The SARS-CoV-2 pandemic has been affecting the health and economic, as well as social, life of the entire globe since the end of 2019. The virus causes COVID-19, with a wide range of symptoms among the infected individuals, from asymptomatic infection to mortality. This, along with a high infection rate, prompted efforts to investigate the potential mechanisms of the different clinical manifestations caused by SARS-CoV-2 among the infected populations.
HypothesisOne of the possible mechanisms that has been reported is the ABO blood system polymorphism. Indeed, one of the major proposed mechanisms is the presence of naturally occurring anti-A antibodies in individuals of groups O and B, which could be partially protective against SARS-CoV-2 virions.
Objective and MethodThis article aimed to review the published data on the potential effect of the ABO blood group system on the susceptibility to COVID-19 and the disease progression and outcomes.
ResultsThe reviewed data suggest that individuals of blood group A are at a higher risk of infection with SARS-CoV-2 and may develop severe COVID-19 outcomes, whereas blood group O is considered protective against the infection, to some extent. However, some of the available studies seem to have been influenced by unaccounted confounders and biases.
ConclusionTherefore, further appropriately controlled studies are warranted to fully investigate the possible association between the ABO blood groups and COVID-19 susceptibility and severity.
The current 21st century has so far witnessed three major pandemics by coronaviruses. The first pandemic occurred in 2002 caused by the Severe Acute Respiratory Syndrome coronavirus (SARS-CoV). The infection began in China then spread around the globe until it was ended in 2013.1 In 2012, a fatal pandemic caused by the Middle East Respiratory Syndrome coronavirus (MERS-CoV), first reported in the Arabian Gulf region with a mortality rate of approximately 30%.1 In 2019, yet another pandemic originated in China where Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) disseminated worldwide rapidly causing coronavirus disease (COVID-19).2 By June 2021, the infected cases exceeded 170 million, with more than 3.7 million deaths worldwide.3 The review aims to provide an overview of the current knowledge and understanding of the association between the ABO blood group system and the susceptibility to, and severity of, SARS-CoV-2 infection, and the possible mechanisms of interaction between different ABO blood groups with SARS-CoV-2.
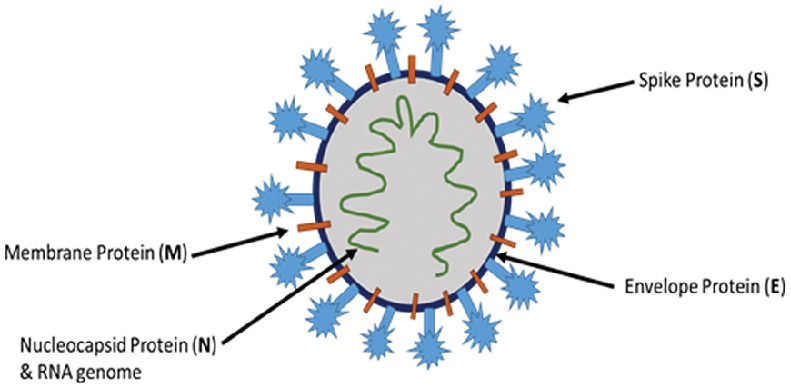
Pathogenesis of COVID-19 infectionSARS-CoV-2 is one of coronavirus family members, which are sub-divided into four genera, alpha (α), beta (β), gamma (γ) and delta (δ), of which only the α and β genera are known to cause infections in human, SARS-CoV-2 belonging to the β coronaviruses.4 Coronaviruses are enveloped and have a positive sense single-stranded RNA genome.5 The virus genome consists of ten open reading frames (ORFs) where ORF1a/b alone accounts for around two-thirds of the virus's total RNA.6 The translation of the virus RNA produced by ORF1a/b results in two polyproteins, ppla and pplab, which are further transcribed to 16 non-structural proteins necessary for production of the viral replicase transcriptase enzyme.6 The remaining one-third of the viral RNA is required to transcript the virus's structural proteins. SARS-CoV-2 and coronaviruses in general, have four essential structural proteins, Figure 1, namely, Spike (S), Envelope (E), Matrix (M) and Nucleocapsid (N).5 The S protein consists of 2 subunits, the S1 subunit expresses the receptor binding domain (RBD) required for the virus-host binding and the S2 subunit is needed for the virus fusion with the host cell membrane.7 The SARS-CoV-2 enters host cells by interacting with the angiotensin-converting enzyme 2 (ACE2) receptor located on human tissue cells.8 The virus binds to the ACE2 through S1 glycoprotein, while the invasion is accomplished through the S2 glycoprotein.78
The COVID-19 pandemic is affecting human health across the globe, with some people being more susceptible to the infection than others, although variation in clinical features in SARS-Cov-2-infected individuals is commonly observed. Epidemiological studies show that around 80% of the infected individuals are asymptomatic, but contagious, while others experience mild symptoms, such as cough and fever, or severe respiratory complications, such as the acute respiratory distress syndrome (ARDS).9 This variation in COVID-19 clinical features was thought to be caused by differences in the body immune response to the infection. Early effective immune response can reduce the viral load and prevent the infection from reaching the lungs, whereas extreme immune response can cause an excessive inflammatory reaction leading to severe adverse consequences.10 Moreover, statistics show increased prevalence of diabetes, hypertension and liver diseases among the severe COVID-19 cases, suggesting that metabolic disorders have a role in directing the response of the body to the infection.11
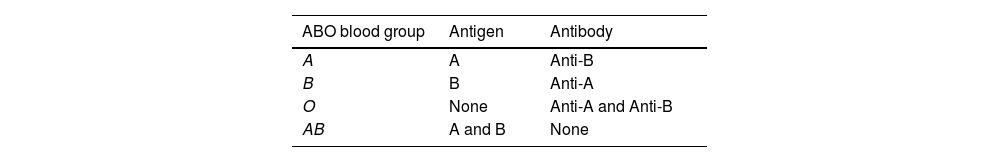
ABO blood group systemThe ABO blood group system was discovered in 190112 and it consists of the 3 alleles A, B and O, all coded by the ABO gene. The combination of these 3 alleles on red blood cells (RBCs) results in 6 possible genotypes and four phenotypes, resulting in antigens on (RBCs) with antibodies in plasma. Table 1 shows the antigen and the corresponding antibodies in each blood group.
Since the time of its discovery, attempts have been made to study the potential linkage of the ABO blood group system with various disorders and infections. The polymorphism of the ABO blood group was reported to be associated with the susceptibility to, and outcomes of, several diseases and infections, including tumors, coronary heart disease, hepatitis B virus, SARS-CoV and Helicobacter pylori.1314 In addition, growing evidence suggests a potential role of the ABO blood group in the SARS-CoV-2 infection susceptibility and severity.15
ABO and COVID-19 infection and susceptibilityThe impact of the ABO blood group system on the COVID-19 susceptibility was first reported by Zhao et al. in confirmed COVID-19 cases at three different hospitals in China.16 It was found that patients with blood group A had a higher COVID-19 infection rate, as compared to patients with blood group O, especially in a region where the prevalence of blood groups A and O among the population is 31% and 34%, respectively. Patients with blood group A accounted for 37% of total COVID-19 cases, while patients with blood group O represented only 26% of the confirmed COVID-19 cases. These findings suggest that blood group O may provide protection against the infection, while people with blood group A are more susceptible to get infected with COVID-19. The possibility of the ABO blood group association was further demonstrated in a case-control study reported by Wu et al. that involved 187 confirmed COVID-19 cases and demonstrated that 37% of COVID-19 patients had blood group A, while only 22% of the patients had the blood group O.17 Furthermore, in another case-control study that included 265 COVID-19 patients, Li et al. found that patients with blood group A accounted for 39% of COVID-19 cases, while those with blood group O represented 26%.18
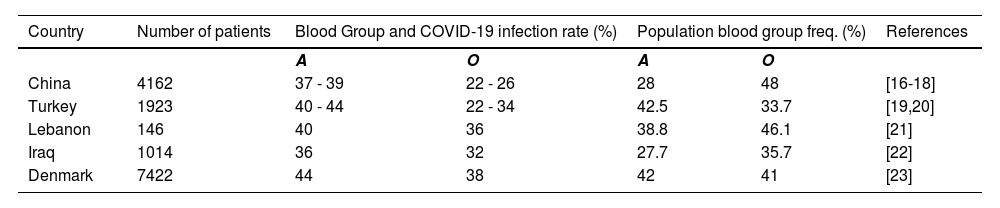
In line with findings from China, studies from Turkey, Lebanon, Iraq and Denmark also demonstrated that patients with blood group A represented the highest proportion of COVID-19 positive cases, when compared to the other blood groups and that furthermore, the blood group with the lowest number of infected individuals was reported to be the O type,19-22 as shown in Table 2. In addition, Barnkob et al. reported that, although each of the blood groups O and A represent 42% of the Danish population, the infection rate among group O was 38%, for group A it was 44%, suggesting that group O decreases susceptibility to the SARS-CoV-2 infection.23 Low prevalence of the O blood group among COVID-19 cases was also reported in studies in the USA and Spain.24-26 Furthermore, a recent meta-analysis of the susceptibility of the ABO blood group to the COVID-19 infection concluded that blood group A individuals were more susceptible to the COVID-19 infection.27
Prevalence of A and O blood groups in COVID-19 patients.
| Country | Number of patients | Blood Group and COVID-19 infection rate (%) | Population blood group freq. (%) | References | ||
|---|---|---|---|---|---|---|
| A | O | A | O | |||
| China | 4162 | 37 - 39 | 22 - 26 | 28 | 48 | [16-18] |
| Turkey | 1923 | 40 - 44 | 22 - 34 | 42.5 | 33.7 | [19,20] |
| Lebanon | 146 | 40 | 36 | 38.8 | 46.1 | [21] |
| Iraq | 1014 | 36 | 32 | 27.7 | 35.7 | [22] |
| Denmark | 7422 | 44 | 38 | 42 | 41 | [23] |
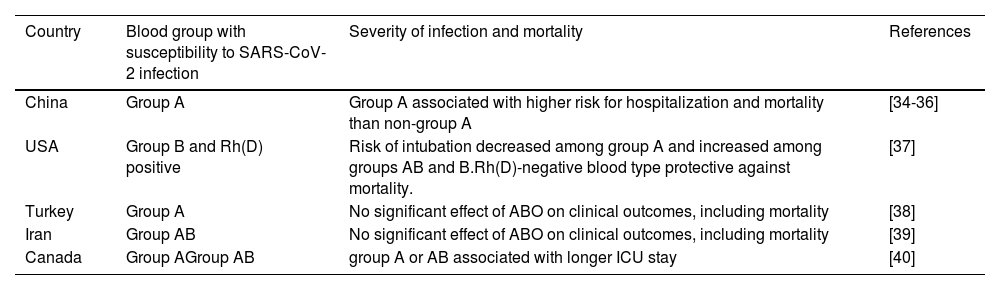
A number of studies evaluated the association between ABO blood groups and the COVID-19 severity and mortality. Currently, there are conflicting reports of blood group association with severe COVID-19 outcomes, as shown in Table 3. Indeed, it was reported that the highest percentage of COVID-19 patients with severe symptoms was blood group A,1328 while blood group O was reported to have the lowest severity.19 Similarly in Lebanon, it was reported that blood group A was associated more critical cases of COVID-19.21 In contrast, some studies in different countries reported no association between ABO blood groups and the COVID-19 severity or mortality.1617202223,29-32 One study reported reduced severity and risk of intubation in COVID-19 cases with blood group A.24 A meta-regression analysis of 101 nations that used the known populational blood group distributions, the study analyzed data from ∼9 million COVID-19 cases and ∼450,000 deaths, adjusting for 14 potential confounders, including life expectancy at birth, hypertension and obesity prevalence, the study concluded there was no association of groups A or B with overall mortality. However, group O was associated with lower mortality.33
The association between blood groups and SARS-CoV-2 infection and severity.
| Country | Blood group with susceptibility to SARS-CoV-2 infection | Severity of infection and mortality | References |
|---|---|---|---|
| China | Group A | Group A associated with higher risk for hospitalization and mortality than non-group A | [34-36] |
| USA | Group B and Rh(D) positive | Risk of intubation decreased among group A and increased among groups AB and B.Rh(D)-negative blood type protective against mortality. | [37] |
| Turkey | Group A | No significant effect of ABO on clinical outcomes, including mortality | [38] |
| Iran | Group AB | No significant effect of ABO on clinical outcomes, including mortality | [39] |
| Canada | Group AGroup AB | group A or AB associated with longer ICU stay | [40] |
Most of the studies that assessed the association of the ABO and COVID-19 infection and severity suggest that group O individuals present with a lower risk of SARS-CoV-2 infection and less severe COVID-19 disease. However, these findings are not conclusive. These conflicting findings could be attributed to the different populations and their geographical locations, the controls that were selected for comparison and the presence of confounders, such as comorbidities, that some studies did not adjust for. Another potential factor for these varying findings is that some of the studies used randomly selected volunteer blood donors as controls. Volunteer blood donors are not necessarily representative of general populations, as some blood banks selectively recruit group O donors, which may lead to the group O epidemiological predominance.41 This would increase the risk of reporting a false apparent decrease of group O patients, when compared to non-O blood groups. These different variables can seriously affect outcomes and therefore, it is vital to appropriately design observational case-control studies with mitigating measures in place to minimize bias, particularly when selecting control groups, as a major flaw that has been identified is selecting control information by obtaining the population distribution of ABO blood groups from blood bank records.42
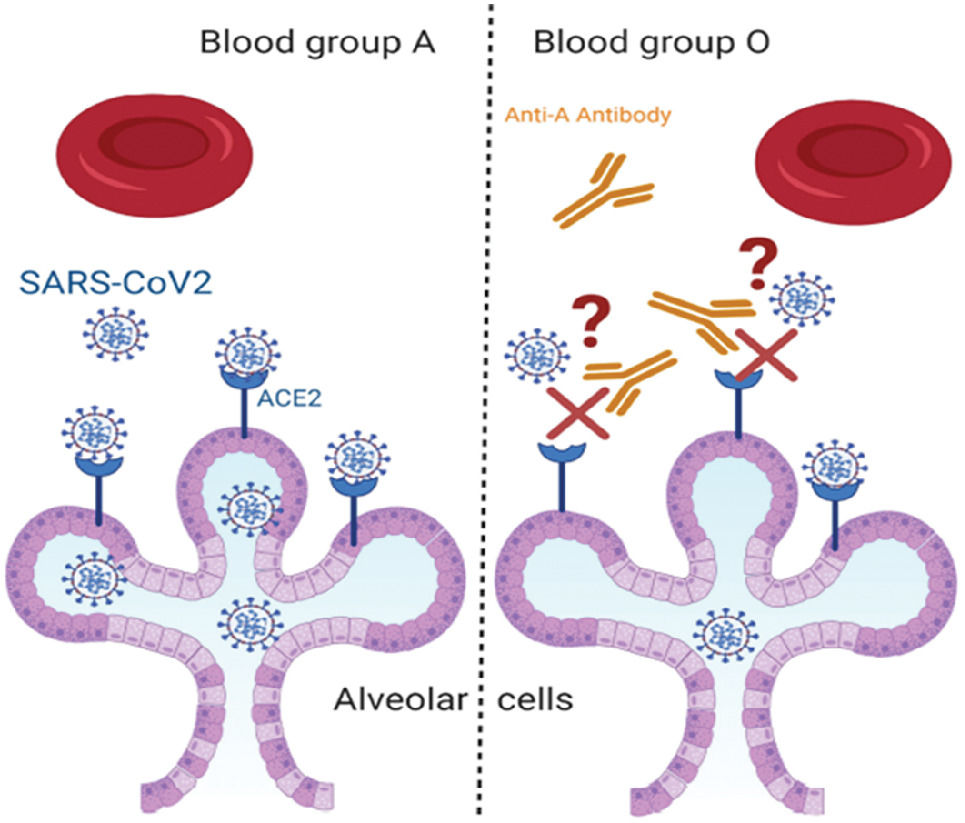
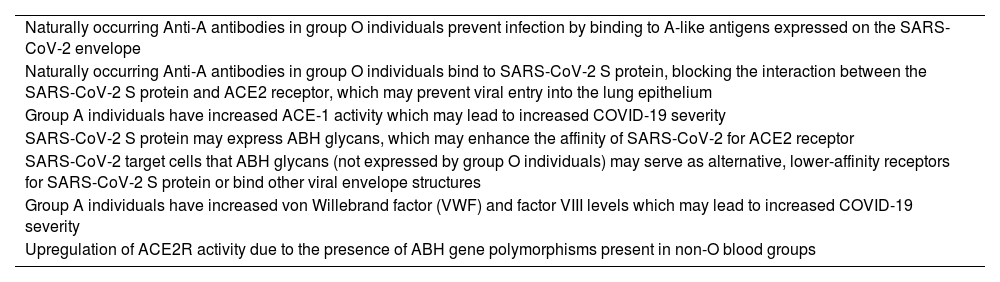
Mechanisms for association between ABO blood groups and COVID-19Several mechanisms have been proposed to explain the association between ABO blood groups and COVID-19 susceptibility and these include the existence of anti-A antibodies, production of glycan antigens by SARS-CoV-2, influence of coagulation system and genetic variations in the ABO gene, as shown in Table 4. Blood groups A and B glycosyltransferases have also been shown to affect glycosylation in various cell types, including epithelial cells in the respiratory tract. The evidence demonstrates that the interaction between the SARS-CoV-2 S protein and its membrane receptor ACE2 could be inhibited by anti-A blood group antibodies that are naturally present in blood groups O and B individuals.15
Summary of proposed mechanisms for association between ABO blood groups and SARS-CoV-2 infection.
Indeed, the presence of anti-A antibodies has been suggested as one of the potential mechanisms that leads to reduced susceptibility of group O individuals to the COVID-19 infection. This hypothesis suggests that anti-A antibodies, which are present in the plasma of blood groups O and B and absent in the A blood group interfere with the SARS-CoV-2 adhesion to host cells, thereby preventing the interaction between the S protein of the virus and the ACE 2 on the cell surface, as shown in Figure 2. A study by Gérard et al. reported that the COVID-19 was less prevalent among blood groups O and B, which have anti-A antibodies, while it was higher in the groups lacking the anti-A antibodies.43 The neutralizing effect of the anti-A antibody has previously been shown to block the binding of the S protein of the SARS-COV to ACE 2 receptors.44 It was further demonstrated that anti-A antibodies from the blood group O were more protective than the antibodies produced by the blood group B, possibly due to the fact that the anti-A present in blood group O are from the IgG class, while those in the blood group B are from the IgM class.43 Furthermore, it is reported that the antibody of the IgM class produces phenotypic glycosylation in none of the O blood groups associated with reduced isoagglutinin activity.45
Another possible mechanism is that the SARS-CoV-2, while replicating in the host epithelium, produces glycan antigens similar to those of the host A or B antigens, according to the blood group of the host.45 When the SARS-CoV-2 exhibits a specific glycan antigen which infects another individual with a different blood group, the corresponding antibodies, if present, will block the interaction between the S protein of the virus and the ACE 2 of the host cells.46 For example, if the SARS-CoV-2 is expressing A antigens, then individuals with blood group B or O will show protection to some extent, as anti-A antibodies will inhibit the virus adhesion to the host cells. On the other hand, individuals with blood group A or AB will face a greater risk of infection, as they lack the anti-A antibodies.
Some factors of the coagulation system have also been proposed to influence the severity of COVID-19 by expressing A and B antigens to increase their concentration and life span. In individuals with blood group A, the factor VIII and VWF express A antigens, leading to the increased susceptibility of group A individuals.47 An additional proposed mechanism, suggesting a potential role of the genetic variation of the ABO blood system in COVID-19 severity. It has been reported that there is an association between the respiratory failure in COVID-19 and the presence of the rs657152 polymorphism, which is a variant that is located at the ABO locus.48 In addition, a study by Luo et al. showed that four ABH gene polymorphisms (rs495828, rs8176740, rs8176746 and rs12683493), which compromise the GATC haplotype, upregulate the activity of ACE 2 receptors.49 Interestingly, the GATC haplotype predominants are non-O blood groups, as the SARS-CoV-2 utilizes the ACE 2 to adhere to host cells.50
Although, a large number of studies reported an associated between ABO blood groups and COVID-19 susceptibility and disease severity, currently there are no specific COVID-19 interventions based on the patient blood groups. These findings have not yet been used as clinical evidnence to deliver personalized medicine to more susceptible individuals. Furthermore, population blood groups have not been used to model viral infection to predict the future course of an outbreak and evaluate strategies to control the spread of infection. This is because the relationship between the blood group, COVID-19 infection, and disease severity is still under debate and not fully understood.
ConclusionThe SARS-CoV-2 is a pandemic affecting human health and economy all around the world. Since the first confirmed case, millions of people have been affected worldwide, with varying clinical manifestations, ranging from asymptomatic infection to death. Many studies have investigated the association between ABO blood groups and COVID-19 suceptibility and severity. Data from theses studies suggest that the ABO blood group could be one of the factors that may play a role in determining COVID-19 susceptibilty, severity and mortality. The data reviewed in this review suggets that blood group O could potentially decrease the susceptibility against the SARS-CoV-2 infection and disease severity. On the other hand, individuals with blood group A have been demonstrated to be at greater risk for the SARS-CoV-2 infection and serious outcomes. However, the studies discussed herein may have been influenced by several confounding factors. These confounding variables include the number of patients included, the types of controls used for comparison and the relative ABO frequencies in the population studied, as these variations in the ABO blood group frequencies between populations of different geographical locations may represent an important source of potential bias. Therefore, further studies are warranted to fully elucidate the ABO assocaition and the exact mechamism/s.
None.