To translate, cross-culturally adapt and validate the Sickle Cell Self-Efficacy Scale for application in the Brazilian cultural context.
MethodsThis is a methodological study performed in 6 steps: 1- Forward translation; 2- Translation synthesis; 3- Back-translation; 4- Assessment by expert committee, with computation of the Content Validity Index (CVI); 5- Cultural adequacy (pre-test); 6- Reproducibility. A pre-test was performed with the participation of 10 adolescents/young adults with sickle cell disease through a telephone call and their responses were recorded on a form in a web platform. The instrument validation step was carried out with 55 adolescents/young adults with sickle cell disease, 43 of them having participated in the retest. The analysis of internal consistency and reproducibility was calculated using the Cronbach's alpha coefficient and the Intraclass Correlation Coefficient (ICC), in the R statistical programming environment.
ResultsThe translated instrument had good acceptance among the experts, reaching an average CVI of 1.0. In assessing reliability, the scale showed acceptable internal consistency, with a Cronbach's alpha of 0.84. In the agreement analysis, the ICC was 0.923 (95% CI: 0.857 to 0.958), which indicates good temporal reproducibility.
ConclusionsFollowing the process of translation, cross-cultural adaptation and validation, we obtained the Brazilian version of the Sickle Cell Self-Efficacy Scale, considered valid and reliable to be applied to adolescents and young adults with sickle cell disease in Brazil.
Sickle cell disease (SCD) is one of the most common genetic and hereditary diseases worldwide. Its mutation originated on the African continent and can be found in populations from all continents due to population migrations, with a high incidence in Africa, Saudi Arabia, and India. In Brazil, due to the large presence of Afro-descendants, SCD represents a group of relevant diseases and conditions.1
In the context of SCD, self-efficacy has been shown to be positively correlated with self-care behavior, whereby individuals perform care activities to better manage a disease or chronic condition.2–4,5 Self-efficacy is defined as the belief in one's personal ability to efficiently perform certain tasks or behaviors to produce a desirable result.6
Designed to measure how adolescents and young adults with SCD perceive their ability to manage their symptoms and to perform daily functional activities, the Sickle Cell Self-efficacy Scale (SCSES) was developed and validated in the United States. It consists of nine questions based on SCD self-care agency, addressing pain and tiredness control, emotion management, need for behavior change, making appropriate decisions about disease care and ability to perform activities of daily living.2,3
Among the instruments that assess self-efficacy in SCD, the SCSES stands out for being effective, brief, practical and quick to administer. It can be administered via telephone calls to a large number of young people, before and after an intervention.3
A group of researchers at the Nursing School, along with researchers at the Laboratory for Experimentation in Translation, Arts College and the Department of Statistics of the Federal University of Minas Gerais (UFMG), have been pursuing studies on the translation, cross-cultural adaptation and validation of healthcare instruments under the auspices of the project “Empower – Methodological innovation in educational practices aimed at enhancing chronic disease self-care”. In order to provide healthcare professionals in Brazil with an instrument to assess self-efficacy in SCD, the researchers decided to adopt the SCSES within educational practices aimed at psychosocial aspects of adolescents and young adults.
The aim of this study was to translate, cross-culturally adapt and validate the SCSES to be administered to adolescents and young adults with SCD in Brazil.
MethodsThis is a methodological study that followed the recommendations established in the scientific literature.7 For analysis of conceptual and item equivalence, concepts related to SCD were explored in order to verify whether the dimensions of the instrument were relevant to the Brazilian cultural context. A broad literature review was performed and meetings were held by members of the Management, Education and Health Assessment Center (NUGEAS - Núcleo de Gestão, Educação e Avaliação em Saúde) of the Nursing School, along with healthcare professionals and applied linguists, to discuss and assess the SCSES.
Upon deciding for the viability and relevance of using the SCSES in Brazil and obtaining the author's permission to translate the instrument, the following steps were taken.
Forward translation was performed independently by two translators, thereby obtaining two versions in Brazilian Portuguese (T1 and T2). The translated versions were then compared and assessed to produce a consensual version (T1-2), which was back-translated by two translators independently, to assess the equivalence between the original version in English and the consensual version (T1-2) in Brazilian Portuguese via its backtranslation into English.7
The version obtained, after successfully confirming equivalence, was submitted to evaluation by an expert committee, made up of five nurses, who were invited to answer an electronic questionnaire on the web tool e-Surv.8 The web questionnaire showed the items in English and their translation in Brazilian Portuguese. To answer each question a star rating was used: 1 star standing for full retranslation required; 2 stars for partial retranslation required with substantial revision; 3 stars for partial retranslation required with minor revision to improve text style, and; 4 stars for no retranslation required. When selecting one, two or three stars, experts were requested to fill in a text box with their suggestions for improvement.
The Content Validity Index (CVI) was computed on the basis of the sum of relative frequencies of answers “3” and “4”, considering that the higher the CVI, the fewer the number of suggestions to retranslate and revise to improve the translation of the instrument9.
The version obtained after the expert evaluation was used in the pre-test, which was administered via a telephone call to a group of ten adolescents/young adults with SCD. Male and female participants were contacted, their age ranging from 16 to 23 years old. All of them were selected based on their capability to understand and respond verbally to the questions in the instrument. For adolescents under the age of 18, their consent and that of their parents and/or legal guardians to participate in the study were requested.
An electronic questionnaire on the e-Surv8 web platform was used to record the respondents’ answers to the instrument. For each item in the translated version of the instrument, there were response options on a 5-point Likert scale with the following levels of agreement10: 1 point - “Not at all sure”; 2 points - “Not sure”; 3 points - “Neither”; 4 points - “Sure”; and 5 points - “Very sure”. The total scores were obtained by summing up the responses for all nine items, with higher scores indicating greater self-efficacy.2,3,5
The administrators used a form to record respondents’ level of understanding of each question with the following options: 1) Respondent showed no difficulty in understanding the item; 2) Respondent showed difficulty in understanding the item; 3) Respondent requested administrator to read the item more than once; and 4) Respondent did not answer the item.
Upon instrument administration, discussions were held by the researchers participating in the project to make adjustments to enhance respondents’ understanding. After that step, the final version of the instrument was obtained.
Validation aimed to assess the internal consistency and temporal reproducibility of the SCSES.
The final version was then administered to adolescents/young adults with SCD on two occasions (test and retest), following the same methodological steps described in the pre-test.10
The selection of adolescents/young adults who took part in this step was performed as convenience sampling from a database of participants in a project entitled “Evaluating a healthcare digital intervention using a mobile app – a randomized clinical study”.11 A total of 55 adolescents/young adults participated in the test, 43 of whom participated in the retest. Female and male participants were selected, aged between 15 and 23, all capable of understanding and responding verbally to the questions in the instrument. The difference in the number of participants from the test to the retest was due to some respondents’ failure to participate in the retest. The average interval between the test and retest was 17 days.
The collected data were coded and anonymously stored in a database created for this purpose and analyzed in the statistical programming environment R.
For assessment of internal consistency, the Cronbach's alpha coefficient was used. In the analysis of temporal reproducibility, Spearman's correlation coefficient between the responses to the items at the time of the test and retest was computed, as well as the ICC (Intraclass Correlation Coefficient), using the instrument's total score. The Wilcoxon test was used to verify the hypothesis that there was no significant difference between the median of the responses obtained in the test and in the retest.12 For all the statistical analyses, the significance level was set at 0.05.
Ethical approval for this study was granted by the Institutional Review Boards of HEMOMINAS Foundation, Belo Horizonte, MG and UFMG, under Certificate No. 3.990.306.
ResultsOf the 15 invitations sent to experts to participate in the committee, five replies were received and questionnaires answered on the web platform e-Surv. This is a number compatible with published studies. All experts reported graduate degrees, proficiency in English, 60% of them stating that they read English texts twice or more times a week. Most participants reported their proficiency in understanding and reading skills to be reasonable (40% and 60%, respectively).
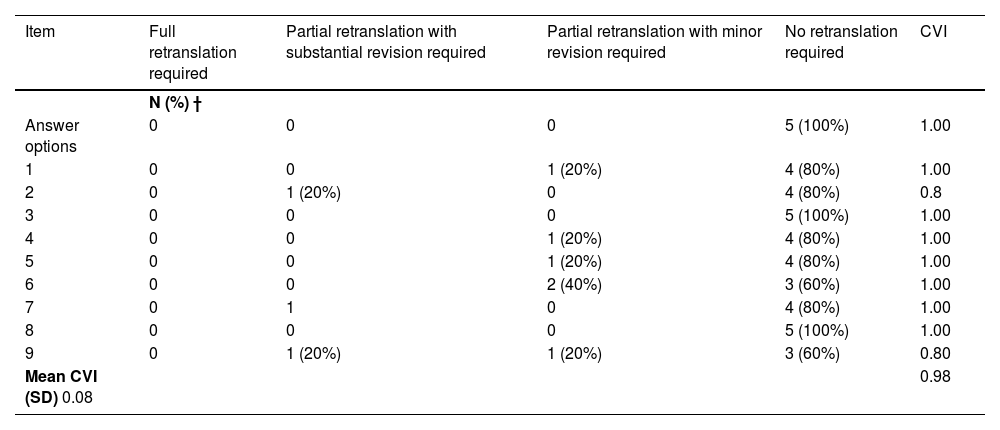
In general, the instrument obtained high CVI values, yielding a mean CVI of 0.98 (standard deviation of 0.08). Questions 2 and 9 had lower CVI values, indicating the need for revision. Despite having CVI equal to 1.0, questions 1, 4, 5 and 6 received suggestions for partial retranslation with minor revision, as shown in Table 1.
Absolute and relative frequency of the expert assessment of the instrument items and Content Validity Index. Belo Horizonte, MG, Brazil, 2020.
CVI – content validity index; †The relative frequencies add up to 100% within the lines and the absolute frequencies correspond to the number of experts for each group of instrument statements. All experts evaluated the instrument's instructions and answer options.
The experts agreed on the translation of a WH question (“how sure?”) by a Yes or No question in Portuguese (“você acha?” [do you think?]) followed by the 5-point Likert scale for level of certainty, since the WH question “quão certo” (“how sure?”) is not frequently used in colloquial Portuguese. All suggestions made by the experts were thoroughly discussed until no further revision was felt to be necessary and a satisfactory version was obtained. For questions 3 and 8, there was no need for retranslation or revision suggested by the experts. For questions 1, 3, 4, 5 and 7, word order was suggested. However, upon discussing that suggestion, the NUGEAS expert group decided not to introduce shifts in word order as the original and the translated versions had reached semantic, idiomatic and conceptual equivalence.
The committee's comments considered relevant to cross-cultural adaptation in items 2, 6 and 9 are briefly described below:
- •
Item 2 “How sure are you that you can keep doing most of the things you do day-to-day?” was initially translated as “Você acha que consegue seguir fazendo a maior parte das suas atividades normais do dia a dia?” [Do you think you can manage to keep doing most of your everyday activities?]. However, the expert committee suggested replacing “seguir fazendo” [keep dpoing] by “realizar” [to do]; therefore, the final version was “Você acha que consegue realizar a maior parte das suas atividades normais do dia a dia?” [Do you think you can manage to do most of your everyday activities?].
- •
Item 6 “How sure are you that you can do something to help yourself feel better if you are feeling sad or blue?” was initially translated as “Você acha que consegue ajudar a você mesmo quando está triste ou infeliz?” [Do you think you can manage to help yourself when you are sad or unhappy?]. The expert committee suggested including “sentir-se melhor” [feel better], the final version being “Você acha que consegue ajudar a você mesmo a sentir-se melhor quando está triste ou infeliz?” [“Do you think you can manage to help yourself feel better when you are sad or unhappy?]
- •
Item 9, “How sure are you that you can deal with the frustration of having sickle cell disease?”, was initially translated as “Você acha que lida bem com a frustração de ter doença falciforme?”[do you think you can deal with the frustration of having sickle cell disease?]. The committee remarked that even if the word “frustration” is in the original in English, saying “with the frustration” implies that there is such feeling, which may not always be the case. The committee thus suggested “Você acha que lida bem com a condição de ter doença falciforme?” [Do you think you can deal adequately with the condition of having sickle cell disease?].
With regard to the answer options, all participants considered them adequate and made no suggestions for revision.
The adapted version was then applied in the pre-test to a sample of ten adolescents/young adults with SCD.
During the pre-test, notes were taken by the interviewer, which allowed some adjustments to improve interaction with participants and make sure they understood the questions in the scale: (1) before starting the questions, participants were explicitly informed that the answers would be based on their knowledge and experience regarding SCD, and; (2) to facilitate the scale administration via telephone call, participants were advised to write down the answer options on paper. If they decided not to do that, the answer options were repeated every time each question was asked during the call.
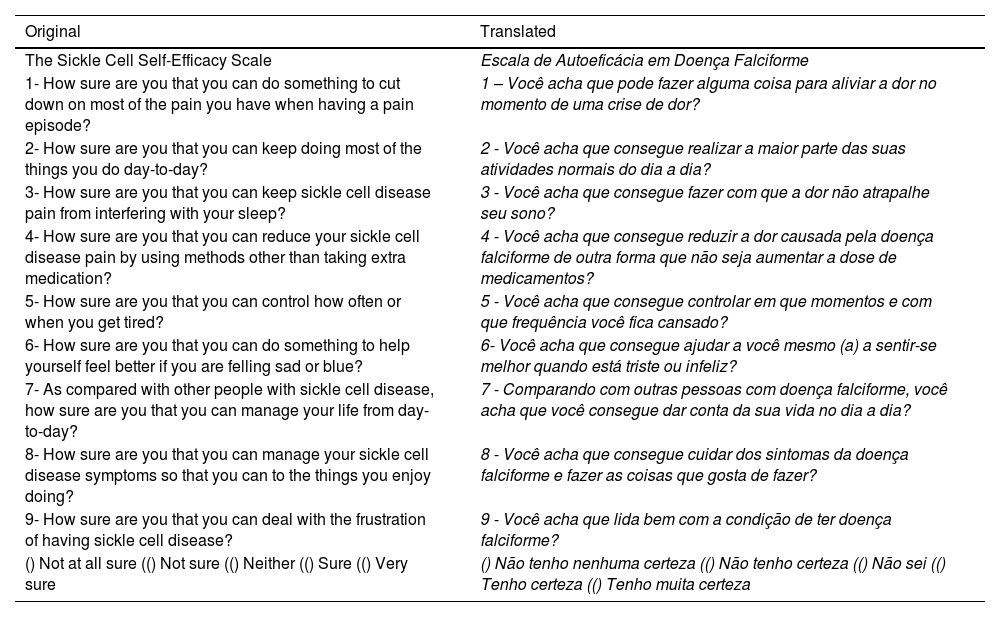
Upon concluding the pre-test, the final version of the SCSES - Brazilian version was obtained, as shown in Chart 1.
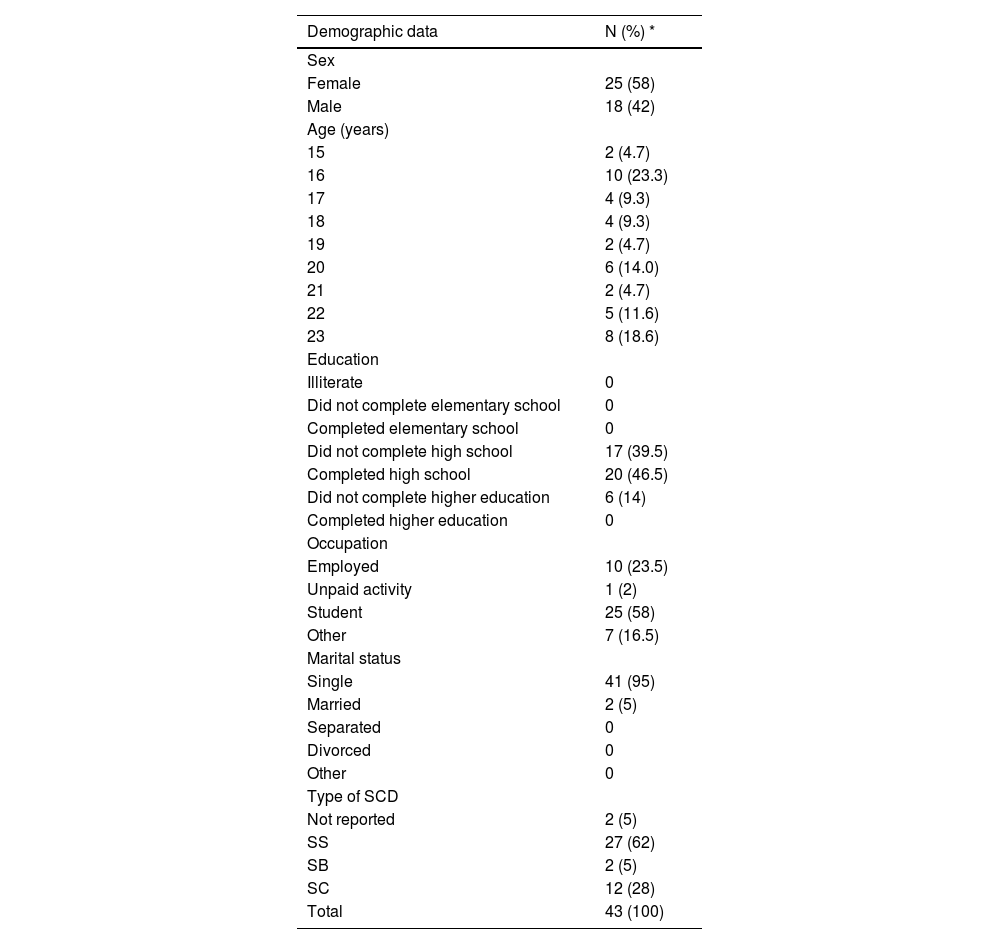
Table 2 shows the demographic data of adolescents/young adults who participated in the test and retest.
Demographic data of adolescents/young adults participating in the SCSES validation. Brazil, 2020.
| Demographic data | N (%) * |
|---|---|
| Sex | |
| Female | 25 (58) |
| Male | 18 (42) |
| Age (years) | |
| 15 | 2 (4.7) |
| 16 | 10 (23.3) |
| 17 | 4 (9.3) |
| 18 | 4 (9.3) |
| 19 | 2 (4.7) |
| 20 | 6 (14.0) |
| 21 | 2 (4.7) |
| 22 | 5 (11.6) |
| 23 | 8 (18.6) |
| Education | |
| Illiterate | 0 |
| Did not complete elementary school | 0 |
| Completed elementary school | 0 |
| Did not complete high school | 17 (39.5) |
| Completed high school | 20 (46.5) |
| Did not complete higher education | 6 (14) |
| Completed higher education | 0 |
| Occupation | |
| Employed | 10 (23.5) |
| Unpaid activity | 1 (2) |
| Student | 25 (58) |
| Other | 7 (16.5) |
| Marital status | |
| Single | 41 (95) |
| Married | 2 (5) |
| Separated | 0 |
| Divorced | 0 |
| Other | 0 |
| Type of SCD | |
| Not reported | 2 (5) |
| SS | 27 (62) |
| SB | 2 (5) |
| SC | 12 (28) |
| Total | 43 (100) |
The average age of adolescents/young adults was 15 to 23 years (M = 19.2 years; SD = 2.8 years). Regarding the type of SCD, 62% had SS type and 5% were unable to report which type they had.
A total of 58% were female; 46.5% had completed high school; 58% were students and 23.5% were regularly employed.
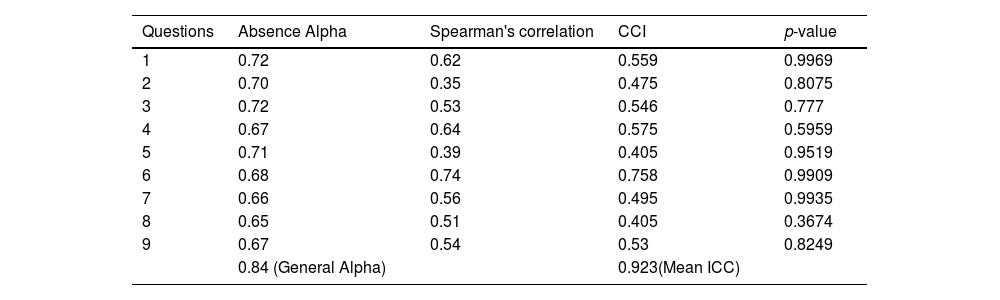
Table 3 presents the results of the internal consistency assessment (alpha of absence of each item and general Cronbach's alpha), Spearman's correlation for each item (test-retest), the ICC value between the total score of the test and retest and the p-value of the test for equality between the scores of the test and retest. The SCSES - Brazilian version had an overall value of Cronbach's alpha = 0.84 and its internal consistency was considered acceptable.
Internal consistency assessment (alpha of absence of each item and general Cronbach's alpha), Spearman's correlation, ICC and the p-value of the test for no difference between the scores of the test and retest the Sickle Cell Self-Efficacy Scale – Brazilian version. Brazil, 2020.
Items in the original version of the Sickle Cell Self-Efficacy Scale and their Brazilian version. Brazil, 2020.
To obtain Spearman's correlation coefficient, the answers obtained in the test and retest showed moderate correlation for questions 1, 3, 4, 7, 8 and 9, weak correlation for questions 2 and 5 and strong correlation only for question 6.
Analysis of the instrument reliability was supported by the calculation of ICC. The ICC average obtained in the test and retest was 0.923 (95% CI: 0.857 - 0.958). The above result indicates excellent agreement (ICC > 0.90) between the mean of the responses obtained in the test and in the retest.
For all items, we obtained a p-value higher than the significance level in the Wilcoxon test, which implies that there is no statistical evidence that the scores of the test and retest have different distributions (Table 3). Therefore, we can conclude that the Brazilian version of SCSES has temporal stability.
DiscussionThis study aimed to translate, cross-culturally adapt and validate the SCSES to be used in Brazil. Each step followed methodological recommendations described in the literature.7,13,14
The scores obtained by using this scale may represent an indicator of evaluation of educational practices aimed at adolescents and young adults with SCD. This assumption and the lack of valid and specific instruments to measure self-efficacy in SCD motivated the decision to translate, cross-culturally adapt and validate it.3,5,15,16
In the literature, studies were found in other languages that used instruments to assess self-efficacy in SCD; however, the SCSES - Brazilian version stands out for the ease and feasibility of application via telephone calls.3,15,17
There are several advantages in adapting instruments already validated in other languages, instead of elaborating them from scratch. Using validated questionnaires can elicit comparable data; they save time, financial and human resources and they facilitate the exchange of information and dissemination of knowledge among the scientific community.7,14,9
Studies that validated the SCSES used a methodology similar to that presented in our study, following international recommendations, presenting psychometric qualities and robust results.3,13,16,17,14,9,18
Regarding the instrument adaptation, the evaluation performed by the expert committee made it possible to ensure semantic, idiomatic, cultural and conceptual equivalence between the translated version and the original instrument.9 Assessment by experts was conducted through a web questionnaire, enabling fast access, economy of resources and systematization in data treatment.19
The relevance of the role of an expert committee lies in negotiating perspectives from different disciplinary fields, reviewing translations, making critical decisions, seeking consensus on any discrepancy and consolidating all versions of the instrument.7
The Brazilian version presented good acceptance among judges, indicating conformity of the translated version with the original version of the instrument. The CVI values of each item and suggestions made by the evaluators guided our analysis and directed us to focus on the issues that needed improvement in terms and expressions to ensure semantic, idiomatic and conceptual equivalence.20
An instrument needs to be able to measure what it intends to measure and present psychometric characteristics that demonstrate reliability and validity. Hence, the importance of following recommended methodological strategies, avoiding dubious research results and erroneous conclusions.7,20,21
Before starting the procedures to verify the internal consistency and temporal stability of the SCSES - Brazilian version, the pre-test was performed in order to ensure full understanding of items and response options. Decisions regarding instrument administration facilitated the participants’ understanding.
In a study conducted in Saudi Arabia with the SCSES, a Likert-type scale with 3 response options was used.16 However, in our study, we chose to maintain the five categories of responses to make the results of the instrument comparable to the original study.3,17
In the applicability of this scale, the test and retest had the participation of adolescents and young adults of both sexes, with ages distributed between 15 and 23 and different levels of education and occupations (students and employed people). The predominant type of SCD in the sample was HbSS. This profile is similar to that of participants in other studies that evaluated self-efficacy in SCD using the same instrument.3,18
As for interval time between the test and retest, there was an attempt to follow the recommended period in the literature, but we had an average interval of 17 days (SD = 3.0) due to participants’ schedules and the need to reschedule calls on various occasions.13,12,22
A Cronbach's alpha value of 0.84 was obtained in the internal consistency analysis. This value is within the values considered acceptable in the literature.23 This result corroborates studies that validated the original version of the instrument and presented the Cronbach's alpha values of 0.80 and 0.89, respectively.3,17,18
In the reliability analysis through stability, the ICC of 0.923 (95% CI: 0.857 - 0.958) was obtained for the scale as a whole, which demonstrates temporal stability.12
Data on internal consistency and reliability determined homogeneity and temporal stability.24 Multiple applications of the instrument in the Brazilian context may generate similar and accurate results.25
The validation process made it possible to confirm the successful use of a web platform, which proved to be a reliable and safe methodology. The use of this tool allowed the participation of professionals in the expert committee and facilitated the recording of the answers obtained in the test and retest. The tool provided the organization with information in a spreadsheet generated automatically for later import of data for analysis in a statistical programming environment, as well as avoiding data transcription and saving time and human resources.19
The SCSES - Brazilian version is a specific instrument for SCD, already validated in other countries, such as the United States and Saudi Arabia. It is used to measure the perception of adolescents and young adults with SCD of their ability to manage their symptoms and perform activities of daily living. Its applicability in studies showed that people with SCD who had lower levels of self-efficacy had more symptoms, such as pain crises, hospitalizations and sought more medical care, when compared with individuals who reported higher levels of this variable.2,3,18,26
A limitation of this study is the need for further studies that reinforce evidence of validity and reliability of the SCSES - Brazilian version, using other representative samples, composed of different regional groups. This can be overcome through a continuous evaluation process of the instrument, aiming at its improvement for use in the Brazilian cultural context.
It is expected that further studies be conducted in the future to evaluate self-efficacy scores in adolescents and young adults with SCD and educational practices be implemented for this group.
ConclusionThe SCSES - Brazilian version was considered valid and reliable to be administered to adolescents and young adults with SCD.
This study was funded by the Brazilian National Council for Scientific and Technological Development (CNPq - Conselho Nacional de Desenvolvimento Científico e Tecnológico), Grant 303250/2019-4.
The authors are grateful for the support of the Foundation of Hematology and Hemotherapy of Minas Gerais / HEMOMINAS.