aimed at discussing the blood transfusion status of West African countries in the pre-COVID-19 period and analyze the capacity to respond to the COVID-19 blood crisis, as well as to outline the panacea.
MethodsSecondary data were extracted from published reports, journal articles and web pages, reviewed and analyzed.
ResultAll the West African countries have recorded confirmed COVID-19 cases and deaths. The confirmed cases have reached 55,697, with 1069 deaths and a fatality rate of 1.9%, as of June 17, 2020. The assessed countries lagged in most of the WHO benchmarks for effective blood transfusion services.
ConclusionBlood transfusion services in the West African region lacked the basic benchmark practice and policy, are not coordinated and may find it hard to tackle the blood transfusion crisis created by the COVID-19 pandemic.
Blood transfusion is a lifesaving intervention that is included in the World Health Organization (WHO) list of essential medications.1–3 In Africa, and sub-Saharan Africa in particular, blood transfusion is critical in the management of varying pathologies, including malaria associated anemia, trauma, obstetric hemorrhage and neoplasms, among others.4–6 However, the availability of, and access to, safe blood has continued to be a challenge in Africa.7 The 2016 WHO report on blood safety and availability showed that the WHO African region contributed to only 5.6% of the 112.5 million blood donations globally. Moreover, it revealed that 67 countries (38 of which are in the WHO Africa region) reported collection of less than 10 whole blood donations per 1000 inhabitants per year in 2013 which is below the WHO benchmark. Only Mauritius and South Africa beat the par, with 39.7% and 18.0% donations per 1000 inhabitants, respectively.8
The west African sub-region is made up of 16 countries, with an estimated population of 401,359,000, accounting for approximately 5.16% of the global population (United Nations estimate).9 The proportion of the population donating blood ranged from 0.24% to 0.72%.7 An efficient, well established and functional national blood transfusion system is scantly available in the region, irrespective of the development of national blood transfusion policies by most of the countries.8
An outbreak of pneumonia was reported on December 31, 2019 in the city of Wuhan, Hubei Province, China, which was identified and subsequently named severe acute respiratory syndrome corona virus 2 (SARS-CoV-2), belonging to the Beta coronavirus genus of the coronaviridae family on January 7, 2020.10–12 As of March 11, 2020, the World Health Organization declared the disease pandemic and named it COVID-19.13 It is a highly contagious respiratory disease. The principal symptoms of the disease include fever (98.6%), fatigue (69.6%), dry cough (59.4%) and dyspnea (43.0%).11,14 The incubation period of the virus varies from 1 to 14 days, with a mean value of 5 days.15 It is a respiratory tract infection primarily transmitted via respiratory droplets and contact. The maximum load of virus is present in the bronchoalveolar lavage fluid (93%).16 However, parenteral transmission has not been established, as only a few studies, such as one in Wuhan, China, which reported 6 out of 41 (14.6%) of the COVID-19 patient blood samples testing positive for COVID-19.17 Another study in China among blood donors has identified SARS-CoV-2 RNA in routine blood donations. In the study, 2430 blood donations (1656 platelet and 774 whole blood) collected between January 25, 2020 and March 4, 2020 were screened by real-time reverse transcription polymerase chain reaction (PCR) for SARS-CoV-2; in addition, almost 5000 samples collected between December 21, 2019 and January 22, 2020 were retrospectively tested. Four samples were positive for SARS-CoV-2. All four blood donors were asymptomatic at the time of collection, but two developed fever the day after donation.18 Similarly, there have been reports of the detection of SARS-CoV-2 in semen,19 the gastrointestinal tract, saliva and urine.20
As of June 17, 2020, there have been 8,043,487 confirmed cases and 439,487 deaths globally in 213 countries and territories and 2 conveyances.21 The COVID-19 pandemic started in western Africa in February 2020 in Nigeria,10 with Nigeria and Ghana being the most affected countries.
This study is aimed at discussing the blood transfusion status in the West African region in the pre-COVID-19 period and analyzing the capacity to respond to the blood demand during the pandemic of COVID-19, as well as discussing a possible panacea to improve services.
MethodsResearch articles, case reports, report updates and other web pages were reviewed for blood transfusion services and practices. The WHO database was searched for the blood transfusion practice in the West African region and COVID-19 updates, while the Worldometere database was searched for country populations. The Pubmed database and Google advanced search were used to search for COVID-19/SARS-CoV-2/nCOV-related articles. The data extracted were presented as frequencies and proportions (%) to weigh the capacity to respond to the blood demands in the pre- and intra-COVID-19 periods.
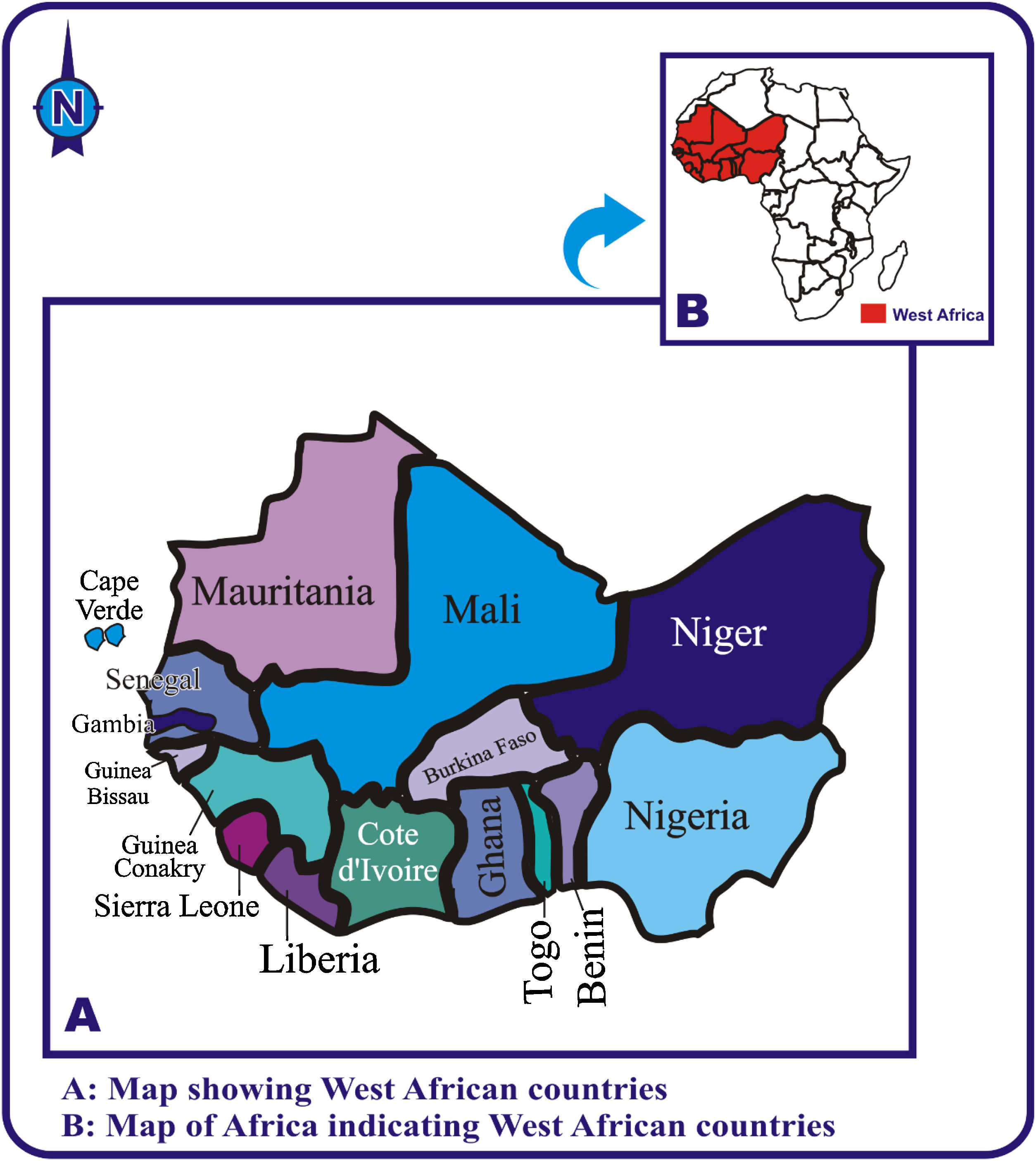
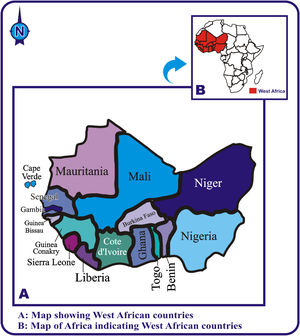
ResultsCOVID-19 pandemic in West AfricaWest Africa is composed of 16 countries: Benin, Burkina Faso, Cape Verde (Cabo Verde), Cote d’Ivoire, Gambia, Ghana, Guinea Conakry, Guinea Bissau, Liberia, Mali, Mauritania, Niger, Nigeria, Senegal, Sierra Leone and Togo (Figure 1). The region boasts 30% and 28% of Africa’s population and gross domestic product (GDP), respectively.22 All of these countries belong to the Economic Community of West Africa (ECOWAS), except Mauritania. The ECOWAS has a GDP of US$ 716.7 billion.23
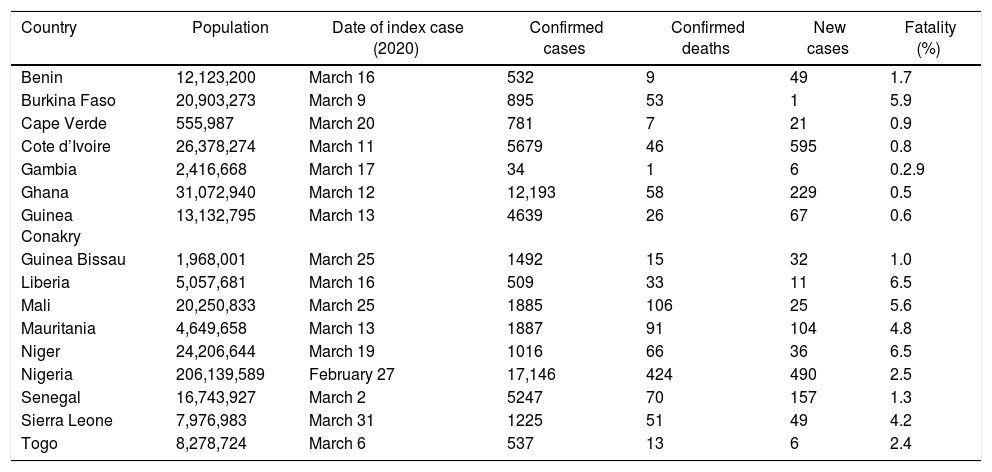
The first case of COVID-19 in West Africa was reported in Nigeria on February 27, 2020. Subsequently, the pandemic has escalated to other West African countries. As of the month of March 2020, Nigeria, Cote d’Ivoire and Senegal had the highest number of confirmed COVID-19 cases. On the other hand, Nigeria, Mauritania and Senegal recorded the highest number of confirmed COVID-19 deaths. Niger, Liberia and Burkina Faso had the highest fatality rates. The highest numbers of new cases were recorded in Cote d’Ivorie, Nigeria and Ghana (Table 1).
Incidence of COVID-19 in countries in West Africa, as of June 17, 2020.9,19
| Country | Population | Date of index case (2020) | Confirmed cases | Confirmed deaths | New cases | Fatality (%) |
|---|---|---|---|---|---|---|
| Benin | 12,123,200 | March 16 | 532 | 9 | 49 | 1.7 |
| Burkina Faso | 20,903,273 | March 9 | 895 | 53 | 1 | 5.9 |
| Cape Verde | 555,987 | March 20 | 781 | 7 | 21 | 0.9 |
| Cote d’Ivoire | 26,378,274 | March 11 | 5679 | 46 | 595 | 0.8 |
| Gambia | 2,416,668 | March 17 | 34 | 1 | 6 | 0.2.9 |
| Ghana | 31,072,940 | March 12 | 12,193 | 58 | 229 | 0.5 |
| Guinea Conakry | 13,132,795 | March 13 | 4639 | 26 | 67 | 0.6 |
| Guinea Bissau | 1,968,001 | March 25 | 1492 | 15 | 32 | 1.0 |
| Liberia | 5,057,681 | March 16 | 509 | 33 | 11 | 6.5 |
| Mali | 20,250,833 | March 25 | 1885 | 106 | 25 | 5.6 |
| Mauritania | 4,649,658 | March 13 | 1887 | 91 | 104 | 4.8 |
| Niger | 24,206,644 | March 19 | 1016 | 66 | 36 | 6.5 |
| Nigeria | 206,139,589 | February 27 | 17,146 | 424 | 490 | 2.5 |
| Senegal | 16,743,927 | March 2 | 5247 | 70 | 157 | 1.3 |
| Sierra Leone | 7,976,983 | March 31 | 1225 | 51 | 49 | 4.2 |
| Togo | 8,278,724 | March 6 | 537 | 13 | 6 | 2.4 |
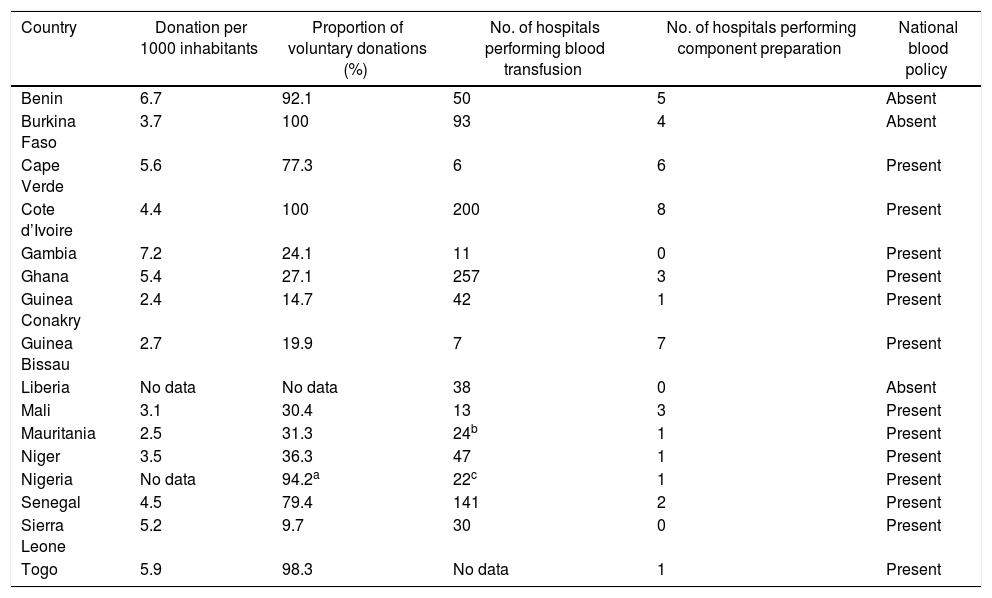
None among the 16 West African countries reached the WHO benchmark of 10 whole blood collections per 1000 inhabitants. The highest values, namely 7.2, 6.6 and 5.9, were reported in Gambia, Benin and Togo, respectively. Thirteen (13) out of the 16 countries in West Africa have developed national blood policies. However, the implementation of these policies has been strongly restrained, partly due to the lack of funding, political will and open-mindedness to innovative ideas on safe donor recruitments.24–26 Only Benin, Togo, Senegal and Cape Verde had high proportions of voluntary non-remunerated donation. The value for Nigeria was only reported by the National Blood Transfusion Service Center in Abuja. The remaining sources of blood were via family replacement and commercially remunerated donors (Table 2).
Blood donation rate and proportion of voluntary donations in countries in West Africa.8
| Country | Donation per 1000 inhabitants | Proportion of voluntary donations (%) | No. of hospitals performing blood transfusion | No. of hospitals performing component preparation | National blood policy |
|---|---|---|---|---|---|
| Benin | 6.7 | 92.1 | 50 | 5 | Absent |
| Burkina Faso | 3.7 | 100 | 93 | 4 | Absent |
| Cape Verde | 5.6 | 77.3 | 6 | 6 | Present |
| Cote d’Ivoire | 4.4 | 100 | 200 | 8 | Present |
| Gambia | 7.2 | 24.1 | 11 | 0 | Present |
| Ghana | 5.4 | 27.1 | 257 | 3 | Present |
| Guinea Conakry | 2.4 | 14.7 | 42 | 1 | Present |
| Guinea Bissau | 2.7 | 19.9 | 7 | 7 | Present |
| Liberia | No data | No data | 38 | 0 | Absent |
| Mali | 3.1 | 30.4 | 13 | 3 | Present |
| Mauritania | 2.5 | 31.3 | 24b | 1 | Present |
| Niger | 3.5 | 36.3 | 47 | 1 | Present |
| Nigeria | No data | 94.2a | 22c | 1 | Present |
| Senegal | 4.5 | 79.4 | 141 | 2 | Present |
| Sierra Leone | 5.2 | 9.7 | 30 | 0 | Present |
| Togo | 5.9 | 98.3 | No data | 1 | Present |
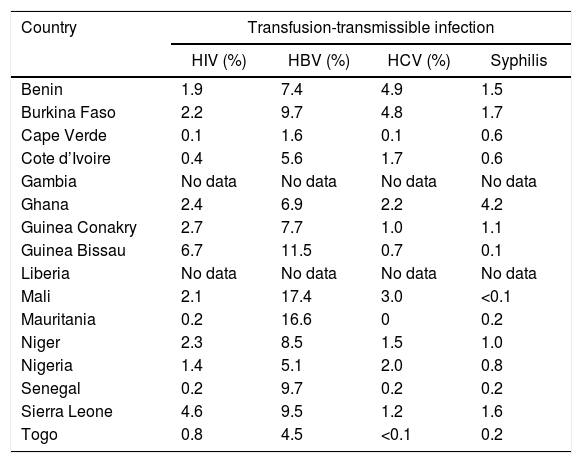
The proportion of transfusion-transmissible infections (TTIs) in donated blood units in the West African countries is high, ranging from 0.1 to 6.7 for HIV, 1.6 to 16.6 for HBV, 0 to 4.9 for HCV and 0.02 to 4.2 for syphilis (Table 3). A study in Nigeria2 in 2018 showed that 14.96% of donors were infected with at least one of the four major transfusion-transmissible infections. The TTI prevalences were 4.2%, 4.1%, 3.1% and 3.6% for HIV, HBV, HCV and syphilis, respectively. Another study in Burkina Faso27 in 2012 showed the TTI prevalences of 1.8%, 13.4%, 6.3% and 2.1% for HIV, HBV, HCV and syphilis, respectively. An additional study in Senegal28 reported the TTI prevalence of 3.5 per 100,000 donations for HIV, 102.45 per 100,000 donations for HBV and 138 per 100,000 donations for HCV.
Proportion of blood donations positive/reactive for transfusion-transmissible infections.8
| Country | Transfusion-transmissible infection | |||
|---|---|---|---|---|
| HIV (%) | HBV (%) | HCV (%) | Syphilis | |
| Benin | 1.9 | 7.4 | 4.9 | 1.5 |
| Burkina Faso | 2.2 | 9.7 | 4.8 | 1.7 |
| Cape Verde | 0.1 | 1.6 | 0.1 | 0.6 |
| Cote d’Ivoire | 0.4 | 5.6 | 1.7 | 0.6 |
| Gambia | No data | No data | No data | No data |
| Ghana | 2.4 | 6.9 | 2.2 | 4.2 |
| Guinea Conakry | 2.7 | 7.7 | 1.0 | 1.1 |
| Guinea Bissau | 6.7 | 11.5 | 0.7 | 0.1 |
| Liberia | No data | No data | No data | No data |
| Mali | 2.1 | 17.4 | 3.0 | <0.1 |
| Mauritania | 0.2 | 16.6 | 0 | 0.2 |
| Niger | 2.3 | 8.5 | 1.5 | 1.0 |
| Nigeria | 1.4 | 5.1 | 2.0 | 0.8 |
| Senegal | 0.2 | 9.7 | 0.2 | 0.2 |
| Sierra Leone | 4.6 | 9.5 | 1.2 | 1.6 |
| Togo | 0.8 | 4.5 | <0.1 | 0.2 |
<0.1 = 0.02.
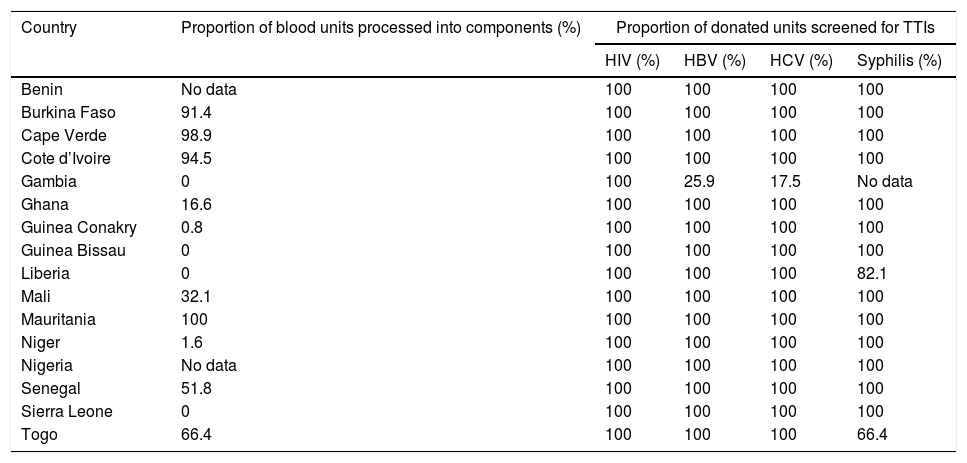
Most of the countries in West Africa do not effectively practice blood component preparation. Especially Liberia, Guinea Bissau, Guinea Conakry, Sierra Leone, Gambia, Niger and Ghana were found wanting in this. They possibly lack facilities for component preparation and hence, perform the transfusion of whole blood.7,24 Only Mauritania, Burkina Faso, Cape Verde, Cote d’ Ivoire, Togo and Senegal were found above par in terms of blood component preparation. Most of the countries screened all donated blood units for HIV, HBV, HCV and syphilis, except Gambia, Togo and Liberia, where HBV, HCV and syphilis screening were skipped at times (Table 4).
Proportion of donated blood units processed into components and also screened for TTIs.8
| Country | Proportion of blood units processed into components (%) | Proportion of donated units screened for TTIs | |||
|---|---|---|---|---|---|
| HIV (%) | HBV (%) | HCV (%) | Syphilis (%) | ||
| Benin | No data | 100 | 100 | 100 | 100 |
| Burkina Faso | 91.4 | 100 | 100 | 100 | 100 |
| Cape Verde | 98.9 | 100 | 100 | 100 | 100 |
| Cote d’Ivoire | 94.5 | 100 | 100 | 100 | 100 |
| Gambia | 0 | 100 | 25.9 | 17.5 | No data |
| Ghana | 16.6 | 100 | 100 | 100 | 100 |
| Guinea Conakry | 0.8 | 100 | 100 | 100 | 100 |
| Guinea Bissau | 0 | 100 | 100 | 100 | 100 |
| Liberia | 0 | 100 | 100 | 100 | 82.1 |
| Mali | 32.1 | 100 | 100 | 100 | 100 |
| Mauritania | 100 | 100 | 100 | 100 | 100 |
| Niger | 1.6 | 100 | 100 | 100 | 100 |
| Nigeria | No data | 100 | 100 | 100 | 100 |
| Senegal | 51.8 | 100 | 100 | 100 | 100 |
| Sierra Leone | 0 | 100 | 100 | 100 | 100 |
| Togo | 66.4 | 100 | 100 | 100 | 66.4 |
The COVID-19 pandemic has had an enormous impact on almost all aspects of life, including the blood transfusion practice, number of blood donations, blood safety and movement of consumables used for blood transfusion screening. Based on data from a previous survey on the blood transfusion practice by the WHO and an early alert from the sub-Saharan region on the scarcity of blood with the onset of the pandemic,29,30 we discuss the preparedness and panacea to tackle the possible blood supply shortage.
Just as previous epidemics (SARS epidemic of 2003, influenza pandemic of 2009), the COVID-19 pandemic has been widely reported to lead to the decline in the number and availability of blood donors.11,31–34 This decline in blood donors partly stems from the fear in the healthy population that they might get infected while visiting a high-risk areas, such as hospitals and blood transfusion centers, and even in transit.11 Furthermore, the mass lockdown in many countries has also made it difficult for blood donors to move from place to place and blood transfusion centers to run donation drives and camps. The poor voluntary blood donation observed in most of the countries in West Africa makes it difficult to adapt to the pandemic crises, as voluntary blood donation would be best fitted to adapt in this period, considering that it is mostly driven by altruism.
Moreover, the government restrictions in most parts of the world in the attempt to curtail the COVID-19 pandemic also adversely affects the supply chain of consumables used in blood transfusion services. The ban on international flights and restrictions in interstate travels limits the conveyance and supply of blood transfusion consumables and, in some cases, adds extra cost. In addition, the decreased workload as a result of the pandemic and wastage of reagents meant for daily maintenance of automated equipment, as well as the unnecessary expiration of reagents due to a decreased workload add to the list.11 The possibility of maneuvering these challenges lies in effective, functional national blood transfusion service centers and effective blood transfusion policy.
The safety of the blood donor and the recipient is paramount in the blood transfusion practice. Hence, there is a need for the constant monitoring of donors and recipients in the event one develops an infection suggestive of a transfusion-transmissible infection. Although parenteral transmission of COVID-19 has not been established, there are theoretical reports of detection of the viral RNA in blood.16,35–38
In view of the blood transfusion status in the countries of West Africa listed above, it is empirically difficult for these countries to respond effectively to an emergency, given the scarcity of blood posed by the COVID-19 pandemic. The pillars of an effective and efficient blood transfusion service are anchored on voluntary non-remunerated donation, a well-established and well managed nationally coordinated blood transfusion service and a well developed and implemented national blood transfusion policy. As evident in the data above, most of the countries in West Africa rely on familial replacement and commercially remunerated blood donors. These classes of donors are not altruistic, but rather are driven by the remuneration impulse. Hence, the same are classified as a high-risk group. Remunerated blood donors have been documented to express higher seropositivity for transfusion-transmissible infections than voluntary donors.2,39–41 Furthermore, this pandemic period is quite a restricted one and donors who are not motivated to save lives might not be willing to submit themselves to the rigorous process of blood donation at this time. Moreover, the lack/poor practice of blood components separation in most of the countries is counterproductive in this pandemic period, in which the demand for blood is relatively low. The donation and transfusion of whole blood for most indications for blood transfusion is a common practice in most hospital-based blood transfusion services (which are the majority) in most sub-Saharan countries.5,42,43 Aside from the human resources and logistic aspects, there is the absence or non-implementation of blood policies in most of the countries in West Africa, as well as the absence of contingency plans for blood transfusion services in crises, such as the current COVID-19 pandemic period.7 Such neglect in a region primed with high infant and maternal mortality7 and infectious disease outbreaks, weighs in on the downside of the situation. Benin, Guinea Conakry, Nigeria, Liberia and Togo are still battling with the latent Lassa fever epidemic.
PanaceaInclusion of blood transfusion services in emergency response teamAs part of the palliative measures to curtail the COVID-19 crises, the WHO has issued guidelines on maintaining a safe and adequate blood supply during the COVID-19 pandemic. It advised a national, rather than a sub-national or local approach. The need to include blood services in the national outbreak response through experts linked to the national emergency response team.44 This will go a long way to air the importance of blood transfusion in a time of crisis and promote the inclusion of same on priority list.
Establishment of blood management information systemA lesson learnt from China on blood management during the pandemic was the establishment of the blood management information system. The implementation of such an information system helps optimize the blood supply chain. This allows for the conveyance of blood or donors from a bountiful area to a place of need.31 Such an arrangement helps spread out and balance excesses and deficits in the blood supply across the various parts of the country.
Practice of social media medicineThe world has become a global village and social media has become an important media for conveying and receiving information. One of the lessons learnt from the Chinese medical team in blood management in the current pandemic was the use of social media to recruit blood donors. The Chinese Society of Blood Transfusion (CSBT), in lieu of blood drives, made a public appeal for blood donation via the We Chat (a social media), in which indicated donors were invited and appointments were made for donations, while observing social distancing.31 The same can be replicated in West Africa using the more popular social media in the region, such as Facebook, Twitter, Instagram and others.
Use of pharmacological agentsIn pandemics, such as the current COVID-19, one of the best approaches to minimize the blood shortage is the use of pharmacological agents instead of transfusing blood. The use of desmopressin in the treatment of mild hemophilia, in lieu of blood transfusion, and the use of the vasoconstrictor agent aprotinin to reduce blood loss at the operative site have been recommended. Furthermore, fluid replacement volume expanders such as crystalloids or colloids are good alternatives to blood transfusion in this pandemic period. In addition, the use of hematinic is a good alternative for anemic patients.32
Issue of appointment letters and mobile blood drivesSome blood centers have devised an innovative method of recruiting donors via the issue of appointment letters to voluntary blood donors to get individual access to the blood centers during the lockdown.33 Another perspective to this is the mobile blood drive that entails meeting the voluntary blood donors at home. In the pandemic period, regular voluntary donors are preferable. First-time donors and those who have not donated blood in the last five years are high-risk donors in the period of pandemic.45
The use of “lowest hanging fruit” optionSome clinicians have suggested the application of the “lowest hanging fruit” option to balance the demand and supply of blood and blood products during the pandemic. A typical example is the single unit policy called “why give 2 when 1 will do?” for erythrocytes does more to reduce overall transfusion requirements than simply monitoring the hemoglobin trigger.46 Other ways to achieve this approach entail cell salvage during surgery, minimally invasive surgical procedures and more.46
Nevertheless, this study might be potentially prone to varying limitations. First, the study extracted data retrospectively and missing data were observed in some cases. Secondly, the theme of the study is anchored on the previous survey, an early alert on blood availability during the pandemic and the authors’ day-to-day perceptions to demonstrate the weakness of the region in the blood transfusion practice in view of tackling the COVID-19 challenge.
ConclusionThe analysis of the blood transfusion practice in the pre-COVID-19 period in the countries in West Africa shows the unpreparedness to arrest the wave of blood chain shortage that is arising across the globe, even in developed countries, owing to the COVID-19 pandemic. The loophole the pandemic has exposed in terms of the blood transfusion practice has been harnessed by developed countries and should serve as an opportunity to strengthen the blood transfusion practice in West Africa. There is the need to adopt innovative ideas, as well as to employ advocacy and novel campaigns.
Author contributionsHUO conceived the study, performed the literature search, analyzed the data, designed the map and prepared the initial manuscript draft; IMO performed the literature search and analyzed the data; EAA analyzed the data; COO analyzed the data, and; IKU analyzed the data. All authors read and approved the final manuscript.
Conflicts of interestThe authors declare no conflicts of interest.