Multiple myeloma is a progressive and incurable cell neoplasm characterized by deregulated and clonal proliferation of plasma cells in the bone marrow. These cells produce and secrete monoclonal immunoglobulin or a fragment of the same, called Protein M.1 Pathophysiological consequences of the disease's progression include bone destruction, renal failure, suppression of hematopoiesis, increased risk of infection and splenic rupture.2 The increased incidence of multiple myeloma in recent years is related to a better understanding of its natural history and pathogenesis, improved laboratory resources, increased life expectancy worldwide and chronic exposure to pollutants.2
A rare pathophysiological consequence of the disease progression is pathological splenic rupture, a non-traumatic rupture occurring in a diseased spleen. Splenic rupture due to multiple myeloma is rare, with only three cases having been reported in the literature.3 Some of the pathogenic factors leading to splenic rupture in patients affected by the disease include infiltration of the spleen, splenic infarction and blood coagulation defects.
We now report a case of splenic rupture secondary to myeloma, a very rare complication of a not uncommon hematologic neoplasia.
Case reportA 44-year-old previously healthy male presented with complaints of abdominal pain for the last two days. Physical examination revealed a slightly pale complexion, pain on gentle palpation, and a blood pressure of 100/70mmHg. The hemogram showed erythropenia (3.29million/mm3) and reduced levels of hemoglobin (9.1g/dL) and hematocrit (29.0%). Serum levels of creatinine (1.5mg/dL), urea (120.0mg/dL), and potassium (5.7nmol/L) were elevated, as were the C-reactive protein (389.4mg/dL) and international normalized ratio (INR) (1.65).
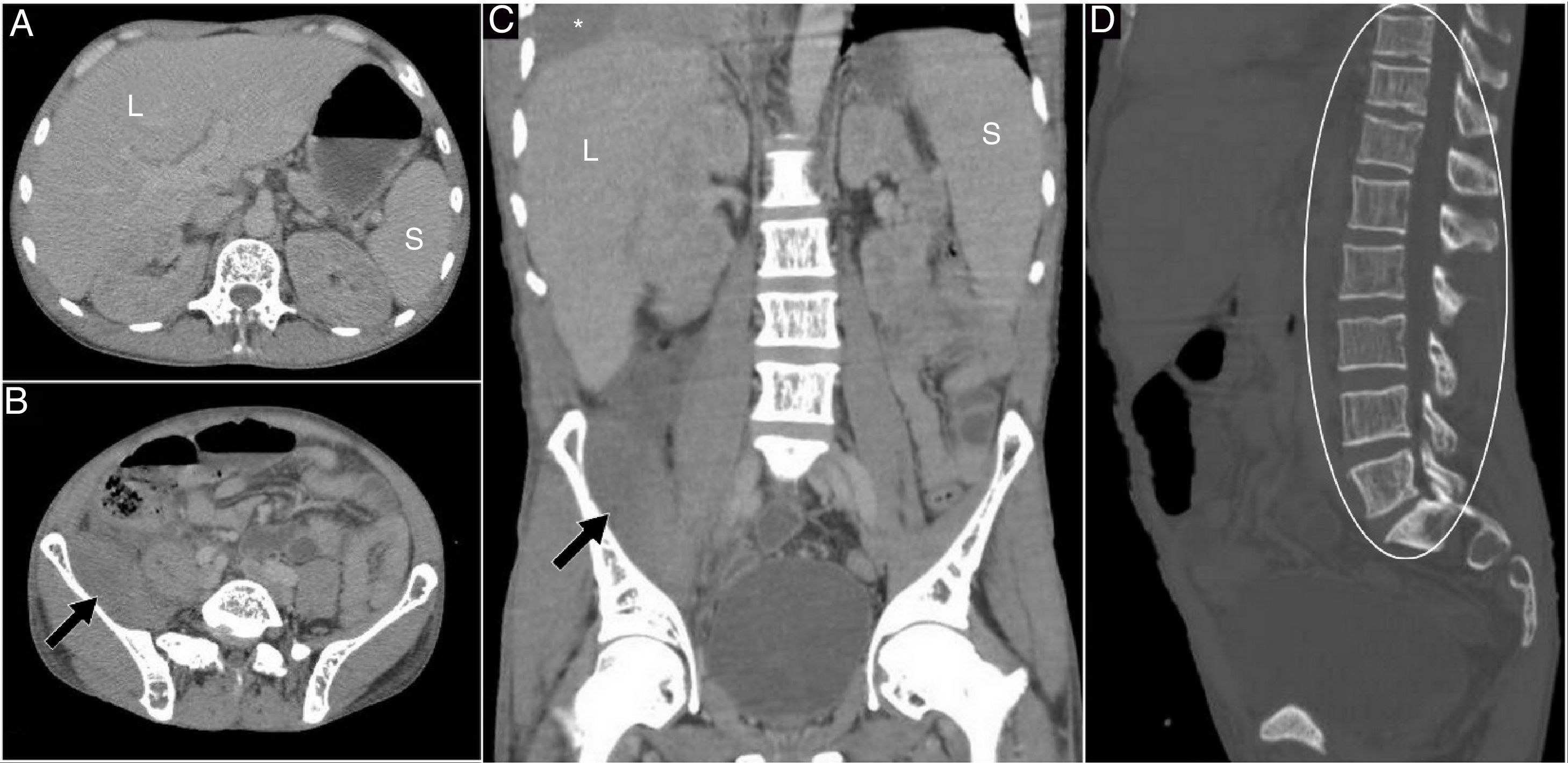
Abdominal computed tomography (CT) scanning with an intravenous contrast medium showed a normal-appearing liver and spleen (Figure 1A), retroperitoneal fluid collection near the iliopsoas muscle in the right iliac fossa (Figure 1B and C), a minimal amount of intra-abdominal free fluid, and diffuse changes in trabeculation and bone marrow density throughout the skeleton (Figure 1D), as well as a mild to moderate pleural effusion at the base of the right hemithorax (Figure 1C).
(A–D) Portal phase abdominal CT with intravenous contrast medium showing the liver (L) and spleen (S) without perceptible abnormalities, retroperitoneal collection near the iliopsoas muscle in the fossa (black arrow), diffuse changes in trabeculation and bone marrow density throughout the skeleton (white circle), as well as a mild to moderate pleural effusion at the base of the right hemithorax (*).
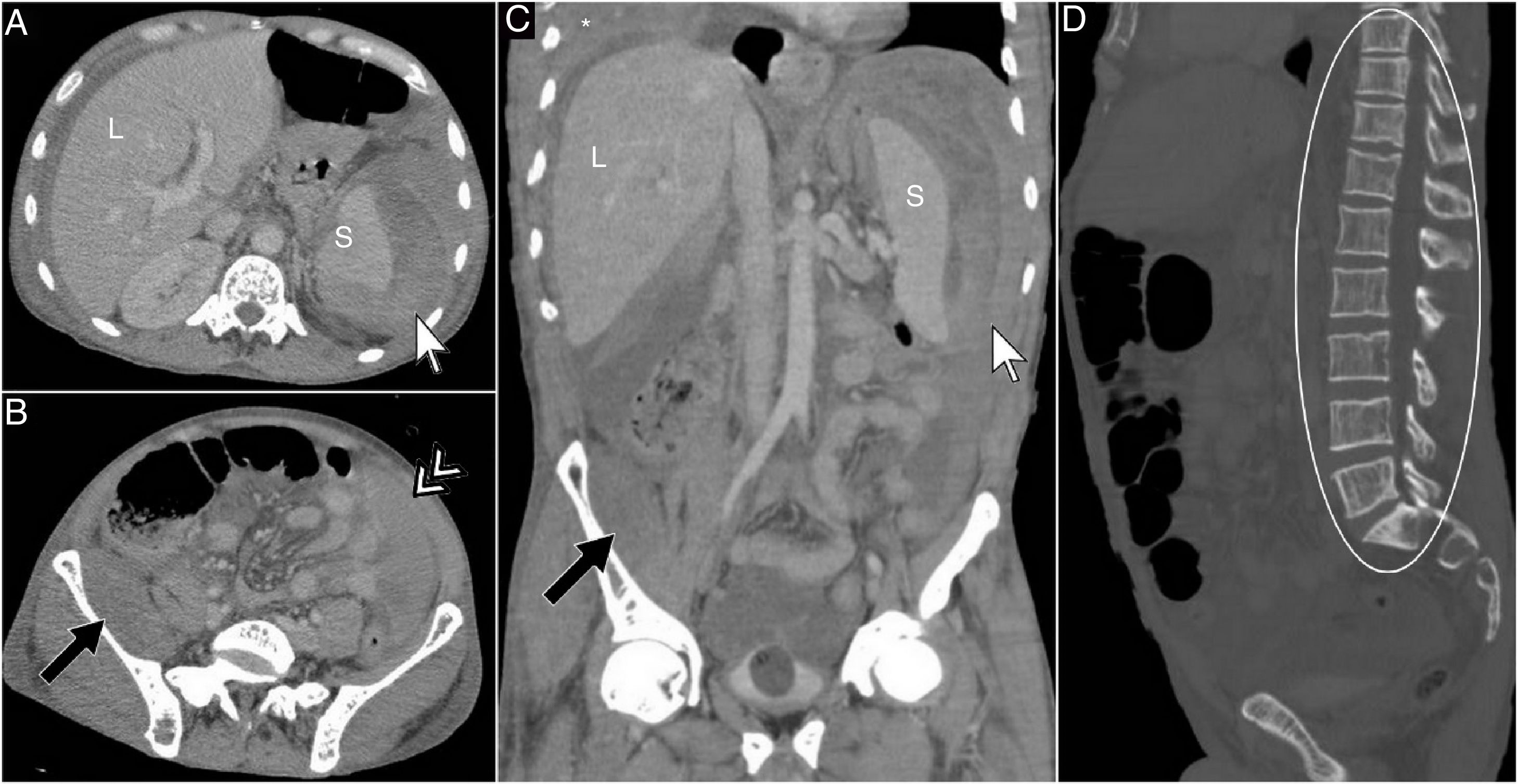
After the patient's condition deteriorated, a new hemogram showed more severe erythropenia, with reduced erythrocyte levels (1.75million/mm3), hemoglobin (5.2g/dL), hematocrit (16.2%), and the urine was negative for the Bence Jones protein. In a new abdominal CT scan, a laceration of the spleen became apparent, as well as a subcapsular collection of hematic fluid (Figure 2A), a hemoperitoneum to the left side (Figure 2B), continued retroperitoneal fluid collection (Figure 2B and C) and right pleural effusion (Figure 2C), an increased amount of intra-abdominal free fluid, and similar bone findings (Figure 2D).
(A–D) Portal phase abdominal CT with intravenous contrast medium showing an apparent laceration in the spleen with a hyperdense subcapsular collection of hematic fluid (white arrow), a large hemoperitoneum on the left side (double headed white arrow), continued retroperitoneal collection in the right iliac fossa (black arrow) and a mild to moderate pleural effusion on the right side (*), as well as the previously described bone alterations (white circle).
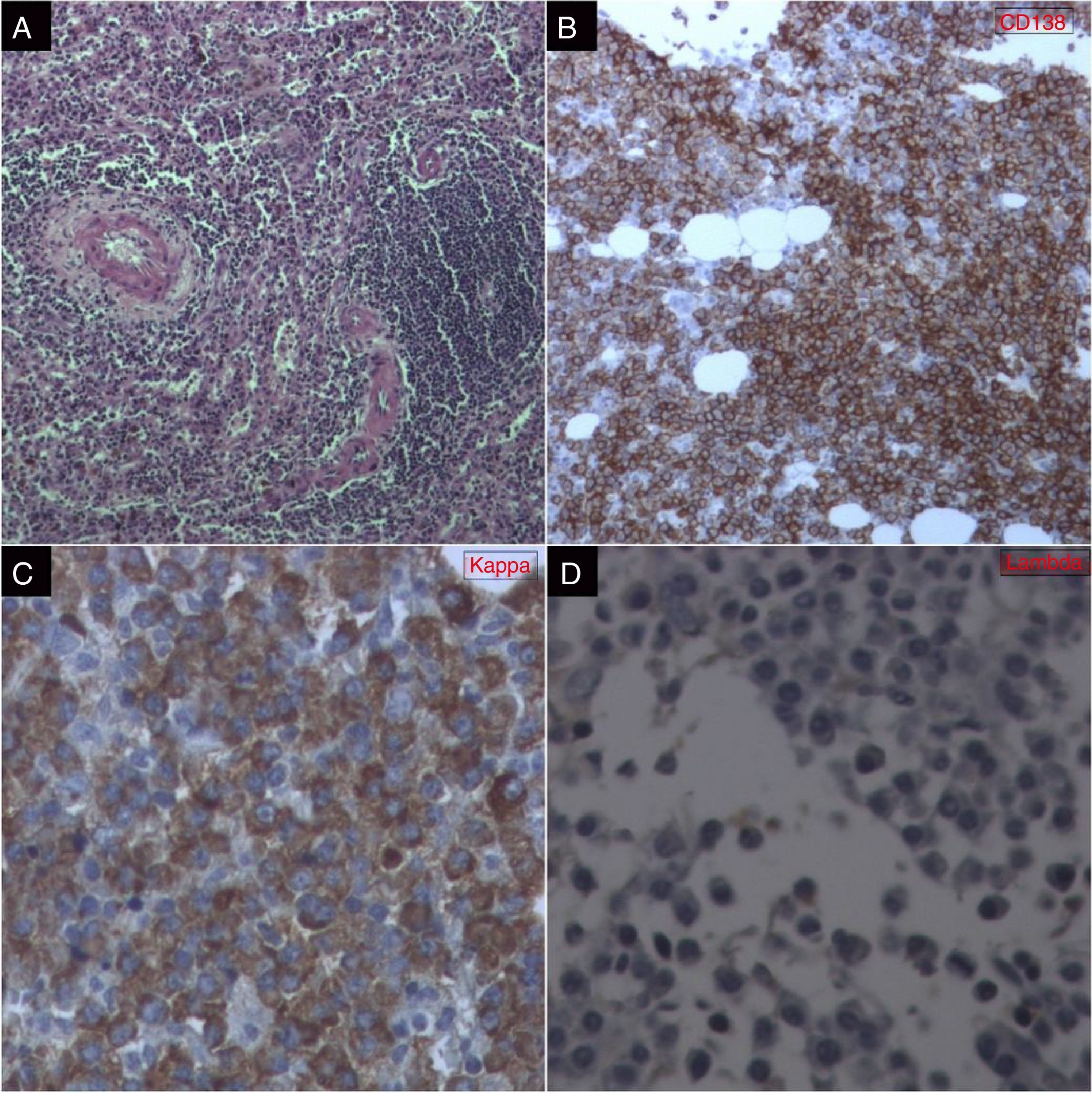
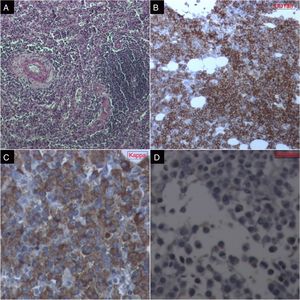
Serological tests and laboratory analysis for HIV, HCV, HBV, Epstein–Barr virus, and cytomegalovirus, as well as blood cultures, were negative. A splenectomy was performed, and the clinicopathological study revealed a splenomegaly, with signs of hypersplenism with acute peripheral infarction, rupture of the capsule and lymphoproliferative disease with an expansion of the red pulp. Complementary biopsy and histology of the medulla and the resected spleen (Figure 3A) indicated lymphoproliferative disease with plasma-like cells. Immunohistochemistry (Figure 3B–D) showed infiltrative neoplasia with plasmacytic differentiation, as well as the following results: CD3 (MRQ-39), CD20 (L26), Lambda; CD5 (4C7), Cyclin D1 (EP12); CD10 (56C6) and CD138 (B-A38) with 60% cellularity and Kappa (polyclonal) were positive; Myeloperoxidase (polyclonal)=myeloid cellularity (30%); and Glycophorin A (GA-R2)=erythroid cellularity (10%). Protein electrophoresis showed an elevation in the gamma globulin (2.91g/dL) and beta 2 microglobulin (5490ng/mL).
(A) Spleen: HE-stained slide showing increased white pulp volume at the expense of marginal zone lymphoid cells and red pulp with increased macrophages. (B) Bone marrow: immunohistochemical study with CD138 presenting a neoplastic population of small lymphoid cells with plasmacytic differentiation. (C) Bone marrow: Kappa chain immunoglobulin expression in most bone marrow cells. (D) Bone marrow: lack of lambda chain immunoglobulin expression in neoplastic cells.
The patient presented clinical and laboratory improvement after surgery and was later referred to another unit for neoplasia treatment.
Diagnosis: Retroperitoneal hemorrhage and splenic rupture related to multiple myeloma.
DiscussionThe etiology of a spontaneous splenic rupture can vary from infection (30%) to hematological disorders (27%), tumors (11%), digestive diseases (10%), rheumatic disorders (4%) and other causes (15%).1 The occurrence of spontaneous splenic hematoma in patients using pegfilgrastim is also common, a factor that increases the neutrophil count in patients on chemotherapy.4 The existence of extramedullary hematopoiesis in the spleen may result in splenomegaly, a tendency to rupture and hematomas.5
Splenic rupture due to multiple myeloma is a rare phenomenon, with only three cases having been reported in the literature.2 There has been only one case of spontaneous splenic rupture associated with uncomplicated myeloma, which was attributed to the effects of pressure from multiple plasmacytomas on the splenic capsule, although this has not been definitively established.6
Clinical findings that should be considered typically include pain in the upper left quadrant, recurrent fever and an intra-abdominal mass.
The clinical picture of multiple myeloma may be insidious or asymptomatic. Its clinical manifestations arise due to the infiltration of neoplastic plasma cells in organs, the production of excess immunoglobulin and the suppression of normal humoral immunity. As a consequence, severe anemia, bone damage, renal failure and recurrent infection can occur.6,7
In cases of splenic rupture, the radiographic signs are: elevation of the left diaphragmatic dome, clouding of the left hypochondrium, gastric dilatation and a serrated aspect of the greater curvature of the stomach, lowered splenic angle, increased distance between the colon and the abdominal wall and separation from the abdominal wall.
The tomographic results included structural alterations in bone trabeculation, cortical erosions, lithic areas and a periosteal reaction.7 Due to its poor prognosis, early diagnosis is essential to avoid a possible splenic rupture, since in all previously-described cases the diagnosis has been late, requiring urgent surgical intervention due to hemodynamic instability.8
Splenic rupture in association with multiple myeloma has been reported in the literature only three times and is a very rare complication of a not uncommon hematologic malignancy. It has been hypothesized that forms of multiple myeloma may occasionally behave aggressively, resembling plasma cell leukemias and resulting in splenomegaly and extramedullary hematopoiesis.2,9
ConclusionSplenic rupture secondary to multiple myeloma is a rare phenomenon whose prognosis is worse than other pathophysiological consequences of multiple myeloma. Thus, it is essential to expedite diagnosis to avoid a possible splenic rupture, since in all previously-described cases the diagnosis has been late, after the onset of hemodynamic instability.
Conflicts of interestThe authors declare no conflicts of interest.