Diversity in Classical Hematology Research
More infoData on the prevalence of clinically significant antigens (Rh, Kell, Kidd, Duffy, MNSs, Lewis, P and Lutheran) among the Indian donor population is sparse.
ObjectiveThis prospective study was aimed at determining the prevalence of 21 clinically significant antigens for the first time in the South Indian donor population.
MethodA total of 672 regular O group blood donors were enrolled for Rh (C,c, E, e) and Kell (K) antigens typing. Of these, 188 donors were typed for other clinically significant antigens (k, Kpa, Kpb, Jka, Jkb, Fya, Fyb, M, N, S, s, P1, Lea, Leb, Lua and Lub).
ResultsAntigen frequencies were expressed in percentages. In our study, R1R1 and rr were the most common phenotypes among D+ and D- donors, respectively. Among the Rh antigens, the e antigen was expressed by 97.5% and 100% of D+ and D- donors, respectively. The K antigen was found in only 0.15% of donors. In the Duffy and Kidd blood group system, Fy (a+b+) and Jk (a+b+) were the most frequent phenotypes, respectively. In the MNSs blood group system, M+N+ and S-s+ were the most common phenotypes reported. The Le (a-b+) was found to be the phenotype with the highest prevalence in the Lewis blood group system. The Lu (a-b+) was the only phenotype found in the Lutheran blood group system.
ConclusionKnowledge regarding the prevalence of antigens in a given population is essential in developing cost-effective in-house panels and a rare donor registry comprising donors typed negative for a high-frequency antigen or a combination of common multiple antigens.
To date, 43 blood group systems and 348 red cell antigens have been officially recognized by the International Society of Blood Transfusion (accessed through https://www.isbtweb.org/working-parties/red-cell-immunogenetics-and-blood-group-terminology).1 Of these, antigens of ABO and Rh (mainly D) blood group system are given the utmost importance in terms of transfusion and transplantation. Thanks to the progress in the immunohematology discipline, antibodies to antigens other than AB/D (namely antigens of Rh, Kell, Kidd, Duffy, MNS, Lewis, P1PK and Lutheran blood group systems) have also been frequently encountered in the clinical transfusion practice. These antibodies are primarily implicated in hemolytic transfusion reactions and hemolytic disease in the fetus and newborn and are often associated with the reduced in vivo survival of the antigen-carrying red cells.2 Of note, in everyday clinical practice, red cell antigen phenotyping is employed under few special circumstances, namely: 1. to identify or confirm the specificity of the alloantibody/autoantibody in an individual; 2. to perform donor antigen typing to find a compatible unit for an alloimmunized recipient, and; 3. to perform prophylactic extended antigen matched transfusions in the non-alloimmunized or alloimmunized recipient. However, such discrete observations may not be adequate to determine the pattern of allo/autoimmunization and study its impact on the transfusion recipients/antenatal patient cohort. To accomplish this objective, red cell antigen prevalence studies of any given population are indispensable. It is well known that the distribution of blood group antigens among individuals is variable, depending on the race/ethnicity that those individuals belong to. While vast information in the literature is available on the prevalence of red cell antigens among different populations, such as Whites, Blacks and Chinese,3,4 only very few reports exist in the Indian population. Hence, the current study was aimed at estimating the prevalence of 21 common clinically significant red cell antigens of various blood group systems serologically, which included Rh (C, c, E and e), Kell (K, k, Kpa and Kpb), Kidd (Jka and Jkb), Duffy (Fya and Fyb), MNS (M, N, S and s), P1PK (P1), Lewis (Lea and Leb) and Lutheran (Lua and Lub), in the South Indian donor population. To the best of our knowledge, this is the first study on the prevalence of blood group systems in South India (other than ABO and RhD).
MethodsThis prospective study was conducted from January 2019 to January 2020 in the Department of Transfusion Medicine in a 1,000-bed tertiary care hospital in South India. Our hospital is a well-established solid-organ and stem cell transplant center which offers treatment for both adult and pediatric patient populations. Our blood center is a regional blood transfusion center catering to more than 15,000 patients annually. The study was duly approved by the Institutional Research Ethics Committee and written consent had been obtained from the donors participating in the study at the time of enrollment. Regular blood donors were selected as per the donor selection criteria laid down by the Drugs and Cosmetics Act, 1945 and the rules therein. Blood donors who did not belong to the region were excluded. During blood donation, 3ml of the blood sample were collected from each donor in sample tubes containing ethylenediaminetetraacetic acid anticoagulant, using the diversion pouch. Each blood donor was given a unique identification number and the samples were barcoded simultaneously. A total of 672 'O' blood group donor samples were included in the study. All the immunohematological tests in this study were performed with the column agglutination technology (CAT). Donor samples were tested for the ABO blood group and Rh typing with monoclonal antisera (DiaClon ABO/D+Reverse grouping) using a fully automated immunohematology system (IH500, Bio-Rad, Cressier, Switzerland). The RhD negative samples were further subjected to weak D testing, using IgG monoclonal antisera anti-D (Tulip Diagnostics, Goa, India). The direct antiglobulin test (DAT) was performed on all donor samples, using the polyspecific (IgG+C3d) Coombs reagent. Only DAT negative samples were included.
The Rh-K phenotyping (C, c, E, e and K) was performed on all the samples. Of the 672 samples, 188 samples were randomly selected for extended red cell phenotyping of other antigens (including k, Kpa, Kpb, Jka, Jkb, Fya, Fyb, M, N, S, s, P1, Lea, Leb, Lua and Lub). The number of samples typed for the antigens varied, depending on the availability of reagents. Extended phenotyping for all the antigens was performed using ID-Diaclon gel cards (Bio-Rad, Cressier, Switzerland). The Rh-K phenotyping was done using the Diaclon Rh-subgroups+K phenotyping. Single antigen testing gel cards were used for phenotyping of the other antigens. A 5% red cell suspension was prepared in bromelain for the phenotyping of the P1, Lea, Leb, Kpa, Kpb, Jka, Jkb, Lua and Lub antigens. A 0.8% low-ionic strength solution was used for the preparation of red cell suspension while phenotyping for the Rh-K, k, M, N, S, s, Fya and Fyb antigens. Known positive and negative controls for each antigen were selected from the commercial cell panels (DiaCell and DiaPanel, Bio-Rad, Cressier Switzerland) and used appropriately. The test procedures for antigen phenotyping were performed as per the manufacturer's instructions. The test results thus derived using the CAT were interpreted as follows: the grade of agglutination was noted to range from 4+ to negative. (4+ - a solid red line at the top of the gel column; 3+ - agglutinates covering the upper half of the gel column; 2+ - agglutinates dispersed throughout the length of the gel column; 1+ - agglutinates limiting to lower half of the gel column, and; negative – a compact red button at the bottom of the gel column).
The total number of donors who tested positive for a particular antigen or phenotype divided by the total number of donors tested yielded the prevalence of that particular antigen or phenotype and the results were expressed in percentages.
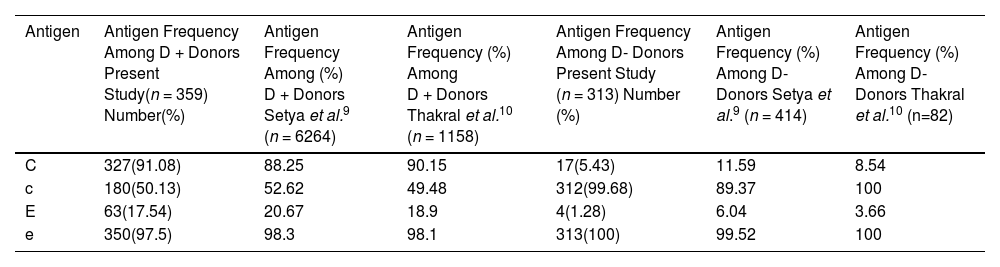
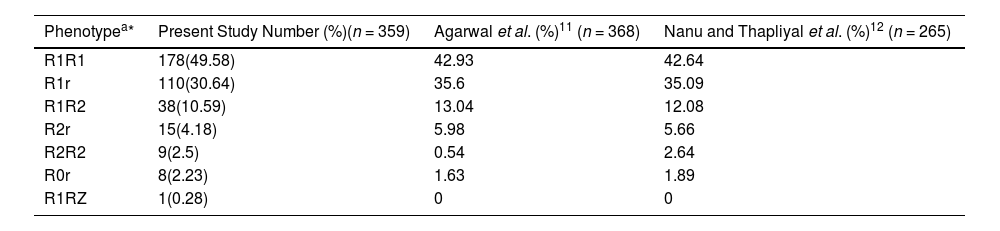
ResultsA total of 672 donors were typed for Rh (C, c, E and e) and K antigens. Of these, 359 donors were D+ and the remaining 313 donors were D-. No individual was noted to have the variant D. The Rh phenotypes mentioned in this study are presumed to be the most probable phenotypes of the study population. Among the Rh antigens, the e antigen was found to be the most prevalent antigen, with a frequency of 97.5% and 100% among the D+ and D- donors, respectively. The C antigen was found more frequently in D+ donors, when compared to D- donors (91.08% vs. 5.43%, respectively). The c antigen was expressed by 99.68% of D- donors, while only 50.13% D+ donors expressed the c antigen. The E antigen was found in 17.54 % and 1.28% of D+ and D- donors, respectively. Table 1 describes the prevalence of Rh antigens among D+ and D- donors observed in the present study. A total of 7 Rh phenotypes were observed among the D+ donors. The R1R1 phenotype was the most frequent (49.58%), followed by the R1r (30.64%) and R1R2 (10.59%). A rare phenotype R1RZ was documented in the current study in one donor, with a frequency of 0.28%. Among the D- donors, the rr phenotype (93.29%) was observed to be the most frequent, followed by the r'r (5.11%). An unusual phenotype r'r' was noted in one donor (0.32%). The various Rh phenotypes among D+ and D- donors and their prevalence in the present study population have been listed in Tables 2 and 3, respectively.
Prevalence of Rh antigens among D+ and D- donors in the present study and other studies in India.
| Antigen | Antigen Frequency Among D + Donors Present Study(n = 359) Number(%) | Antigen Frequency Among (%) D + Donors Setya et al.9 (n = 6264) | Antigen Frequency (%) Among D + Donors Thakral et al.10 (n = 1158) | Antigen Frequency Among D- Donors Present Study (n = 313) Number (%) | Antigen Frequency (%) Among D- Donors Setya et al.9 (n = 414) | Antigen Frequency (%) Among D- Donors Thakral et al.10 (n=82) |
|---|---|---|---|---|---|---|
| C | 327(91.08) | 88.25 | 90.15 | 17(5.43) | 11.59 | 8.54 |
| c | 180(50.13) | 52.62 | 49.48 | 312(99.68) | 89.37 | 100 |
| E | 63(17.54) | 20.67 | 18.9 | 4(1.28) | 6.04 | 3.66 |
| e | 350(97.5) | 98.3 | 98.1 | 313(100) | 99.52 | 100 |
Rh phenotypes among D+ donors in the present study and other studies in India.
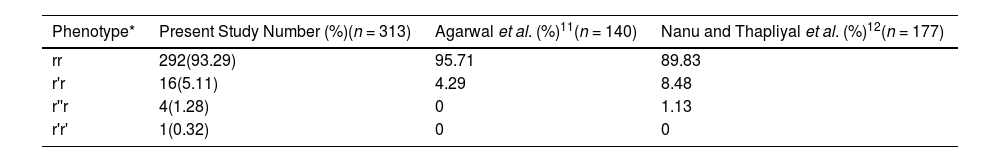
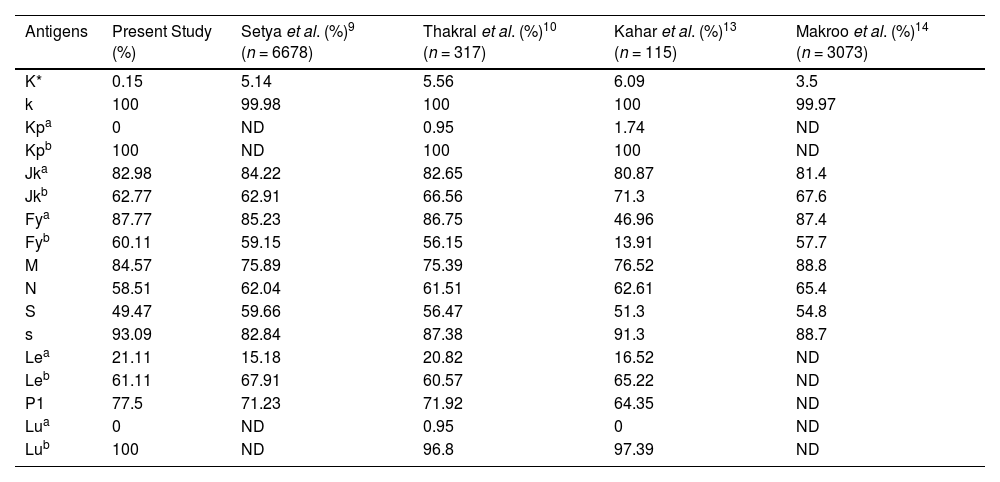
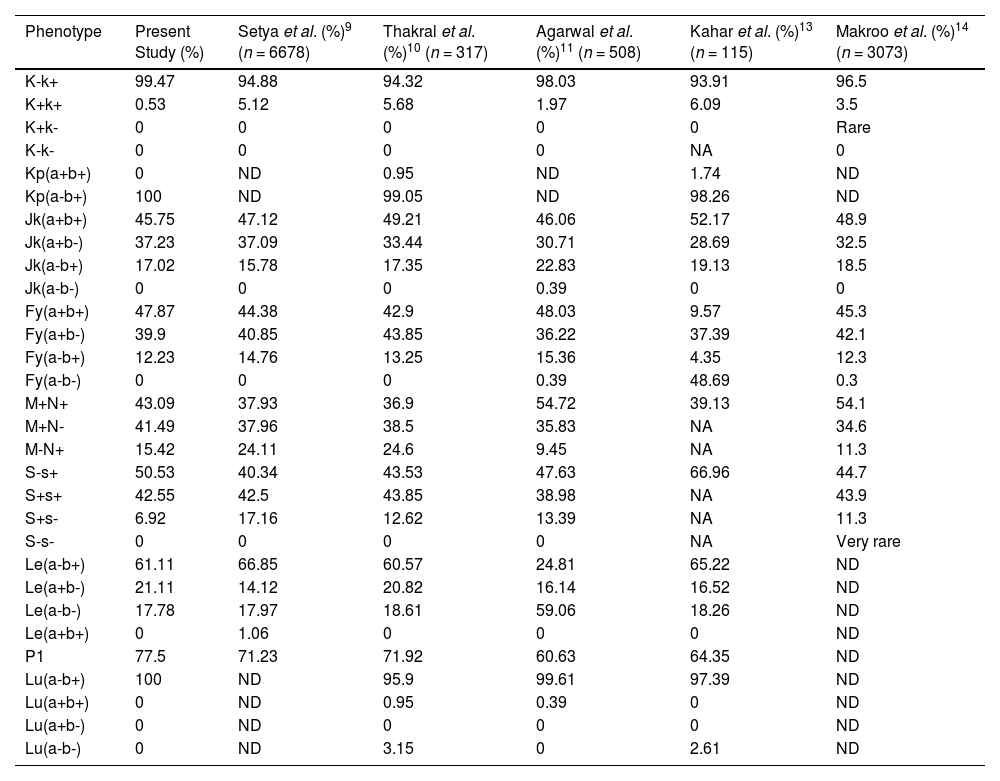
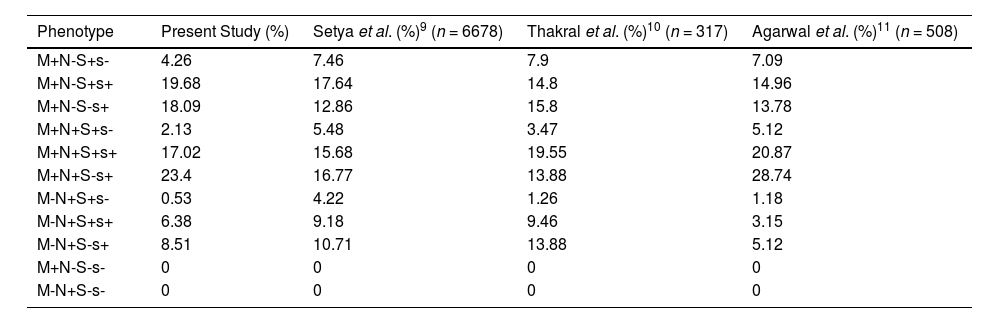
With respect to the Kell blood group system, the K antigen was present in 0.15% of the donors. The k and Kpb antigens were found in 100% of our donors. The rare phenotype Kp(a+b+) was not observed in any individual. In the Kidd blood group system, the Jka antigen was found in 82.98% of the donors, while 62.77% of the donors expressed the Jkb antigen on their red cells. The Jk(a+b+) was the most common phenotype (45.75%) reported in the current study. In the Duffy blood group system, Fya and Fyb antigens were expressed by 87.77% and 60.11% of the donors, respectively. Of the Duffy phenotypes, Fy(a+b+) was the most frequent phenotype reported (47.87%). Null phenotypes, such as the Jk(a-b-) and Fy(a-b-), were not reported in the present study. Among the antigens of the MNSs blood group system, 93.09% and 84.57% of the donors expressed s and M antigens, respectively. The most common phenotypes were as follows: M+N+ (43.09%) and S-s+ (50.53%). Of all the possible phenotypic combinations, the M+N+S-s+ was the most frequent (23.4%), followed by the M+N-S+s+ (19.68%) and M-N+S+s-, a rare phenotype was noted in one individual (0.53%). In the Lewis blood group system, the Le(a-b+) was the most frequent phenotype observed (61.11%), while the Le(a-b-) phenotype was found in 17.78% of the donors. In the P1PK system, the P1 antigen was noted in 77.5% of the donor samples tested. Among the antigens of the Lutheran blood group system, all the donors expressed the Lub antigen (100%), while none of the donors expressed the Lua antigen. Tables 4 and 5 enumerate the prevalence of other blood group antigens and their phenotypes, respectively. The possible combination of phenotypes in the MNSs blood group system, along with their estimated prevalence, has been summarized in Table 6.
Prevalence of other red cell antigens in the present study (n = 188) and other studies in India.
| Antigens | Present Study (%) | Setya et al. (%)9 (n = 6678) | Thakral et al. (%)10 (n = 317) | Kahar et al. (%)13 (n = 115) | Makroo et al. (%)14 (n = 3073) |
|---|---|---|---|---|---|
| K* | 0.15 | 5.14 | 5.56 | 6.09 | 3.5 |
| k | 100 | 99.98 | 100 | 100 | 99.97 |
| Kpa | 0 | ND | 0.95 | 1.74 | ND |
| Kpb | 100 | ND | 100 | 100 | ND |
| Jka | 82.98 | 84.22 | 82.65 | 80.87 | 81.4 |
| Jkb | 62.77 | 62.91 | 66.56 | 71.3 | 67.6 |
| Fya | 87.77 | 85.23 | 86.75 | 46.96 | 87.4 |
| Fyb | 60.11 | 59.15 | 56.15 | 13.91 | 57.7 |
| M | 84.57 | 75.89 | 75.39 | 76.52 | 88.8 |
| N | 58.51 | 62.04 | 61.51 | 62.61 | 65.4 |
| S | 49.47 | 59.66 | 56.47 | 51.3 | 54.8 |
| s | 93.09 | 82.84 | 87.38 | 91.3 | 88.7 |
| Lea | 21.11 | 15.18 | 20.82 | 16.52 | ND |
| Leb | 61.11 | 67.91 | 60.57 | 65.22 | ND |
| P1 | 77.5 | 71.23 | 71.92 | 64.35 | ND |
| Lua | 0 | ND | 0.95 | 0 | ND |
| Lub | 100 | ND | 96.8 | 97.39 | ND |
Prevalence of antigen phenotypes among the various blood group systems in the present study (n = 188) and other studies in India.
| Phenotype | Present Study (%) | Setya et al. (%)9 (n = 6678) | Thakral et al. (%)10 (n = 317) | Agarwal et al.(%)11 (n = 508) | Kahar et al. (%)13 (n = 115) | Makroo et al. (%)14 (n = 3073) |
|---|---|---|---|---|---|---|
| K-k+ | 99.47 | 94.88 | 94.32 | 98.03 | 93.91 | 96.5 |
| K+k+ | 0.53 | 5.12 | 5.68 | 1.97 | 6.09 | 3.5 |
| K+k- | 0 | 0 | 0 | 0 | 0 | Rare |
| K-k- | 0 | 0 | 0 | 0 | NA | 0 |
| Kp(a+b+) | 0 | ND | 0.95 | ND | 1.74 | ND |
| Kp(a-b+) | 100 | ND | 99.05 | ND | 98.26 | ND |
| Jk(a+b+) | 45.75 | 47.12 | 49.21 | 46.06 | 52.17 | 48.9 |
| Jk(a+b-) | 37.23 | 37.09 | 33.44 | 30.71 | 28.69 | 32.5 |
| Jk(a-b+) | 17.02 | 15.78 | 17.35 | 22.83 | 19.13 | 18.5 |
| Jk(a-b-) | 0 | 0 | 0 | 0.39 | 0 | 0 |
| Fy(a+b+) | 47.87 | 44.38 | 42.9 | 48.03 | 9.57 | 45.3 |
| Fy(a+b-) | 39.9 | 40.85 | 43.85 | 36.22 | 37.39 | 42.1 |
| Fy(a-b+) | 12.23 | 14.76 | 13.25 | 15.36 | 4.35 | 12.3 |
| Fy(a-b-) | 0 | 0 | 0 | 0.39 | 48.69 | 0.3 |
| M+N+ | 43.09 | 37.93 | 36.9 | 54.72 | 39.13 | 54.1 |
| M+N- | 41.49 | 37.96 | 38.5 | 35.83 | NA | 34.6 |
| M-N+ | 15.42 | 24.11 | 24.6 | 9.45 | NA | 11.3 |
| S-s+ | 50.53 | 40.34 | 43.53 | 47.63 | 66.96 | 44.7 |
| S+s+ | 42.55 | 42.5 | 43.85 | 38.98 | NA | 43.9 |
| S+s- | 6.92 | 17.16 | 12.62 | 13.39 | NA | 11.3 |
| S-s- | 0 | 0 | 0 | 0 | NA | Very rare |
| Le(a-b+) | 61.11 | 66.85 | 60.57 | 24.81 | 65.22 | ND |
| Le(a+b-) | 21.11 | 14.12 | 20.82 | 16.14 | 16.52 | ND |
| Le(a-b-) | 17.78 | 17.97 | 18.61 | 59.06 | 18.26 | ND |
| Le(a+b+) | 0 | 1.06 | 0 | 0 | 0 | ND |
| P1 | 77.5 | 71.23 | 71.92 | 60.63 | 64.35 | ND |
| Lu(a-b+) | 100 | ND | 95.9 | 99.61 | 97.39 | ND |
| Lu(a+b+) | 0 | ND | 0.95 | 0.39 | 0 | ND |
| Lu(a+b-) | 0 | ND | 0 | 0 | 0 | ND |
| Lu(a-b-) | 0 | ND | 3.15 | 0 | 2.61 | ND |
*ND- not done; NA- not available.
Prevalence of combination of phenotypes in MNSs blood group system in the present study (n = 188) and other studies in India.
| Phenotype | Present Study (%) | Setya et al. (%)9 (n = 6678) | Thakral et al. (%)10 (n = 317) | Agarwal et al. (%)11 (n = 508) |
|---|---|---|---|---|
| M+N-S+s- | 4.26 | 7.46 | 7.9 | 7.09 |
| M+N-S+s+ | 19.68 | 17.64 | 14.8 | 14.96 |
| M+N-S-s+ | 18.09 | 12.86 | 15.8 | 13.78 |
| M+N+S+s- | 2.13 | 5.48 | 3.47 | 5.12 |
| M+N+S+s+ | 17.02 | 15.68 | 19.55 | 20.87 |
| M+N+S-s+ | 23.4 | 16.77 | 13.88 | 28.74 |
| M-N+S+s- | 0.53 | 4.22 | 1.26 | 1.18 |
| M-N+S+s+ | 6.38 | 9.18 | 9.46 | 3.15 |
| M-N+S-s+ | 8.51 | 10.71 | 13.88 | 5.12 |
| M+N-S-s- | 0 | 0 | 0 | 0 |
| M-N+S-s- | 0 | 0 | 0 | 0 |
Red cell alloimmunization poses a huge challenge to the recipients of blood transfusion, especially the multi-transfused patient population. Antibody response in a transfused individual is influenced by several factors, such as immunogenicity of the antigen, antigen frequency in the donor population, underlying disease and genetic factors.5 There is plenty of data on the rate of red cell alloimmunization and its serological characteristics in our patient/donor population, in contrast to the sparse literature evidence on the prevalence of clinically important antigens. It has been explicitly shown that the antibodies to Rh-K and MNS blood group antigens are among the commonly reported specificities in these studies.6,7,8 Only a few studies (predominantly from the northern and western parts of the country) have reported the frequencies of clinically significant antigens among their donor population.9-14 As shown in the present study, the R1R1 and R1r (among D+ donors) and rr (among the D- donors) were found to be the most frequent Rh antigen phenotypes in virtually all the studies conducted in India. In these studies, without exception, the 'e' antigen was the most frequent among the Rh antigens, a finding concordant with findings of the current study.9 The K antigen was detected in 0.15% of our donors and its prevalence has been shown to vary among different Indian populations. While the studies from North India conducted by Thakral et al. and Setya et al. reported that 5.56% and 5.14% of their donors expressed the K antigen, respectively, one study from eastern India reported a low antigen prevalence of 0.79%, resembling the data observed in a non-Caucasian population.15 To the best of our knowledge, there are no studies that have evaluated the prevalence of the K-antigen among the South Indian population and future studies from the southern part of India may shed light on this issue. The K-k+ was certainly the most common phenotype observed in our Indian donor population.9
Almost all the studies from India reported that the Jka and Jk(a+b+) were the most common antigen and antigen phenotypes of the Kidd system, as noted in the present study.9-14 Several studies noted that the Fya and Fy(a+b+) were the most frequent antigen and antigen phenotypes of the Duffy blood group system, conforming to the findings of the present study.9 On the other hand, according to Thakral et al., the Fy(a+b-) phenotype was found to be the most prevalent phenotype among their donors.10 The null phenotypes Fy(a-b-) and Jk(a-b-) were rarely found in the Indian population, apart from a study conducted by Kahar et al. in Western India, which demonstrated the Fy(a-b-) to be the most prevalent phenotype, occurring in 48.69% of their donor population.13 Similar to the findings of the current study, Agarwal et al. observed that the M+N+ and S-s+ were found to be the most frequent phenotypes,11 while Thakral and colleagues reported the M+N- and S+s+ as their most frequent phenotypes.10 Among the phenotype combinations of MNS antigens, the M+N+S-s+ was the most frequent phenotype in the present study, while the studies conducted by Setya et al. and Thakral et al. reported the most common phenotypes to be M+N-S+s+ and M+N+S+s+, respectively.9,10 Most of the studies in India reported the Leb and Le(a-b+) to be the most common antigen and antigen phenotypes encountered in the Lewis blood group system,9,10 in agreement with the findings of the current study. In contrast, Agarwal et al. showed that the Le(a-b-) phenotype was their most frequent phenotype.11 Although the Lu(a-b+) was the only phenotype observed in the current study in the Lutheran blood group system, the Lu(a+b+) and Lu(a-b-) were noted as very rare phenotypes by Thakral et al.10 Based on these findings, it appears that the prevalence of red cell antigens and their phenotypes is influenced by the ethnicity of the study population, even within a country.
Red cell antigen prevalence studies are indeed useful in an immunohematology setup in the following ways: 1. Based on the estimated antigen prevalence, cost-effective in-house antibody screening panels can be developed, targeting the common antibody specificities and excluding the high prevalence antigens of the population (the k, Kpb, and Lub antigens have been found in 100% of our donors); 2. Additionally, antigen prevalence data are utilized in predicting the number of units needed to be crossmatched/typed to find a compatible unit. In a previously published report from our institute, based on the existing antigen prevalence data on the Indian population, it was calculated that 230 units would be required to find 2 compatible units in a prospective renal transplant recipient with 5 different alloantibodies. The 2 units were identified after typing 254 units, as predicted;16 3. Rare blood donors are identified by the typing of a large number of donors for various red cell antigens. As the antigen frequencies vary among different populations, the definition of a rare donor tends to vary accordingly in different countries. Broadly, a rare donor is recognized as the one who is typed negative 1, for high prevalence antigens occurring in 1 among 1,000 individuals (while it is 4 per 1,000 in France and 1 in 100 to 1 in 1,000 in Japan) or 2, for a combination of common antigens occurring in 1 per 200 to 1 per 1,000 individuals.17,18 In a study conducted by the Indian Council of Medical Research – National Institute of Immunohematology, 261 donors were identified among 1,221 regular donors, lacking a clinically significant single antigen or a combination of antigens (C, D, e, Fya, Jka and s).19 Similarly, the e antigen is expressed by nearly 98% of donors in all the studies and warm auto/allo anti-e antibodies are not uncommon in clinical practice.20 A catalogue of such single antigen-negative inventory (e-negative donors) generated by a continuous screening of donors regionwise would be a life-saving measure for those patients in need, who would otherwise have to endure an unusually long waiting time to find a compatible unit. Hence, the rarity of a blood donor of a geographical region needs to be defined depending on the population diversity, antigenic distribution and the demand for antigen-negative blood transfusion in that particular region.
Transfusion specialists should be familiar with rare antigen/phenotypes, thereby the treating physicians and the patients can be made aware of the expected delay in obtaining blood. With a data bank of these donors, a regional rare donor registry can be initiated, which would expand with a large cohort of donors from that region and contribute to the national rare donor inventory in the future.
I thank Bio-Rad, India for providing the antigen typing gel cards for carrying out this study.