Diversity in Classical Hematology Research
More infoHodgkin lymphomas are lymphoid neoplasms with large mononuclear and multinucleated neoplastic cells- Reed Sternberg cells (RS cells) surrounded by lymphoid and non-lymphoid inflammatory cells. They are classified into Classical Hodgkin lymphoma (CHL) and nodular lymphocytic predominant Hodgkin lymphoma (NLPHL), with CHL further subdivided into 4 categories- lymphocyte rich, nodular sclerosis, mixed cellularity and lymphocyte depleted (LDHL), each having different microscopic features.1 It is a well-researched and understood entity and considered a fairly easy diagnosis to make even on Hematoxylin and eosin slides. However, Hodgkin lymphomas can also present with varied microscopic and clinical features rarely described in the literature, resulting in a diagnostic dilemma.2-4 Here, we report an interesting case of Classical Hodgkin lymphoma with different microscopic findings.
Case reportA 44-year-old male presented to the emergency department with progressive breathlessness for fifteen days and disorientation for one day. There was a history of gradually progressive painless lymphadenopathy of insidious onset in the cervical and axillary region. History of intermittent fever and productive cough with whitish sputum was also present with significant weight loss during the previous year. There was no history of night sweats or loss of appetite. The patient was started on Anti tubercular therapy (ATT) 4 months back, which he took for 3 months and discontinued after that. However, the patient did not have any test results indicating a diagnosis of tuberculosis.
The patient was admitted to the Intensive care unit following intubation and was on noradrenaline infusion. Chest x-ray showed pleural effusion and right upper lobe collapse. A computed tomography (CT) scan of the thorax and abdomen revealed a neoplastic mediastinal mass measuring 12*17*22cm encasing the heart, aortic arch, proximal descending aorta, pulmonary trunk and other major vessels without luminal obstruction. Narrowed right upper main bronchus due to external compression by the mass was seen on bronchoscopy. A cartridge-based nucleic acid amplification test (CBNAAT) from the pleural fluid was negative. An axillary lymph node excision biopsy was done. Mediastinal biopsy was not done. The next day the patient suffered a hypoxic arrest and expired. Autopsy was not performed.
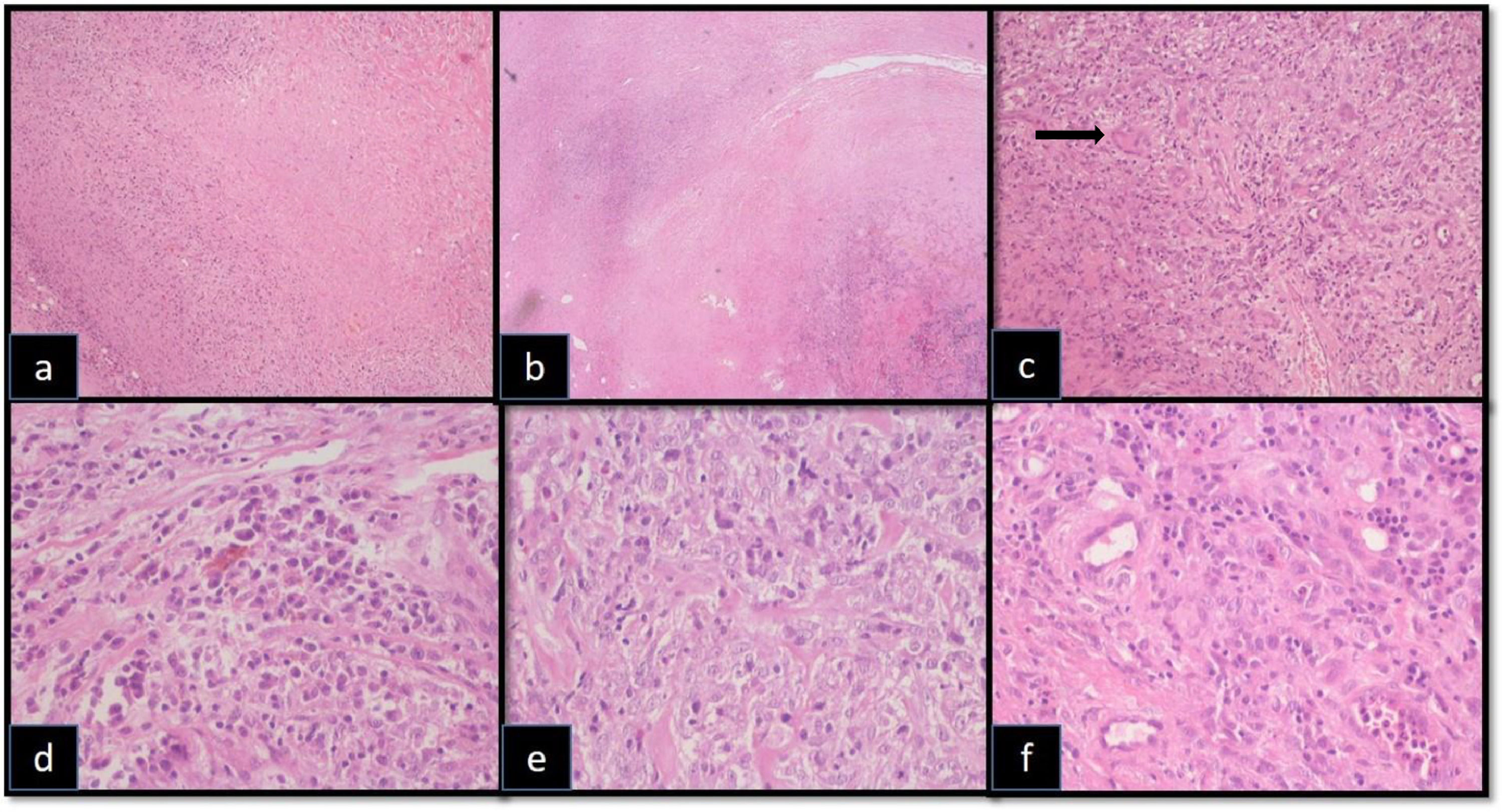
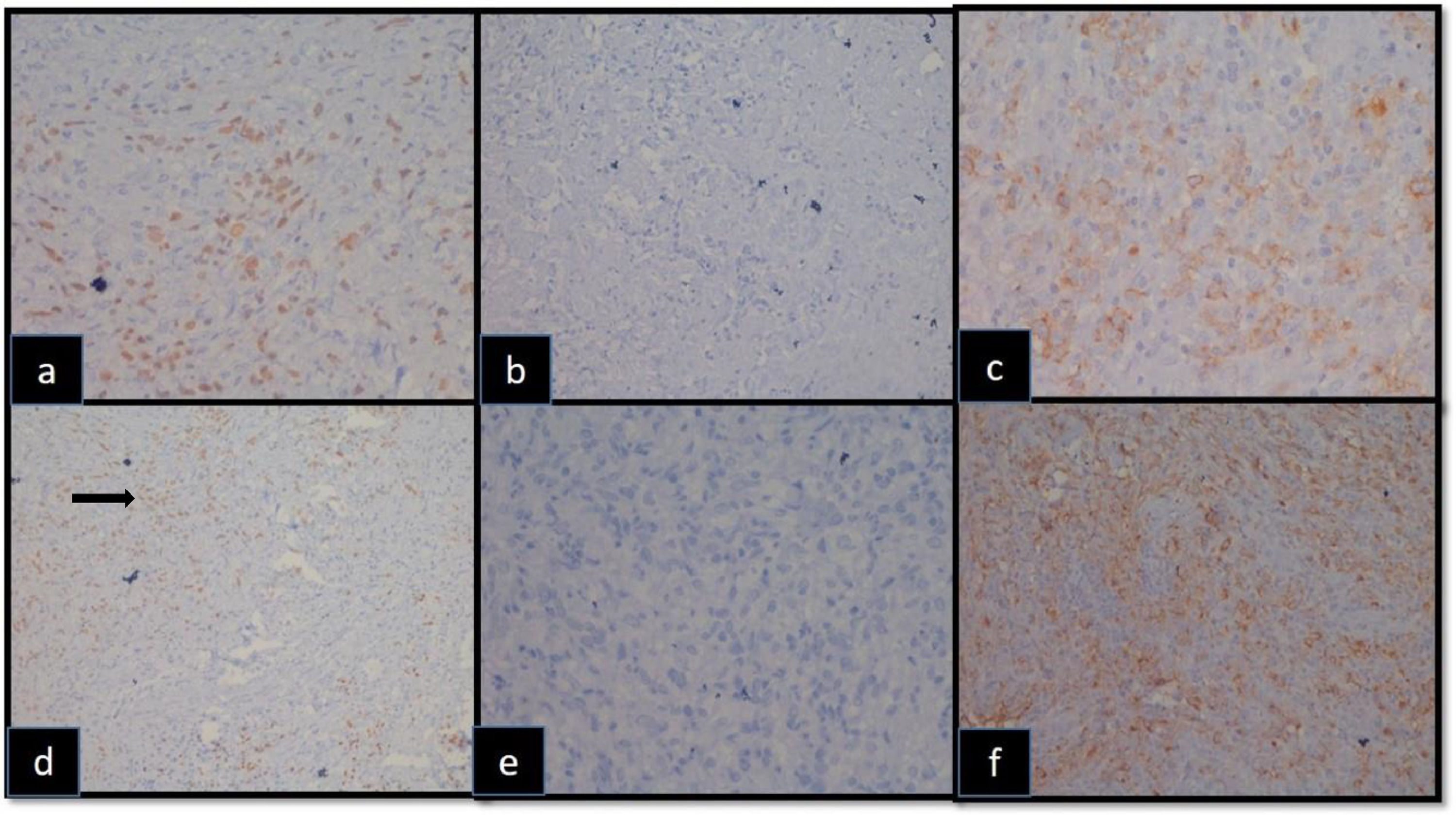
The lymph node excision biopsy showed lymph node tissue with diffuse effacement of the nodal architecture by ill-defined necrotising epithelioid cell granulomas and extensive fibrosis was present along with lymphocytes, plasma cells and histiocytes. Lymphoid follicles were not retained (Figure 1). With these features, the very first possibilities we considered were infective etiology or a malignancy. Special stains- Ziehl Neelsen, Per-iodic acid Schiff and Gomori Methanamine silver stains were done, which did not reveal any organisms. We re-examined the slides and decided to do an initial immunohistochemistry (IHC) panel of CD30, CD68 and PanCK as there were many large cells, which we initially considered as macrophages. These cells were large with vesicular chromatin, prominent nucleoli and moderate amounts of cytoplasm. There were no typical RS cells. On IHC, these cells were negative for PanCK and positive for CD30 in a background of many macrophages that were CD68 positive. Further IHC staining for CD20, CD7, ALK, CD5, EBV-LMP and Pax-5 were performed. These highlighted the large cells to be positive for CD20 with dim Pax-5 positivity and negative for CD7, CD5, ALK and EBV-LMP (Figure 2), which led to the diagnosis of Hodgkin lymphoma.
Effacement of lymphoid architecture by (a) ill defined necrotising granulomas (100 X, H and E (b) and large areas of fibrotic bands (40 X, Hand E). (c) Langhans giant cells (→) admixed with inflammatory cells (200 X, Hand E) and (d) numerous plasma cells (400X, H and E). (e) Large atypical cells with prominent nucleoli, vesicular chromatin and moderate cytoplasm (400 X, Hand E), (f) admixed with many macrophages (400 X, Hand E).
Hodgkin lymphoma is a monoclonal lymphoid neoplasm with the tumor cells accounting for 0.1 to 10% of the whole population, with the rest being lymphoid and non-lymphoid inflammatory cells.1 Even though not classically described, there are many reports of similar cases with presence of granulomas in Hodgkin lymphoma, both necrotising and non-necrotising ones, resulting in a diagnostic dilemma.2,3,5 Studies have mentioned that incidence of caseating granuloma in HL is around 9%; however, that of necrotising granuloma is much lower, around 1.8%.2,3 There is no clear explanation for the formation of granulomas in Hodgkin lymphoma in the literature. T cell mediated immune response against the tumor cells, tumor antigen stimulation causing fibrosis followed by granuloma formation and delayed hypersensitivity to decomposition products of the tumor cells are some of the considered theories.6-8
The diagnosis of Hodgkin lymphoma was difficult in this case due to the atypical morphologic features on presentation. The presence of necrosis and epithelioid granulomas and absence of typical RS cells led us to consider an infective etiology in the first place. We had also considered the possibility of coexisting TB and HL, but the negative CBNAAT report was not in favour of this. Also, the patient had taken ATT for 3 months, after which the granulomas should have been cleared, had it been because of TB. The case showed very few background lymphoid cells, hence ruling out a diagnosis of NLPHL, lymphocyte rich CHL, and mixed cellularity type CHL. Even though presence of fibrous bands were seen, there was no nodule formation, unlike nodular sclerosis cases. The fibrous bands were thick, and not fibroblast-rich as seen in lymphocyte depleted CHL. Presence of many plasma cells ruled out LDHL.1 The polymorphous population of cells, dim Pax-5 positivity by tumor cells and absence of diffuse CD20 positivity ruled out the possibility of other lymphomas like Primary mediastinal large B cell lymphoma and B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and classic Hodgkin lymphoma.9,10 The absence of a typical morphological feature of any of the subtypes of Hodgkin lymphoma had caused a diagnostic dilemma on morphology till the immunohistochemistry was performed.
Hodgkin lymphoma has a good prognosis with 85% 5-year survival rate if the current treatment protocols are followed.1 The patient mentioned here expired even before the diagnosis was made. The patient, even though he was symptomatic for a duration of at least 1 year, did not present himself to the hospital till he developed breathlessness. Additionally, studies have showed that granulomatous Hodgkin lymphomas and cases with increased macrophages are associated with poorer prognosis as seen in our case.1,2
ConclusionDue to the presence of ill formed necrotising granulomas and abundant fibrosis in addition to the absence of typical RS cells, a diagnosis of Hodgkin lymphoma was not initially considered in this case. Diagnosing this case as HL exclusively on morphology would not have been possible. With this case report, we proposed to highlight the existence of a granulomatous reaction in Hodgkin lymphomas and the importance of ancillary studies in similar situations.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.