Hematologists deal every day with high mortality rates of acute leukemia patients. Many times these patients need Intensive Care Unit (ICU) support and some general ICU teams believe that these patients have a much greater chance of dying than patients with other pathologies. In Brazil, data related to mortality rates and ICUs for acute leukemia patients are scarce.
MethodsTherefore, to assess mortality predictors in patients with acute leukemia admitted to a specialized hematological ICU, we evaluated demographics, supportive care, hospitalization time, disease status, admitting diagnosis, neutropenia, number of transfusions and Acute Physiology and Chronic Health Evaluation (APACHE)/Sepsis Related Organ Failure Assessment (SOFA) scores as possible factors associated with mortality. Data were extracted from the first admission records of 110 patients with acute leukemia admitted to the Hemocentro de Pernambuco (Hemope) ICU between 2006 and 2009.
ResultsIn this retrospective cohort study, 72/110 of the patients were men, and 64/110 were from the metropolitan area of Recife. The patients’ age median was 43.5 years (±17.9); 67.3% had acute myeloid leukemia (AML) and 32.7% had acute lymphoid leukemia. The main admitting diagnosis in the ICU was sepsis (66.7%). The mean APACHE II score was 18.3. Of the total, 65 (59%) died, and the mortality rate was independently related to longer hospitalization (p<0.001), the increase in the APACHE II score (p<0.038) and having received hemodialysis (p<0.006). Neutropenia, receiving multiple transfusions and using any kind of mechanical ventilation or vasoactive drug on admission were not relevant to mortality. Factors associated with higher mortality rates were: longer hospitalization, increase in the APACHE II score, and use of hemodialysis.
ConclusionWith these data, to prevent organ lesions before admission to the ICU, a better strategy might be to reduce mortality for leukemia patients.
Acute leukemias are disorders of hematopoietic stem cells, characterized by fast and uncontrolled proliferation of immature cells (blasts) in the bone marrow.1 These very aggressive disorders suppress the production and normal function of bone marrow cells, causing immunosuppression. It requires urgent treatment, and the complete remission rate is high, approximately 60–75% for acute myeloid leukemia (AML).2
Apart from the bone marrow suppression promoted by leukemia, the use of chemotherapy (CT) drugs raises immunosuppression, resulting in frequent infectious complications, which in turn lead to organ dysfunction. Patients are often septic, with acute lung injury/acute respiratory distress syndrome (ALI/ARDS) and acute kidney failure (AKF). These conditions lead patients to require hospitalization in intensive care units (ICUs).2,3
The effervescence of successful anticancer therapies is linked to the better management of critically ill patients, which clamors for the rethinking of the role of intensive care, regarding indications, benefits and prognostic factors related to neoplasm patients in critical conditions. In the early 1990s, cancer survivors maintained a good quality of life and had no limitations to daily activities after admission to intensive care.4 Despite high rates of mortality (45–87%), studies within this population of critically ill patients showed that intensive care was beneficial.5–13 Thereafter, predictors of mortality among patients with cancer in the ICU started to be repeatedly evaluated.3,6,13–17
Currently, although there are many analyses on predictors of mortality among cancer patients in the ICU, reports of units specialized in exclusively treating patients with blood disease are insufficient.18
Thus, the aim of this study is to assess mortality risk factors among patients with acute leukemia admitted to a specialized hematological ICU.
Materials and methodsPatients and methodsThis is a retrospective cohort study. All patients with acute leukemia over 16 years of age on their first admission to the ICU of the Hemocentro of Pernambuco (Hemope) Foundation Hospital between January 2006 and December 2009 had their medical records retrospectively evaluated in this study. During this period, there were 426 admissions, 137 with acute leukemia, and 110 patients met the inclusion criteria. This ICU is specialized in patients with blood disease. It is part of the Hemope Foundation Hospital, where there is a ward with 36 beds for treating acute leukemia (32), hemophilia (2) and sickle cell disease (2). This is a center of excellence in Pernambuco and neighboring states. The Research Ethics Committee approved this project under the CAEE number 11810213.5.0000.5195 2013.
The diagnosis of acute leukemia was established according to criteria of the World Health Organization (WHO), revised in 2008. The disease status was categorized as: aplasia, remission, progression or relapse. Aplasia was defined as the moment after CT when the hemoglobin (Hb) is lower than 10g/dl, associated leukocyte count is lower than 1000cells/mm3 and platelets are lower than 100,000cells/mm3. Remission was defined as the status after CT when the patient has no active disease (<5% blasts in the bone marrow). Progression was defined as failure of therapy any time before admission or with refractory disease. Relapse was classified as a return of disease activity after a period of improvement (remission). Reasons for admission were those mentioned in the medical records and were categorized as respiratory failure of septic and nonseptic origins, acute renal failure (ARF), sepsis, sensory alterations, post-operative bleeding and shock.
The Acute Physiology and Chronic Health Evaluation (APACHE II) score was applied as a predictive mortality index within the first 24h after admission. It is a severity classification system based upon 12 initial routine physiologic measurements (temperature, heart rate, mean arterial pressure, serum sodium, serum potassium, serum creatinine, oxygenation, hematocrit, blood cell count, Glasgow coma score), age and previous health status. An increasing score is closely related to subsequent in-hospital death.17 To assess progression of organ failure, the Sepsis Related Organ Failure Assessment (SOFA) score was evaluated on days 1 and 3. This score has a descriptive function and individualizes the dysfunction of each organ daily.19 The two scores are complementary and both of them were retrospectively calculated for this paper at http://www.globlarph.com/APACHEII.html and http://www.sfar.org/scores2/sofa2.html, respectively.17,19
Supportive care was categorized as the use of invasive or non-invasive mechanical ventilation (IMV/NIMV), vasoactive drugs (VAD) on admission, renal replacement therapy (RRT) and transfusion support. The IMV was defined as the use of an orotracheal tube at any time during the ICU stay, and the NIMV was considered every time that mechanical ventilatory support was necessary but an orotracheal tube was not; VAD was considered when the use of noradrenalin or dopamine was necessary, and; the use of any kind of hemodialysis, at least once and for any duration, defined RRT.
Statistical analysisCore demographics, comorbidities, disease characteristics and factors associated with mortality in the ICU were evaluated using the STATA statistical software version 13.0 (StataCorp LP, College Station, TX, USA).
Results were presented in the frequency tables for qualitative variables. Descriptive statistics (mean, standard deviation, median and range) were used for continuous quantitative variables, according to the outcome in the ICU (death or survival). The outcome results were compared by nonparametric Mann–Whitney U tests.
For quantitative variables, measurements of central tendency and dispersion were made. In this study, considering the high mortality rate in that ICU (59%) on bivariate analysis, the prevalence rate (PR) and their 95% CIs were estimated to evaluate the correlation between the variables and death in the unit.20,21 Variables independently associated with the mortality rate were analyzed with a multiple Cox regression (with robust variance) using variables that had p-values lower than 0.20 in univariate analysis. A chi-square test for linear trend was used for complete blood count (CBC) variables. Regarding non-quantitative variables, a nonparametric Mann–Whitney U test was used for comparison between patients who died and those who did not.
The modeling process started with the variable that had the lowest p-value during bivariate analysis, followed by the addition of all the others with p-values lower than 0.20, with just the variables with descriptive levels lower than 0.05 (p<0.05) remaining for the final model. Finally, PRs were estimated for each variable in the final model with their respective confidence intervals.
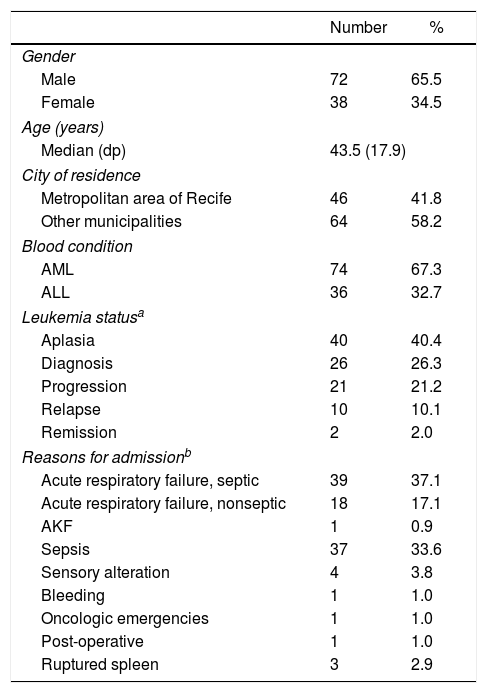
ResultsSixty-five patients died during ICU hospitalization, totalling a 59.1% mortality rate. Table 1 shows demographic and clinical characteristics of the studied population, while Table 2 has hemogram data. Seventy-four out of 110 patients (67.3%) had AML, with French-American-British (FAB) subtypes classified as AML-M3 (n=17, 23.0%), AML-M1 (n=16, 21.6%) and AML-M2 (n=15, 20.3%). The others (36/110) had acute lymphoid leukemia (ALL), 58.3% cases of B-cell (21/115) and 30.6% of the T-cell lineage (11/115).
Characterization of patients with acute leukemia hospitalized in the ICU, according to social and demographic features, base pathology, reasons for admission, severity profile and organ dysfunction at the Hemope Foundation from 2006 to 2009.
| Number | % | |
|---|---|---|
| Gender | ||
| Male | 72 | 65.5 |
| Female | 38 | 34.5 |
| Age (years) | ||
| Median (dp) | 43.5 (17.9) | |
| City of residence | ||
| Metropolitan area of Recife | 46 | 41.8 |
| Other municipalities | 64 | 58.2 |
| Blood condition | ||
| AML | 74 | 67.3 |
| ALL | 36 | 32.7 |
| Leukemia statusa | ||
| Aplasia | 40 | 40.4 |
| Diagnosis | 26 | 26.3 |
| Progression | 21 | 21.2 |
| Relapse | 10 | 10.1 |
| Remission | 2 | 2.0 |
| Reasons for admissionb | ||
| Acute respiratory failure, septic | 39 | 37.1 |
| Acute respiratory failure, nonseptic | 18 | 17.1 |
| AKF | 1 | 0.9 |
| Sepsis | 37 | 33.6 |
| Sensory alteration | 4 | 3.8 |
| Bleeding | 1 | 1.0 |
| Oncologic emergencies | 1 | 1.0 |
| Post-operative | 1 | 1.0 |
| Ruptured spleen | 3 | 2.9 |
| Variables | Mean | Standard deviation |
|---|---|---|
| APACHE IIc | ||
| Mean (dp) | 18.3 | (6.4) |
| Time of hospitalization (days)d | ||
| Median (dp) | 19.1 | (20.5) |
| SOFA D1e | ||
| Mean (dp) | 8.7 | (3.6) |
| SOFA D3f | ||
| Mean (dp) | 11.1 | (5.0) |
| ΔSOFAg | ||
| Mean (dp) | 2.7 | (3.5) |
Ignored data: (a) 11; (b) 5; (c) 25; (d) 1; (e) 63; (f) 81; (g) 83.
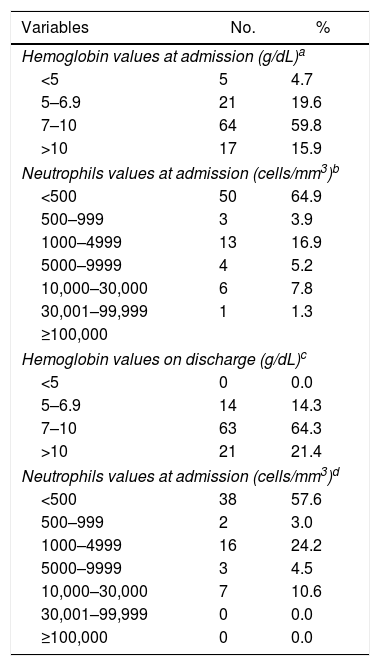
Distribution of patients with acute leukemia admitted to the ICU and blood cell count data at admission and discharge at the Hemope Foundation from 2006 to 2009.
| Variables | No. | % |
|---|---|---|
| Hemoglobin values at admission (g/dL)a | ||
| <5 | 5 | 4.7 |
| 5–6.9 | 21 | 19.6 |
| 7–10 | 64 | 59.8 |
| >10 | 17 | 15.9 |
| Neutrophils values at admission (cells/mm3)b | ||
| <500 | 50 | 64.9 |
| 500–999 | 3 | 3.9 |
| 1000–4999 | 13 | 16.9 |
| 5000–9999 | 4 | 5.2 |
| 10,000–30,000 | 6 | 7.8 |
| 30,001–99,999 | 1 | 1.3 |
| ≥100,000 | ||
| Hemoglobin values on discharge (g/dL)c | ||
| <5 | 0 | 0.0 |
| 5–6.9 | 14 | 14.3 |
| 7–10 | 63 | 64.3 |
| >10 | 21 | 21.4 |
| Neutrophils values at admission (cells/mm3)d | ||
| <500 | 38 | 57.6 |
| 500–999 | 2 | 3.0 |
| 1000–4999 | 16 | 24.2 |
| 5000–9999 | 3 | 4.5 |
| 10,000–30,000 | 7 | 10.6 |
| 30,001–99,999 | 0 | 0.0 |
| ≥100,000 | 0 | 0.0 |
Ignored data: (a) 3; (b) 33; (c) 12; (d) 44.
The main admission diagnosis was acute respiratory failure (ARF) secondary to sepsis (39/110, 37.1%), followed by sepsis (37/110, 33.6%). The other causes of admission appear in Table 1. At that point, the main infection was pulmonary and 30% of the blood cultures were positive, Pseudomonas aeruginosa and Klebsiella pneumoniae being the most common agents detected.
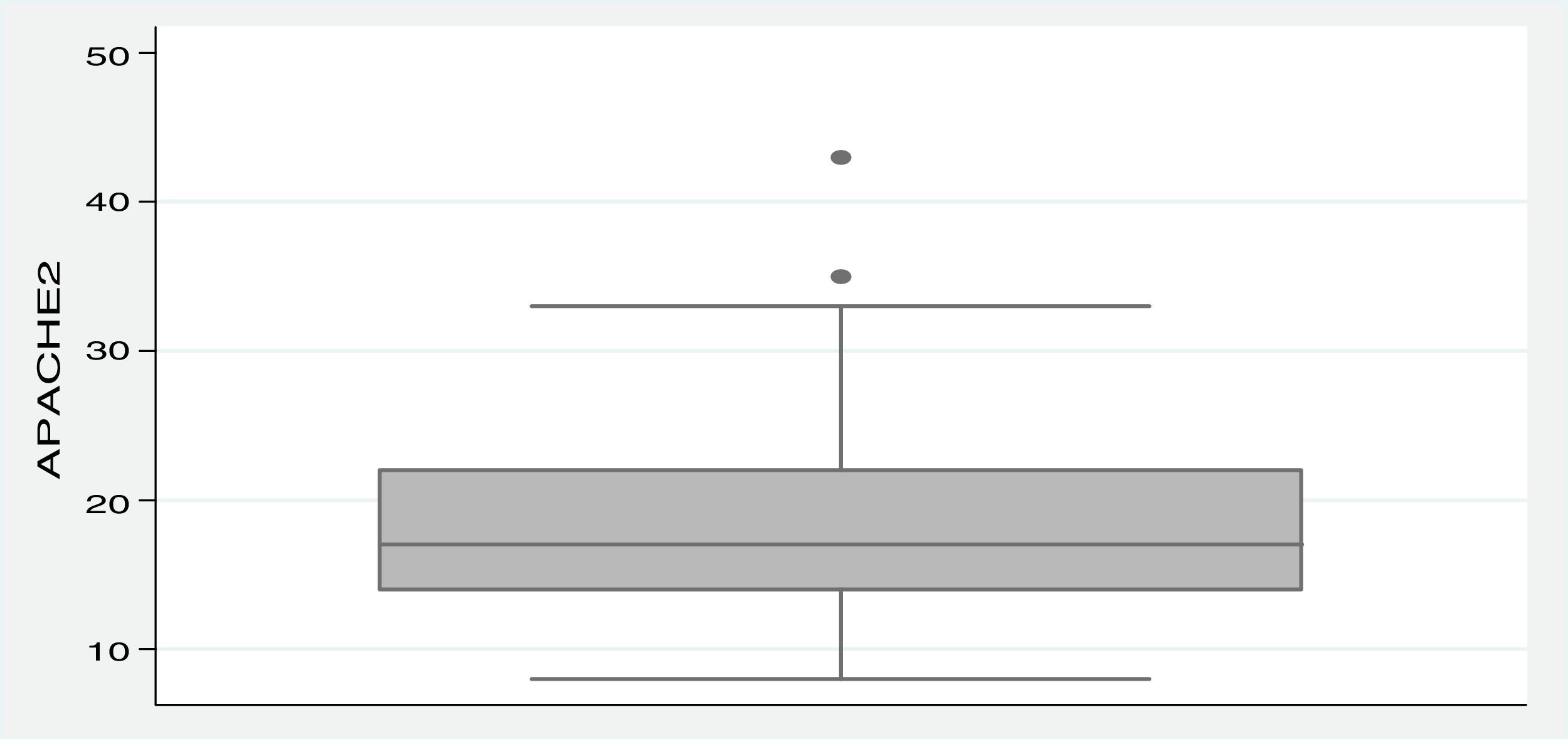
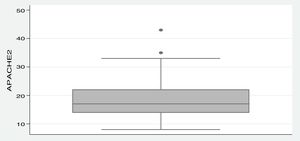
The APACHE II scores were calculated for 85 admitted patients (77.3%), due to the lack of data in the other 25 medical records. The mean APACHE II score for these 85 patients was 18.3 (±6.4), ranging from 8 to 43, as shown in Figure 1. The SOFA score was calculated retrospectively, however, on the first day of admission, 63 patients could not have the SOFA calculated, a number that increased to 81 on the third day. Thus, the mean variation in SOFA in 27 patients was 2.7 (±3.5).
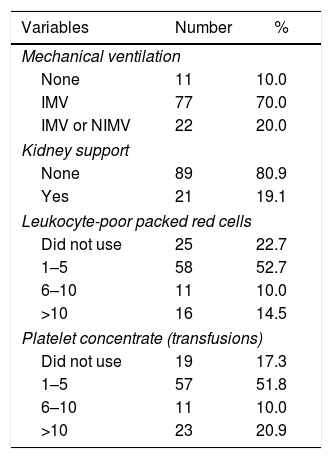
In regard to supportive care, 99/110 patients used mechanical ventilation (MV) of any kind, and only 21/110 needed RRT. The use of vasopressors on admission was not relevant. Among transfused patients, 52.7% received 1–5 units of leukocyte-poor packed red cells (LPPRC), and 51.8% received 1–5 platelet transfusions (Table 3).
Distribution of patients with acute leukemia hospitalized in the ICU according to supportive therapies applied. Hemope Foundation, 2006 to 2009.
| Variables | Number | % |
|---|---|---|
| Mechanical ventilation | ||
| None | 11 | 10.0 |
| IMV | 77 | 70.0 |
| IMV or NIMV | 22 | 20.0 |
| Kidney support | ||
| None | 89 | 80.9 |
| Yes | 21 | 19.1 |
| Leukocyte-poor packed red cells | ||
| Did not use | 25 | 22.7 |
| 1–5 | 58 | 52.7 |
| 6–10 | 11 | 10.0 |
| >10 | 16 | 14.5 |
| Platelet concentrate (transfusions) | ||
| Did not use | 19 | 17.3 |
| 1–5 | 57 | 51.8 |
| 6–10 | 11 | 10.0 |
| >10 | 23 | 20.9 |
IMV: invasive mechanical ventilation; NIMV: non-invasive mechanical ventilation.
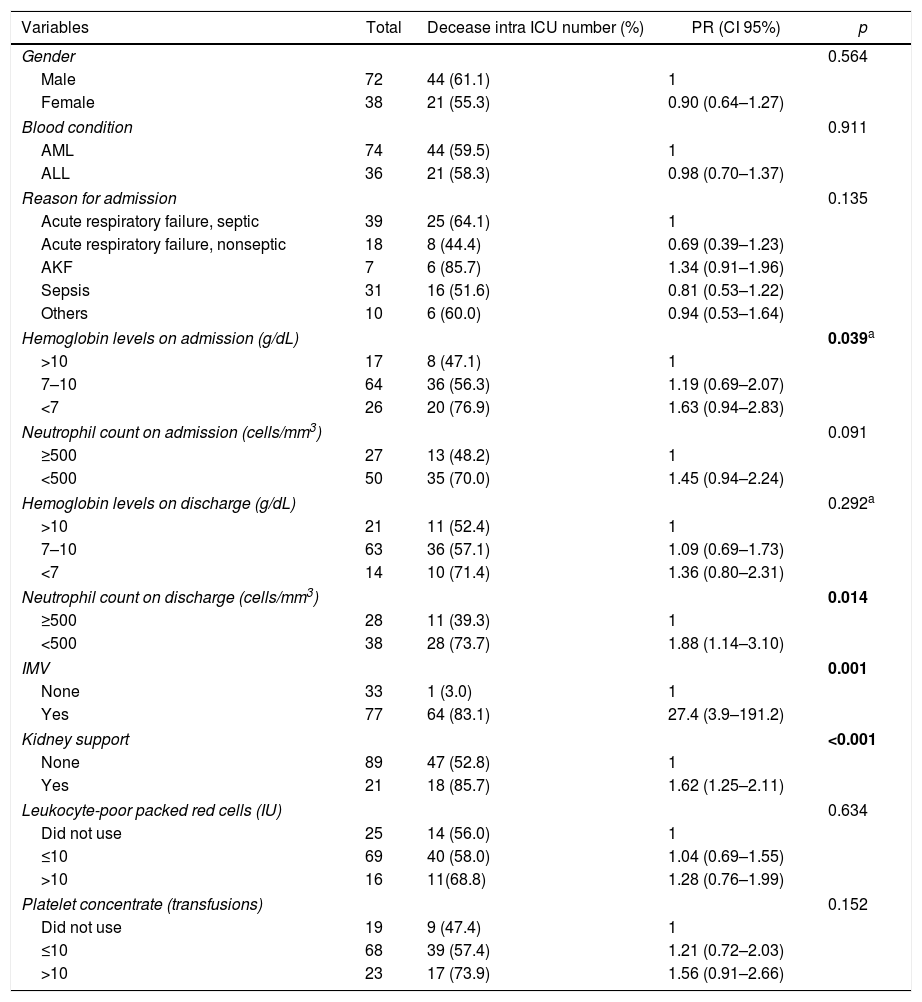
After bivariate analysis, mortality among individuals who underwent hemodialysis was higher than those who did not (p<0.001), and the use of MV might also be a factor associated with higher mortality rates (p=0.001) in this scenario. We additionally found that patients who had a higher hemoglobin value (p=0.039) and more than 500neutrophils/mm3 in the blood count (p=0.014) at admission were less likely to die (Table 4).
Distribution of patients with acute leukemia hospitalized in the ICU, according to their characteristics and occurrence of death, at the Hemope Foundation from 2006 to 2009.
| Variables | Total | Decease intra ICU number (%) | PR (CI 95%) | p |
|---|---|---|---|---|
| Gender | 0.564 | |||
| Male | 72 | 44 (61.1) | 1 | |
| Female | 38 | 21 (55.3) | 0.90 (0.64–1.27) | |
| Blood condition | 0.911 | |||
| AML | 74 | 44 (59.5) | 1 | |
| ALL | 36 | 21 (58.3) | 0.98 (0.70–1.37) | |
| Reason for admission | 0.135 | |||
| Acute respiratory failure, septic | 39 | 25 (64.1) | 1 | |
| Acute respiratory failure, nonseptic | 18 | 8 (44.4) | 0.69 (0.39–1.23) | |
| AKF | 7 | 6 (85.7) | 1.34 (0.91–1.96) | |
| Sepsis | 31 | 16 (51.6) | 0.81 (0.53–1.22) | |
| Others | 10 | 6 (60.0) | 0.94 (0.53–1.64) | |
| Hemoglobin levels on admission (g/dL) | 0.039a | |||
| >10 | 17 | 8 (47.1) | 1 | |
| 7–10 | 64 | 36 (56.3) | 1.19 (0.69–2.07) | |
| <7 | 26 | 20 (76.9) | 1.63 (0.94–2.83) | |
| Neutrophil count on admission (cells/mm3) | 0.091 | |||
| ≥500 | 27 | 13 (48.2) | 1 | |
| <500 | 50 | 35 (70.0) | 1.45 (0.94–2.24) | |
| Hemoglobin levels on discharge (g/dL) | 0.292a | |||
| >10 | 21 | 11 (52.4) | 1 | |
| 7–10 | 63 | 36 (57.1) | 1.09 (0.69–1.73) | |
| <7 | 14 | 10 (71.4) | 1.36 (0.80–2.31) | |
| Neutrophil count on discharge (cells/mm3) | 0.014 | |||
| ≥500 | 28 | 11 (39.3) | 1 | |
| <500 | 38 | 28 (73.7) | 1.88 (1.14–3.10) | |
| IMV | 0.001 | |||
| None | 33 | 1 (3.0) | 1 | |
| Yes | 77 | 64 (83.1) | 27.4 (3.9–191.2) | |
| Kidney support | <0.001 | |||
| None | 89 | 47 (52.8) | 1 | |
| Yes | 21 | 18 (85.7) | 1.62 (1.25–2.11) | |
| Leukocyte-poor packed red cells (IU) | 0.634 | |||
| Did not use | 25 | 14 (56.0) | 1 | |
| ≤10 | 69 | 40 (58.0) | 1.04 (0.69–1.55) | |
| >10 | 16 | 11(68.8) | 1.28 (0.76–1.99) | |
| Platelet concentrate (transfusions) | 0.152 | |||
| Did not use | 19 | 9 (47.4) | 1 | |
| ≤10 | 68 | 39 (57.4) | 1.21 (0.72–2.03) | |
| >10 | 23 | 17 (73.9) | 1.56 (0.91–2.66) | |
PR: prevalence rate; IMV: invasive mechanical ventilation; LPPRC: leukocyte-poor packed red cells; PC: platelet concentrate. Bold values- the Values with p<0,001 or tending to 0,001
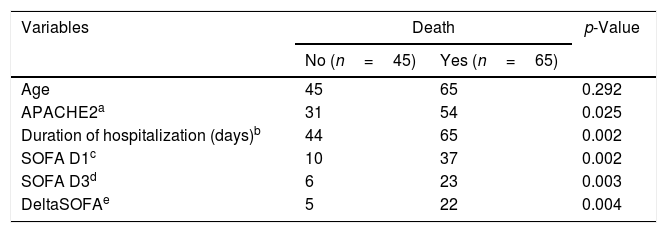
The summary and comparison of the central tendency measurements of these variables among Hemope-ICU patients appear in Table 5. Variables independently associated with the mortality rate in this population were evaluated with a multiple Cox regression with robust variance. In this model, the following variables were included: having undergone RRT, used IMV, stayed longer in the ICU, presented higher APACHE II scores, presented higher Hb values on admission, had an increase in neutrophils on discharge, and had a higher number of platelet transfusions. The SOFA values were not analyzed due to the significant loss of information.
Descriptive statistics of quantitative variables of patients with acute leukemia, according to occurrence of death, at the Hemope Foundation from 2006 to 2009.
| Variables | Death | p-Value | |
|---|---|---|---|
| No (n=45) | Yes (n=65) | ||
| Age | 45 | 65 | 0.292 |
| APACHE2a | 31 | 54 | 0.025 |
| Duration of hospitalization (days)b | 44 | 65 | 0.002 |
| SOFA D1c | 10 | 37 | 0.002 |
| SOFA D3d | 6 | 23 | 0.003 |
| DeltaSOFAe | 5 | 22 | 0.004 |
Ignored data (a) 25; (b) 11 (c) 63; (d) 81; (e) 83.
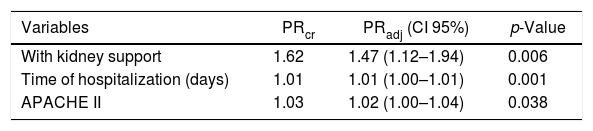
Among the sample of patients with acute leukemia in this study, the mortality in the Hemope ICU was independently associated with RRT [PRadj 1.47 (1.12–1.94)], longer hospitalization [PRadj 1.01 (1.00–1.01)] and higher APACHE II scores [PRadj 1.02 (1.00–1.04)]. Mortality in this setting for patients who underwent RRT was 47% higher than among those who did not (p=0.006), regardless of the ICU hospitalization time and the APACHE II score. Death risk also increased by 1% (p=0.001) for each additional day at the unit, independently of the APACHE II score and of having RRT or not. In addition, the increase of one unit in the APACHE II score relates to a 2% increase in the mortality rate (p=0.038), independently of having undergone RRT or not (Table 6).
Estimation of the mortality prevalence ratio among patients with acute leukemia, with the multiple Cox regression model.
| Variables | PRcr | PRadj (CI 95%) | p-Value |
|---|---|---|---|
| With kidney support | 1.62 | 1.47 (1.12–1.94) | 0.006 |
| Time of hospitalization (days) | 1.01 | 1.01 (1.00–1.01) | 0.001 |
| APACHE II | 1.03 | 1.02 (1.00–1.04) | 0.038 |
PRcr: crude prevalence ratio; PRadj: adjusted prevalence ratio.
We analyzed 110 patients with acute leukemias during critical illness. This is a rarely found patient profile in general ICUs and there are few ICUs which are specialized in hematological diseases around the world. Therefore, describing this population and evaluating predictors of outcome are very important to improve knowledge, not only about their critical illness, but also about their prognosis during the stay in the ICU.
We found a high mortality rate in the studied population (59.1%), being RRT the most important risk factor. This mortality seems not to be different from those previously reported by Azoulay et al. and Abraham et al. in cancer patients in the ICU.5,6 Twenty-nine percent of the patients were admitted with AKF and the mortality rate was 85% for those who needed hemodialysis. These data are similar to those formerly reported by Santos et al. Twelve percent to 49% of the AKF rate among cancer patients and a higher mortality were related to RRT (80%). Although these results are poor, they are in line with the outcomes found in non-cancer patients admitted to the ICU with AKF.22,23
Other important predictors of mortality were longer hospitalization time at the unit and increase in the APACHE II score. We did not find any description related to the length of hospitalization in other studies. And although the increase in the APACHE II score has been associated with a higher chance of death in the ICU, this index was not able to properly estimate mortality in this study because an average APACHE II score of 18 predicts a mortality rate of 20–30%, which is very far from the mortality rates in our study. Despite this disparity, similar data have already been described in publications by Hampshire and Jonge.24,25
Sepsis was the reason for admission for almost 70% in this study. Sepsis is a frequent condition among patients admitted to ICUs and also among patients with cancer. Its mortality rate is around 30–50%, not only for cancer patients, but also for the general population during critical illness. Therefore, despite having a high mortality rate in our study, it was not so different from the rate found among septic patients without cancer. Consequently, we must think about leukemic patients in this setting, as patients with a severe life-threatening disease, but with an almost 50–70% chance of surviving, when admitted to the ICU.26–29
There was also a tendency for lower mortality when there was a higher hemoglobin level on admission (p=0.039) and when neutrophil levels were higher than 500cells/mm3 on discharge (p=0.014). One can think that recovering from neutropenia may be a protecting factor against mortality in this scenario, but at this point, as also mentioned in former publications, studies with a greater number of patients are needed to confirm or refute this trend.26
Finally, the predictors of mortality found in our study are also in accordance with ICU studies related and not related to cancer patients. In this manner, it is important to note that to offer ICU support to leukemic patients is to give them a chance to survive after critical illness. Of course, multicenter prospective studies with a control population may be necessary to elucidate many other questions.
ConclusionOur mortality rate was high, but not different from patients admitted to ICUs for sepsis without leukemias or other oncologic diseases. Predictors of higher mortality were: longer hospitalization, day-by-day increasing APACHE II scores and undergoing hemodialysis, which is also similar to the general population with critical illness.
All these data are important for public health because they call attention to the fact that factors associated with death in the leukemic population are not different from the reasons for death in the general population during critical illness. Therefore, it might be important to revisit admission policies in the ICU, and perhaps, to modify the ranking of priority related to leukemia patients, which may improve the outcomes after critical illnesses in this population.
Conflicts of interestThe authors declare no conflicts of interest.
We would like to thank Prof. Dr. Cesar de Almeida Neto of the Fundação Pró-Sangue, Hemocentro de São Paulo and Department of Medical Sciences at the College of Medicine, University of São Paulo, for his insightful comments, which improved our manuscript.