The oral cavity can present the first clinical manifestations of leukemia, therefore; it is important to recognize their principal characteristics.
ObjectiveTo identify oral manifestations as the first clinical signs of leukemia.
MethodsThis is an integrative review, that gathered data from articles with oral manifestations of leukemia as part of its first clinical features. The were included case reports, case series, clinical research, or reviews with case reports. The variables that were considered relevant: age, sex, sites of the oral lesions, characteristics of the oral lesions, medical history and physical examination, time of evolution, radiographic examination, blood test results, initial diagnosis, differential diagnosis and final diagnosis.
ResultsA total of 31 studies were included, with a total of 33 individuals identified. There were 19 (57.57%) males and 14 (42.42%) females. The age range was from 1.6 to 74 years. Acute myeloid leukemia (72.72%) and acute lymphoid leukemia (18.18%) presented more oral manifestations as the first clinical signs of the disease. All individuals with leukemia presented lesions, such as ulcer, erosion, bleeding, ecchymosis, color change of the bluish or pale mucous membranes and areas of tissue necrosis. Hard tissue lesions were less frequent, being 6 (18.18%).
ConclusionThe first clinical manifestations of leukemia can be present in the oral cavity, mainly in acute myeloid leukemia. The principal oral tissues affected were gingival tissue, buccal mucosa and hard and/or soft palate. When hard tissues, such as the maxilla bone or mandible bone were affected, dental mobility was the principal clinical sign.
Leukemia is a component of oncohematological diseases. Healthy blood cells are replaced with modified immature cells in the bone marrow and circulate through the bloodstream. The classification of lymphoid or myeloid leukemia can be determined by considering the time, whether the leukemia is acute or chronic and the cell type.1,2
The worldwide incidence of leukemia is 437,033 cases, with 30,906 deaths estimated in 2019. The highest prevalence is in males, and acute and chronic leukemia mainly affect the infant/juvenile population and adult population, respectively.3
Given that leukemia is a systemic disease that affects blood components, individuals affected by this disease may present with petechiae, hematomas, ecchymosis and bleeding in different parts of the body, including the mouth, during the physical examination.4
The early identification of this disease allows individuals to start treatment as soon as possible and increases their chances of survival. Therefore, considering that the oral cavity can present the first clinical manifestations of leukemia (MOLs), its recognition from the beginning of the disease is important.5–7
In recent years, few studies have reported oral manifestations as the first clinical signs of leukemia because these manifestations are usually mentioned in clinical case reports that vary from individual to individual and with the type of leukemia.8 This integrative review aimed to identify which tissues of the mouth presented the first MOLs and describes the characteristics that allowed the guiding of the diagnosis of leukemia via clinical signs in the mouth as part of the first clinical manifestations of the disease.
Material and methodsThis study is an integrative review that gathered data from articles to describe the clinical MOLs in the oral cavity when they were present as the first clinical signs of the disease and those that contributed to guide the final diagnosis.
Structured research was performed by searching the PubMed and Scopus databases using the following terms: “(first (OR) initial OR early) AND (oral manifestation OR oral sign OR oral lesion) AND (leukemia).”
Articles published in Portuguese, English or Spanish from 2008 to 2020 were included, including case reports, case series, clinical research and reviews that included case reports. The entire publication file had to be available and had to report oral manifestations as the first clinical signs of leukemia. Animal studies, review articles, studies in other languages not mentioned in the inclusion criteria and clinical cases or research articles in which the oral manifestation of leukemia were not part of the first clinical signs of the disease were excluded.
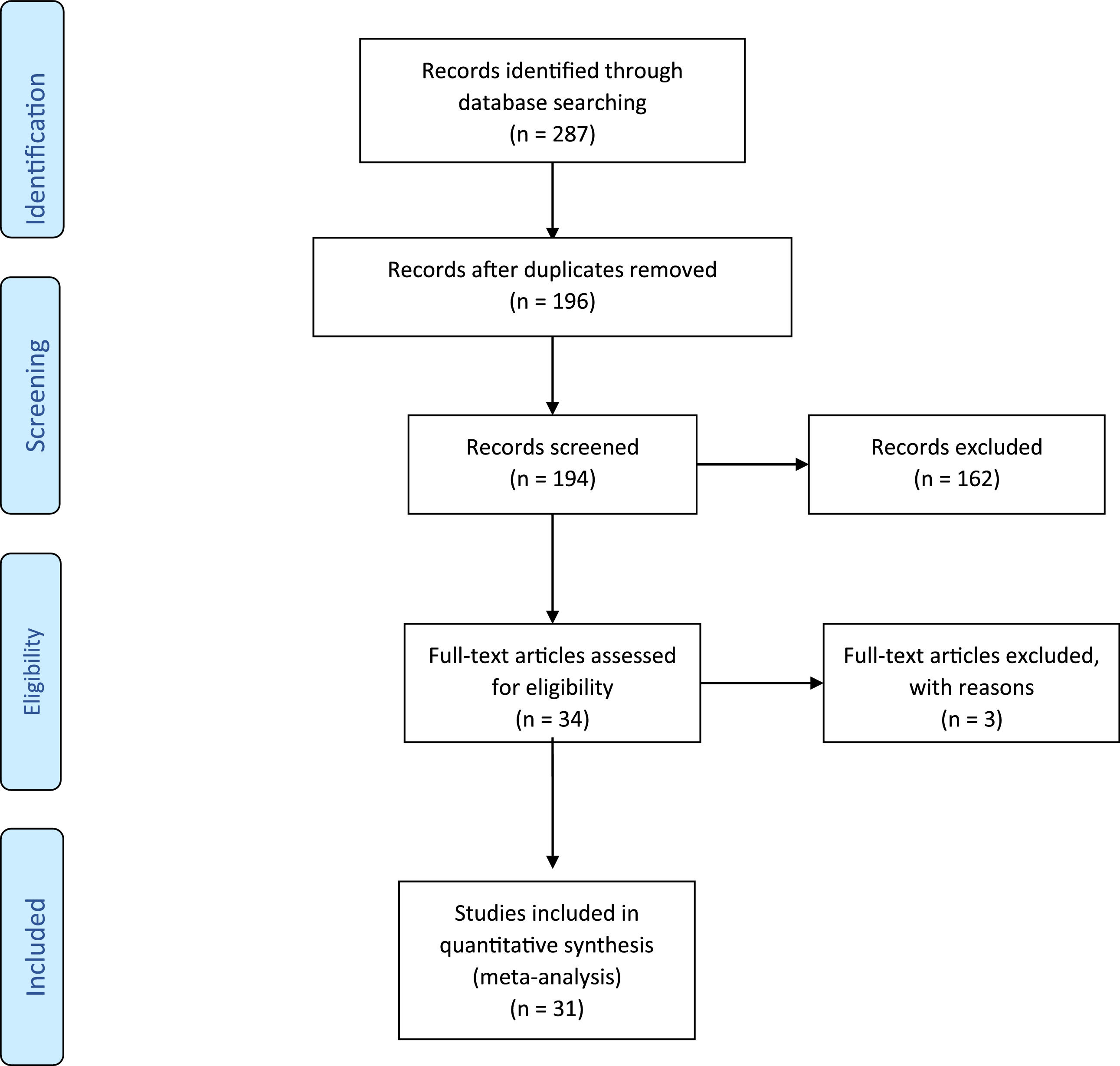
A total of 31 articles fulfilled all the pre-established inclusion criteria. All the information obtained was distributed in a table that contains the variables that were considered relevant: age, sex, sites of the oral lesions, characteristics of the oral lesions, medical history and physical examination, time of evolution, radiographic examination, blood test results, initial diagnosis, differential diagnosis and final diagnosis. (Figure 1)
ResultsA total of 31 studies that mentioned oral manifestations as part of the first clinical signs of leukemia were included. All studies included were clinical case reports or literature reviews that included at least one clinical case report with all the previously described variables.
In the case reports included in this integrative review, the evaluation and initial diagnosis of leukemia were performed principally by dentists who were the first health professionals to come into contact with the patients. Moreover, the dentists also referred the patients to the hematologist and/or oncologist to perform other analyses to establish the final diagnosis. Table 1 describes the characteristics of the 31 case reports.
Principal characteristics of individuals with oral manifestations as first clinical signs of leukemia.
A total of 33 individuals were identified in the selected studies: 19 males (57.57%)9,10,11–18,19–22 and 14 females (42.42%).23–30 The age ranged from 6 to 74 years and only 6 individuals (18.18%) were between 1.6 and 12 years old.10,19,22,26,31,32
Among the types of leukemia, oral manifestations were present principally in acute myeloid leukemia (24 individuals [72.72%]),9,12,14–19,22,23,24,25,30,32 followed by acute lymphoid leukemia (6 individuals [18.18%]),10,13,20,21,26,31 adult T-cell leukemia/lymphoma (2 individuals [6.06%]) and chronic lymphoid leukemia (1 individual [3.03%]).
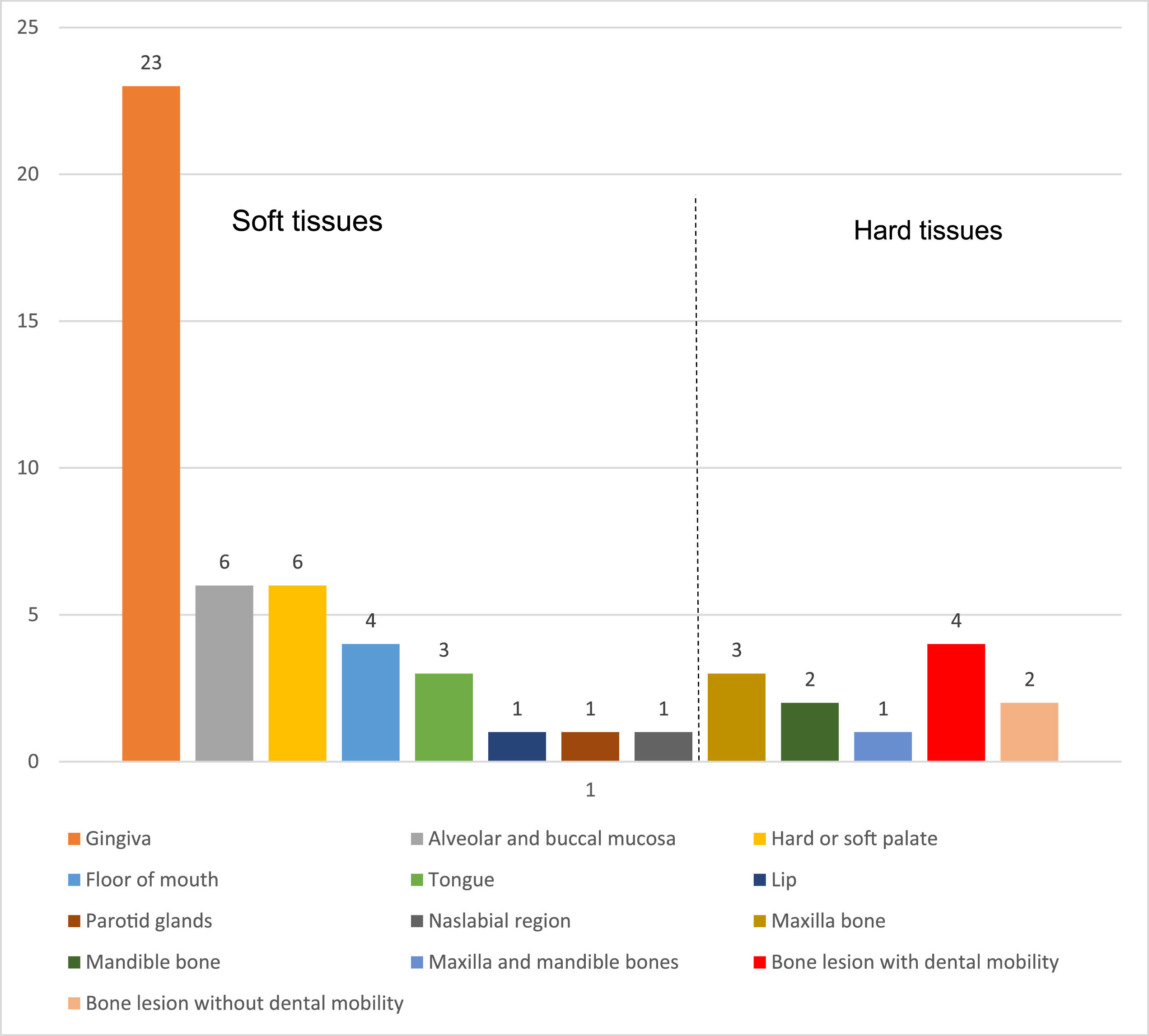
First clinical MOL in oral tissuesOral MOLs as the first clinical signs were more common in soft tissues (27 individuals [81.81%]) than those in hard tissues (6 individuals [18.18%]).11,19,20,28,31,32Figure 2 shows the different sites.
Soft tissuesThe oral MOLs were in gingival tissue (63.63%),9,12,17–19,21,23–25,26,27,30,33–39,15,40 alveolar and jugal mucosa (18.18%)14,18,21,22,26,28 and hard or soft palate (18.18%).9,11,15,16,27,30 Other regions, such as the floor of the mouth (12.12%),13,16,23,38 tongue (9.09%),13,33,39 lip (3.03%),13 parotid glands (3.03%),10 and nasolabial region (3.03%),26 were less frequent.
The main lesions found in the soft tissues of the mouth were ulcer, erosion, bleeding, ecchymosis, color change of the bluish or pale mucous membranes, and areas of tissue necrosis. Among the case reports, 13 individuals (39.99%) reported pain as the principal symptom,9,13,28,30,31,14,15,17–21,25 which was also principally spontaneous.
Hard tissuesAmong the oral MOLs in hard tissues, two cases corresponded to ALL,20,31 two cases corresponded to AML,19,32 one case corresponded to chronic lymphocytic leukemia28 and one case corresponded to adult T-cell leukemia/lymphoma.11 Dental mobility was the most common clinical condition when hard tissues were affected. Panoramic radiography and computed tomography were used to evaluate the bone structures. The main characteristics of the radiographic images were cortical expansion of the alveolar bone, osteolytic areas, thickening of the bone surrounding the teeth with mobility and severe vertical bone loss.
Differential diagnosis of the oral MOLsIn soft tissues, the differential diagnoses were gingival enlargement during pregnancy,25,35 gingival enlargement induced by drugs,41 squamous cell carcinoma and deep fungal infection,28 pericoronarite,21 oral manifestation of HIV,15,33 postoperative complications of extraction,14,36 candidiasis,27 necrotizing acute gingivitis,40 dental cyst eruption32 and herpetic gingivostomatitis.34 In addition, when the oral manifestation was in the maxillary bones, the presumptive diagnoses were acute osteomyelitis,20 osteosarcoma19,20 and Ewing sarcoma.19
General clinical signs and symptoms of leukemiaThe general signs and symptoms, in addition to the oral manifestations, were mainly the following: weakness, fatigue, lethargy or tiredness in 11 individuals (45.45%);9,12,15,17,18,20,23,26,30,36 lymphadenopathies in 8 individuals (36.36%);9,14,15,17,22,25–27 mucosal pallor in 6 individuals (27.27%);12,14,15,22,26 weight loss in 4 individuals (18.18%)15,17,23,38 and loss of appetite in 5 individuals (18.18%).9,16,23,26,32 Adjacent areas, such as the head and neck regions, presented submandibular lymphadenopathy,9,10,15,26,34 cervical lymphadenopathy,17,27,34 dysphagia,9,16,17 facial asymmetry10,26,31,37 and trismus.10,14
Other clinical signs and symptoms that were present, but were less frequent, included genital ulcers,13 vomiting,11 nausea,11,17 diarrhea,11 dizziness,17 abdominal swelling,12 petechiae in the leg and forearm,12,21 musculoskeletal pain,26 increased volume in the pre-sternal region26 and chills and joint pain.21
Results of laboratory tests that led to the presumptive diagnosis of oral MOLsThe blood count was the main blood test requested to help support the presumptive diagnosis of an oral MOL. Thrombocytopenia was present in 22 cases (59.09%),9,10,24,25,31–38,12,39,40,14,15,17,18,21–23 anemia was present in 23 cases (63.63%),9,10,25,26,31–38,12,39,40,14,15,17,20,22–24 leukocytosis was present in 19 cases (45.45%)9,11,31–40,13,15,17,18,22–25 and leukopenia was present in 5 cases (22.72%).10,12,14,19,26
DiscussionThe diagnosis of leukemia is based initially on clinical signs and symptoms that allow for the initial diagnosis of the disease. However, the definitive diagnosis is made by different complementary tests, such as karyotyping, flow cytometry and bone marrow biopsy.6,42 Early diagnosis allows the individual to start antineoplastic treatment as soon as possible, thus increasing the chance of survival and improving the prognosis.43
Before the diagnosis of leukemia, individuals can present with fatigue, fever, adenomegaly, hepatosplenomegaly, persistent or recurrent infections, hematomas, pallor, petechiae and unexpected bleeding from the skin and mucous membranes, including the oral mucosa.6,43 These symptoms and clinical signs may be similar and appear in other systemic diseases, thus hindering an early diagnosis.2 In the current review, the oral MOLs were the main complaint during examination, however, fatigue, lethargy or tiredness, lymphadenopathies, pallor, weight loss and loss of appetite were also reported, as well as the presence of dysphagia, facial asymmetry and trismus.
In this review, among the different types of leukemia with oral manifestations as the first clinical signs, acute leukemia was the most common, particularly acute myeloid leukemia; this finding is similar to that of previous studies.5,44,45 The first oral MOLs include gingival bleeding, gingival hyperplasia, ulcers and petechiae.4,5,44–46 When oral MOLs are present, it is easier for patients to identify these clinical signs because of the visibility of the mouth, compared to other body structures. All cases that were included in this review reported oral lesions as the main complaint, which was the principal reason for visiting dentists before being referred to specialists in the field of oncohematology for the final diagnosis of leukemia.
Oral MOLs can be found mainly in the gingiva, lips, hard and/or soft palate and tongue.5 In all case reports in this review, the clinical signs of leukemia in the mouth affected mainly the soft tissues. The gingival tissue had the highest manifestation9,12,26,27,30,15,17–19,21,23–25 among the types of leukemia and the mouth floor, parotid, tongue and nasolabial region10,13,16,23,26 had the lowest manifestations. Some cases reported spontaneous pain at the time of the complaint and this was one of the main reasons for seeking dental care.
In this review, it was identified that bone structures, such as the maxilla and/or mandible, had the principal features of areas with increased volume, rapid growth and dental mobility without apparent cause as part of the first clinical signs of leukemia. These characteristics led to the suspicion of malignant bone lesions, thus necessitating evaluation by imaging exams.11,19,20,28,31
Complementary imaging examinations, such as panoramic radiography and computed tomography, are essential to evaluate bone structures in greater detail. For this reason, when radiography revealed the characteristics of malignant bone lesions, the patients were referred immediately to specialists in hematology/oncology.19,20
Other dentists used the radiographs to guide the incisional biopsy, which was also useful for early referral to a specialist.28,31 Dentists can perform a biopsy if the patient agrees with the procedure. Among all the case reports of this review, one patient refused biopsy. Nevertheless, because of the malignant characteristics, the patient was immediately referred to a specialist.11 Therefore, malignant characteristics in radiography, with clinical signs and symptoms that are suspected of being oral MOLs, need to be immediately referred to a specialist in hematology/oncology, regardless of whether an oral biopsy needs to be performed.
Bone alterations as oral MOLs are rare, however, when present, they can provoke facial asymmetry, which can be the main reason for seeking dental care.31 Some bone alterations were also present in children.19,31 Therefore, bone alterations can also appear in patients who are still undergoing bone development.
The literature mentioned that children and adolescents with leukemia, who are undergoing bone development and bone maturation, respectively, had bone areas with osteotropic characteristics that can promote the local invasion of malignant cells into bone structures, thus provoking their destruction.47,48
Moreover, hypercalcemia was found in adult patients with bone MOLs.11,36 One of the clinical reports in this review mentioned that hypercalcemia was associated with the ectopic production of the parathyroid hormone protein, in addition to a severe increase in alkaline phosphatase levels.11 Oral manifestations in bone structures as the first clinical signs of leukemia are considered extremely rare, however, after chemotherapy, the bone lesions can regress and the follow-up can be performed via radiography examination.11,19,20,28,31
The diagnosis of leukemia can be challenging and complex, particularly when the oral MOLs have characteristics similar to those of other systemic diseases and specific oral diseases. In this review, 11 cases of oral MOLs were initially confused with other lesions that presented clinical signs and symptoms that are identical to those of some oral diseases.14,15,35,36,19–21,25,27,28,32,33
For example, a case report included in this review mentioned pericoronitis as an initial diagnosis, which is characterized by inflammation, pain, trismus and sometimes, infection associated with the periodontitis eruption of the third molar tooth.21 The oral MOL in this case presented characteristics that initially mimicked the oral MOL. Therefore, the referral to the hematologist was delayed. Another case report in which the final diagnosis was leukemia had pregnancy gingivitis or hyperplasia as the first diagnosis.25 Some pregnant patients with relative frequency may present with changes in the gingival tissue, such as gingivitis. Therefore, considering that the patient was pregnant, the initial diagnosis coincided with the clinical condition of the patient.
Complementary tests, such as the complete blood count, were essential in establishing the initial diagnosis based on the first oral MOL. In this review, a blood count was requested for all patients and this approach allowed for the immediate referral to specialists in hematology/oncology. The main alterations were leukocytosis, thrombocytopenia, anemia and the presence of blasts in the blood count, which was essential and useful, not only in diagnosing leukemia, but also in evaluating the prognosis and guiding the treatment of the patient. An early diagnosis of leukemia corresponds to a high chance of survival.
This integrative review included data from patients of different ages and therefore, we did not analyze the data by age group. This was a limitation because there is a possibility of finding specific first clinical signs of leukemia in the oral cavity of children, young people and the elderly.
ConclusionsLeukemia may present with oral manifestations as part of its first clinical signs. Acute leukemia was the type with the most oral manifestations, particularly acute myeloid leukemia. The anatomical structures most affected in the oral cavity were the gingival tissue, jugal mucosa and hard or soft palate. When oral MOLs were present in hard tissues, such as the maxilla or mandible, dental mobility was the main clinical characteristic. The main complementary test to help formulate the initial diagnosis of leukemia and referral to specialists, such as a hematologist and/or oncologist, was the complete blood count, which can identify leukocytosis, anemia, and thrombocytopenia.
FundingThis study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.