Dengue is the most fatal virus disease spread by mosquito bites and Aedes aegypti is the main transmitting agent. It is an endemic disease in the tropical and subtropical regions, currently affecting more than 100 countries. Although most patients present mild forms of the disease, a considerable proportion of individuals has severe alterations in the blood count. The aim of this study was to evaluate the consumption pattern of blood components in epidemic and non-epidemic periods and to verify if there was an impact on dengue cases and the death rate.
MethodThis is a retrospective cross-sectional study conducted through the collection and analysis of data from the Brazilian Ministry of Health from 2008 to 2019 on new cases and deaths from dengue, as well as the consumption of blood components in the period mentioned by hemovigilance bulletins of the Brazilian authority.
ResultsRegarding the results, no significant difference was found between the absolute amount of blood components used in years with an epidemic peak. Regarding the relative values, an important variation was shown among the distributive consumption patterns of blood components in the outbreak years. In the univariate linear regression analysis, there was statistical significance between the increase in the number of dengue cases and deaths from dengue with the increase in the consumption of red blood cell concentrates (RBP), platelet concentrates (PP), fresh frozen plasma (FFP) and cryoprecipitate (Cryo) (p-value < 0.05). The increase in dengue cases was related to the increase in Cryo consumption with clinical significance (R² > 0.5), but dengue deaths were not correlated to the same. In multivariate analysis, all regression models had clinical and statistical significance.
ConclusionThe data obtained in the present study demonstrate that there is a relevant relationship between the increase in cases and deaths from dengue with the blood components usage, especially PP, FFP and cryoprecipitate.
Dengue is the most fatal viral illness spread through mosquito bites. The main transmitting agent is the arthropod Aedes aegypti, but it can also be transmitted by mosquitoes of the Anopheles genus. The disease is endemic in tropical and subtropical environments.1 Since the first years of the description of Dengue, many epidemic outbreaks have followed and the condition is currently present in more than 100 countries in these areas of the planet.
Although most patients did not develop severe forms of the disease, approximately 8% of patients can develop critical complications, demanding hospitalization and treatment in the intensive care unit.2 One of the main findings in patients with dengue fever (DF) are changes in the blood count, the most common being thrombocytopenia, which can occur in 45.2% to 78% of the patients.3,4 The dengue shock (DS) is especially common in severe forms and changes in cell counts and coagulation tests can prompt the physician to perform blood transfusions.5
There are studies showing that up to 21.4% of blood component transfusions were performed outside the WHO recommendations for the transfusion management of patients with DF/DS.5 In this sense, especially during outbreaks, there is an increase in the pressure for transfusion in blood banks, which can generate additional costs for the health system if the transfusion is outside the safe criteria for transfusion in these cases.6 Thus, this study aimed to assess the consumption pattern of blood components in epidemic and non-epidemic periods and the impact of the number of dengue cases (DCs) and dengue deaths (DDs) caused in the evaluation period.
MethodsThis is a retrospective cross-sectional study which was performed by searching for data on public platforms of the Brazilian Ministry of Health (Brazilian Health Authority, BHA) from 2008 to 2019 on new DCs and dengue deaths, as well as the blood components usage in the period mentioned in the BHA hemovigilance bulletins.7–20 The diagnosis of dengue fever (DF) in the period was performed according to the guidelines of the BHA at the time, using laboratory tests for NS1, immunoassays for IgM antibodies and clinical epidemiological diagnosis. During epidemic periods, there was a higher prevalence of clinical epidemiological diagnosis, as directed by health authorities.
The dengue death rate (DDR) was described as the total value of deaths from DF in the year divided by the number of cases of DF in the same year. The unit was described in relation to 100,000 cases. Data obtained from hemovigilance bulletins included transfusions of blood components (BCT), red blood cell concentrates (RBP), platelet concentrates (PP), fresh frozen plasma (FFP) and cryoprecipitate (Cryo). The PP value was obtained by adding all the subtypes used, such as platelets by apheresis, random and buffy coat.
To demonstrate the variability of the indices used, we considered the values obtained in 2008 as reference values, so that all other values for BCT, RBP, PP, FFP and Cryo were evaluated according to the increase or decrease in value in relation to the values from 2008, year zero (Y0). Thus, the increment or decrement of the variables was determined considering the baseline value referring to Y0 and, in subsequent years, the variation in relation to the increase/decrease. This variation was represented as deltaBCT, deltaRBP, deltaPP, deltaFFP and deltaCryo. Thus, considering the year 2008 as the baseline year, the percentage variation was obtained by evaluating the variation in the absolute value of each variable in relation to the previous value, thus assessing the percentage variation, which was reported as delta%BCT, delta%RBP, delta%PP, delta%FFP, delta%Cryo, delta%DC and delta%DD.
Statistical analysisDescriptive variables were described in terms of median, minimum and maximum values. The differences between groups were analyzed using the Mann-Whitney test for non-parametric variables. To assess the presence of predictability in the pattern of blood components usage during the epidemic years in DF, the model was performed using univariate (UVLR) and multivariate (MVLR) linear regression. The UVLR and MVLR models with clinical significance were considered when the coefficient of determination (R²) was above 0.5. The p-values were considered statistically significant when below 0.05. For a p-value between 0.05 and 0.1, we considered that, in the description of the regression model, there was a trend of model fitness. Confidence interval values were defined to be 95%. Statistical analysis was performed using the R version 4.1.0 software. The R and MedCalc 20.009 software were used to perform the graphics.
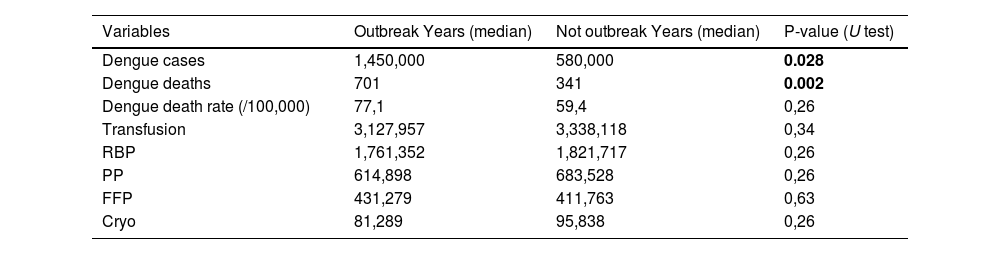
ResultsDuring the period evaluated, between 2008 and 2019, the median of DCs was 59,000 (24,000 – 2300,000), epidemic years presenting the median of 1225,000 and non-epidemic years, 490,000. The death rate from dengue in years considered epidemic was 29.8% higher than in non-epidemic years (77.1 versus 59.4). During the period evaluated, there was no significant difference among the absolute amounts of blood components used in years with outbreaks, as shown in Table 1. In the analysis between the epidemic and non-epidemic groups, there was only a statistically significant difference when evaluating the new cases and deaths from dengue.
Baseline characteristic. RBP, red blood cell packed; PP, platelets packed; FFP, fresh frozen plasma; Cryo, cryoprecipitate. U test realizado com base em Mann-Witney.
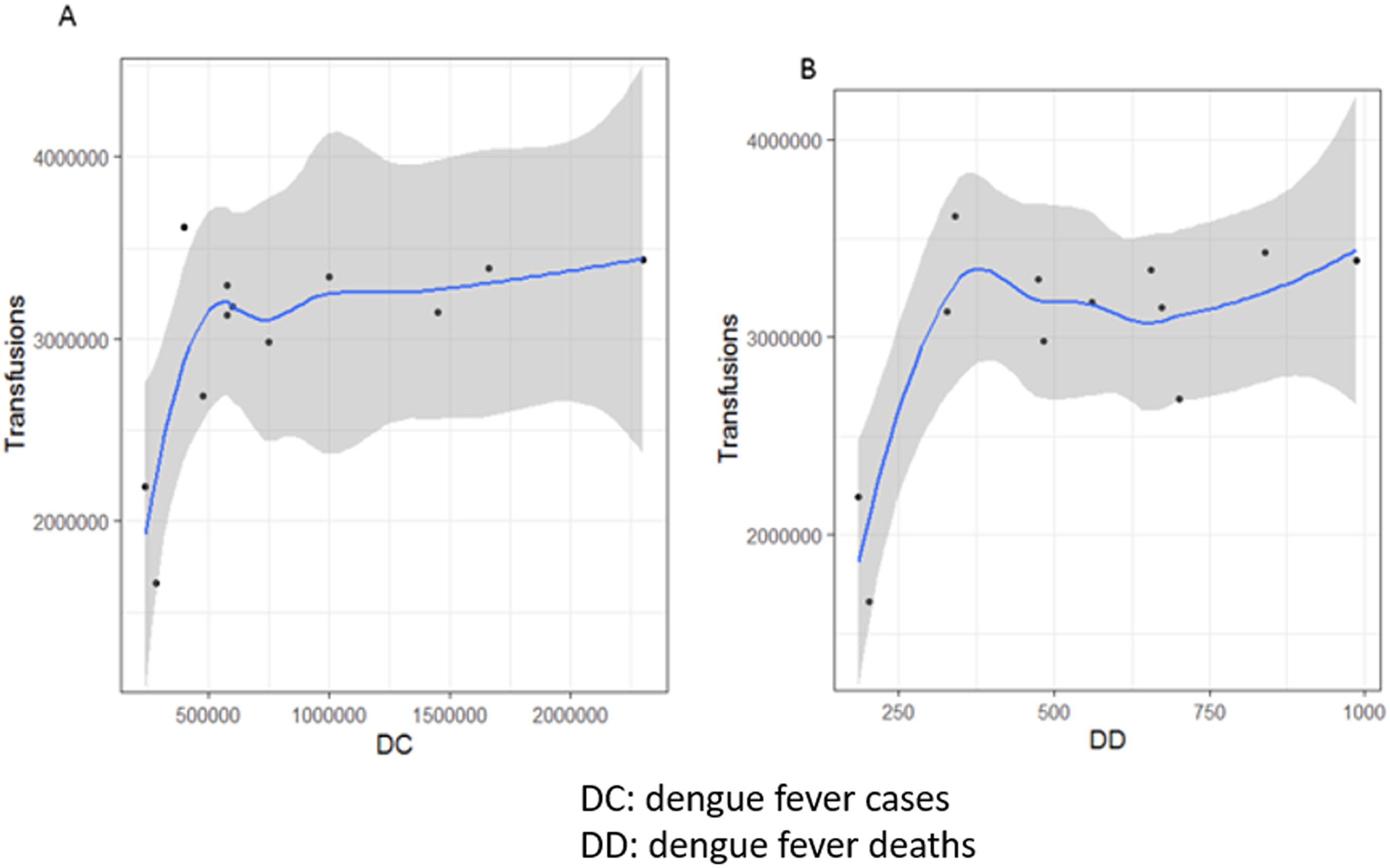
Figure 1 demonstrates the association between the increase in DCs and DDs with increased blood components usage. When performing linear regression analysis, there was no statistical or clinical significance among the data evaluated (p-value > 0.05 and R² < 0.5)
LOWESS distribution demonstrating the behaviour of the increase in transfusion requirements in relation to the increase in new DCs. Graph A shows the increase in transfusions in relation to the increase in DC; Graph B shows the increase in transfusions in relation to the increase in cases of death from dengue (DD).
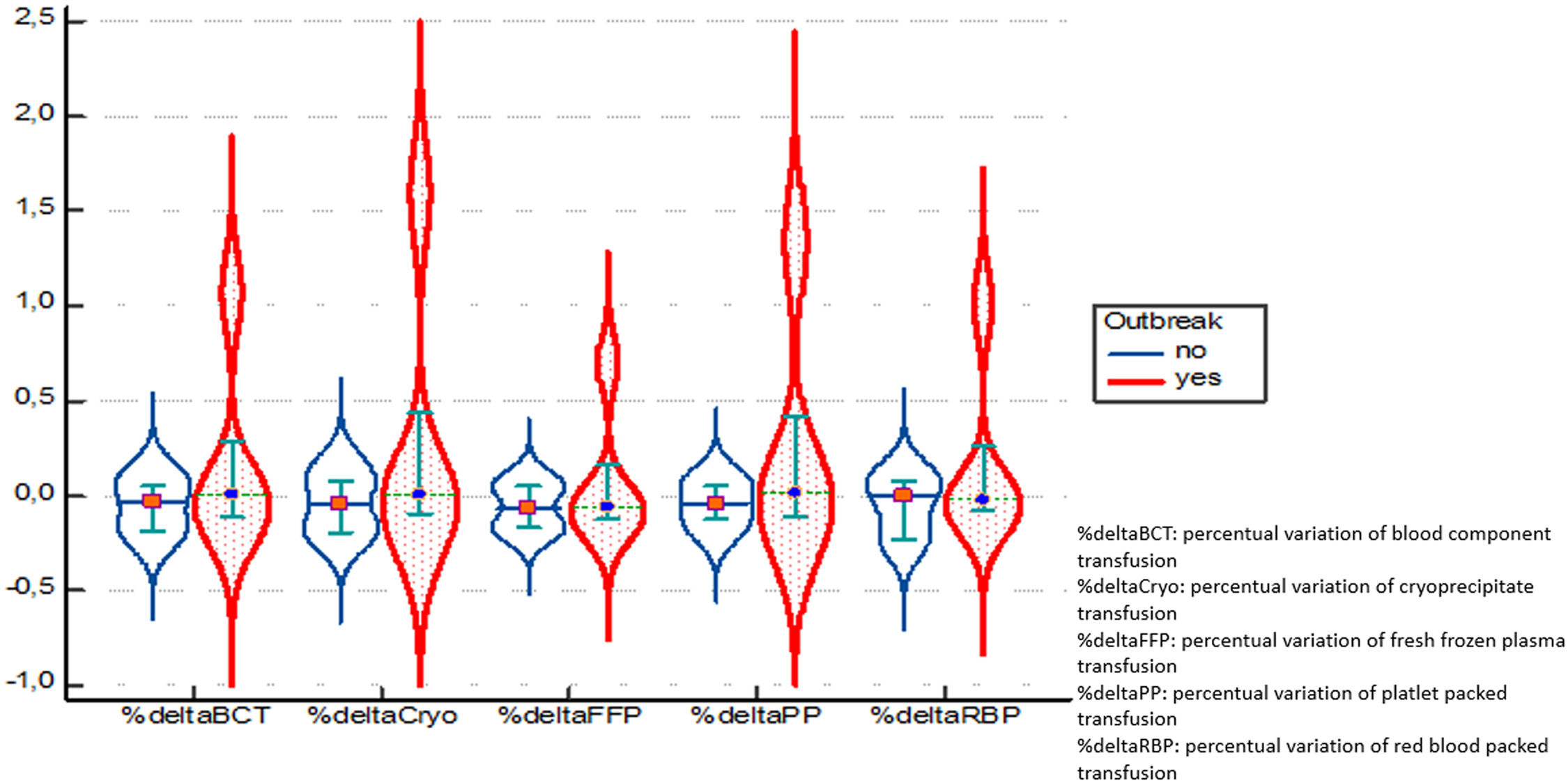
When transforming the absolute values into relative values, based on the year 2008, we have an important variation among the distributive patterns of blood components usage in the years with epidemic outbreaks, as shown in Figure 2. The pattern of blood components usage also demonstrated the specific pattern of each epidemic period.
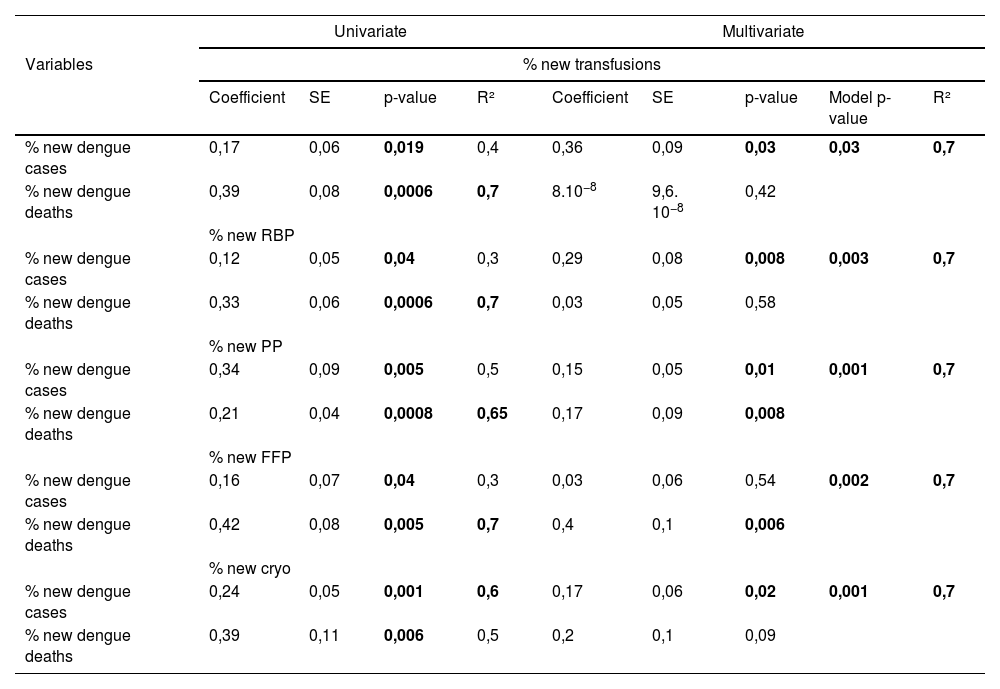
To assess the relationship between the increase in cases, deaths and the increased blood products usage, univariate and multivariate linear regression analysis were performed. The results of the evaluation are described in Table 2. In the univariate analysis, there was statistical significance between the increase in DCs and DDs, with increased demand for transfusion of RBP, PP, FFP and Cryo (p-value < 0.05); however, there was only clinical significance (R² > 0.5) in the relationship between new DDs and the increased consumption of BCT, RBP, PP and FFP. The increment in DCs was correlated to the increase in Cryo consumption with clinical significance (R² > 0.5), but DDs were not correlated to the same.
Univariate and multivariate linear regression analysis. Data with clinical and statistical significance have been bolded for demonstration.
When performing the multivariate analysis, all regression models had clinical (R² > 0.5) and statistical (p-value < 0.05) significance. In this sense, it was demonstrated that the increase in the consumption of all blood components was positively associated with the increase of DCs and/or DDs. It is important to note that the increase in deaths from dengue was positively associated with the increase in the consumption of PP, FFP and cryoprecipitate in the multivariate model.
DiscussionDengue fever is a potentially fatal disease, especially when it evolves to severe forms, of which 15% to 19% are associated with bleeding.21,22 However, other complications are also prevalent in patients with DF, such as hepatitis, acute kidney injury and leakage syndrome.23 In a study by Chang et al., the main factors associated with a worse outcome in severe DF were acute hepatitis and kidney injury, so that bleeding in this group was not associated with an increased chance of death (p-value = 0.419).24 Evolution to coagulopathy in patients with DF is a potentially serious complication, which often exposes the patient to unnecessary transfusions.
A study carried out by Tewari25 analyzed the hematological findings in patients with DF, describing that only 3.2% met the WHO criteria for severe dengue and that 9.2% had hemorrhagic manifestations requiring platelet transfusion.
There are few robust studies evaluating transfusion in dengue26; however, there is evidence that there is an unnecessary use of blood components in the management of minor bleeding in DF. Approximately 22 to 31.96% of platelet transfusions may be performed inappropriately, increasing hospitalization costs and risks of transfusion reactions and negatively compromising the stock of blood banks.27,28 When there is no protocol for the rational use of blood components, the number of inappropriate transfusions can reach as much as 89% of the transfusions. During the evolution of severe cases, in addition to platelets, FFP and Cryo are also used to manage coagulopathy in many patients,29 especially those who progress with leakage syndrome, where coagulopathy is more evident and with a higher rate of mortality.30
As demonstrated in this study, the increase in cases compared to previous years has put an important pressure on the stocks of blood banks, especially due to the higher consumption of blood components; however, other important factors are the decline of suitable blood donors (due to the increase of donors in convalescence from DF) and the period beyond the safe window for blood transmission of dengue.6,31 Thus, stocks are three times more pressured, making it is indispensable to manage patients with more restrictions according to WHO guidelines.31,32
There is robust evidence for the restrictive management of thrombocytopenia in patients with dengue, demonstrating that prophylactic transfusion should not be considered in therapeutic support of these patients.33–36 Another finding of our study is the increased consumption, especially of FFP and Cryo, during epidemic periods. A study by Chuansumit et al. 37 evaluated the consumption of other blood components in addition to PP, describing that 10.6% of the assessed patients were managed with transfusion, of which 29.4% received FFP/Cryo. This finding corroborates our data on increased consumption of these blood components, especially with the increase in DD, which raises the possibility these cases could be cases with intense coagulopathy that required intensive care unit treatment.
The standardization in transfusion management of DF/DS patients is urgently needed. In countries where there is no adequate regulation of this transfusion policy, mortality rates can reach 10 to 15% in epidemic periods,38 mainly tending to be higher in patients older than 60 years.39 In addition to the proper transfusion management of patients with DF, it is extremely important to enhance the population's awareness of the necessity to eradicate the mosquito vector (40). New proposals for vector control have been developed in recent years, such as the use of the bacterium Wolbachia1 with the aim of vector population control. More extensive studies are needed to define the real impact of this ecological therapy, but utmost enthusiasm must be employed in this endeavor.
ConclusionDF is a viral disease that is most often associated with mild symptoms; however, some patients may develop severe manifestations, especially coagulopathy. In this case, many of these patients need to be admitted to wards and others to an intensive care unit, where they are often managed with blood component support. The data obtained in the present study demonstrate that there is a relevant relationship between the increase in cases and deaths from dengue with the blood components usage, especially PP, FFP and cryoprecipitate. Thus, it is important that blood banks be able, during epidemic periods, to prepare for the requested transfusions. It is also important to enhance awareness among physicians and health professionals as to which clinical conditions associated with DF can benefit from correct blood components management.
LimitationsAs this is a retrospective study, the strength of determination between cause and effect should be considered based on the limitations of this type of study. Despite the quality of the data in the country's public registries, it is important to emphasize that there is difficulty in notifying and properly recording the DC, as well as difficulties inherent in the diagnosis, especially in epidemic moments. Mortality registration tends to have greater reliability, given the mandatory registration of death. Due to the continental character of the Brazilian territory, the generalized analysis of data in a national context may not reflect the inherent characteristics of each region or state. To improve the visualization of the variation phenomena according to epidemic years or not, data was standardized in reference to the year 2008. In this sense, the dependent and independent variables were analyzed according to their variation in relation to previous years.