Cancers of different cellular composition and distinct sites of origin are unquestionably separate primaries, which can be temporally diagnosed near to each other or at different times.1
The prevalence of multiple primary malignant neoplasms seems to vary from 0.734% to 11.7%.2 Typically, a patient with a first cancer who develops a second one will do so over time with the presentation of a patient with concurrent primary tumors of distinct histology in separate organ systems being quite unusual.3,4 Recognizing such tumors, however, is important not only for prognostic purposes, but, more importantly, for therapeutic interventions.
Herein, we report on a case of a male patient diagnosed with gastric mucosa-associated lymphoid tissue (MALT) lymphoma simultaneously to the diagnoses of colon granular cell tumors and metastatic lung cancer.
Case reportA previously healthy 56-year-old male patient presented with right posterior chest pain and cough. He was a 63 pack-year active smoker, had had gastric surgery for peptic ulcer disease 20 years previously and was allergic to penicillin. His family history was positive for two cases of cancer; his father had died from lung cancer, and a cousin had died from breast cancer.
The initial chest X-ray showed middle lobe opacity and a small nodule in the upper right lobe. Chemistry panel on presentation was unremarkable except for an albumin level of 3.5g/dL, corrected calcium of 10.8mg/dL and gamma-glutamyl transferase of 97IU/L. Complete blood count was normal except for a hematocrit of 55.6%. Computed tomography (CT) of chest and abdomen revealed lesions in the right lung suggestive of malignancy, a lytic lesion with pathologic fracture of the right sixth rib, thickening of the gastric wall, and signs of emphysema. There were no lymphadenopathies or other masses. CT scan findings were not definitive for a primary lung cancer versus secondary pulmonary metastases, and a bronchoscopy was ordered, but it did not show any bronchial abnormality.
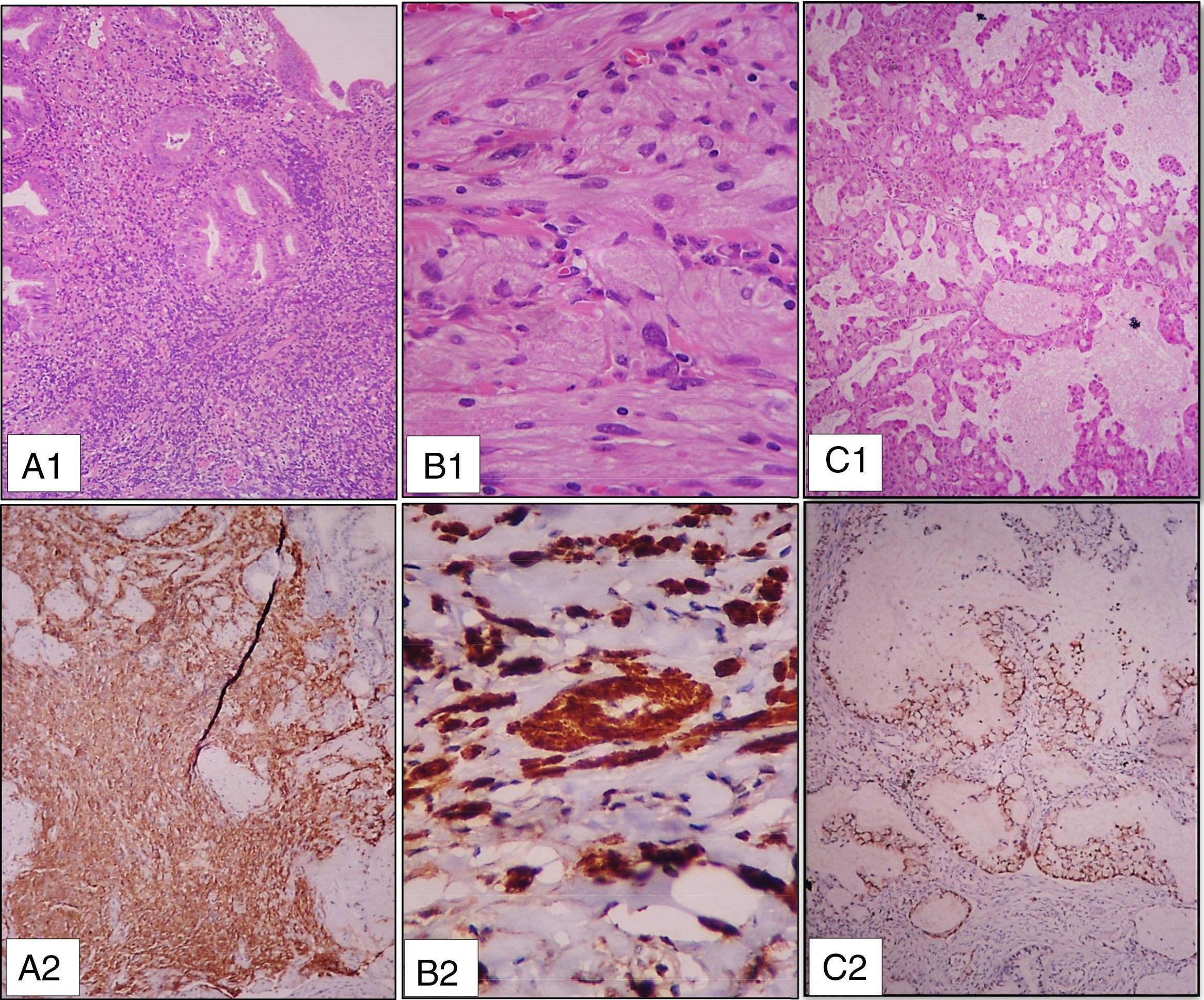
Upper endoscopy was performed, revealing several small shallow gastric ulcers of up to 20mm. Histopathology examination and immunohistochemistry (CD3+, CD20+, bcl-2+, CD43+, CD10+, Ki67 10–25%) of gastric biopsies diagnosed extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) (Figure 1A). Both rapid urease test and gastric histology were negative for H. pylori, but serology (IgM and IgG) was positive. Other serologies (human immunodeficiency virus, hepatitis B, hepatitis C) were negative.
(A) Histologic features of the gastric biopsy: A1 – Gastric mucosa with extensive atypical lymphoid infiltration [hematoxylin and eosin (H&E) – 100×]; A2 – Diffuse reactivity for CD20 – 100×; (B) Histologic features of colon polyps: B1 – Granular cell tumor (H&E – 400×); B2 - Strong and diffuse reactivity for S100 – 400×; (C) Histologic features of lung lesions: C1 – Lung mucinous adenocarcinoma (H&E – 100×); C2 – Positive reactivity for TTF1 – 100×.
As part of the initial evaluation, the patient also underwent a colonoscopy, which showed two polyps of up to 7mm in the ascending colon. They were both excised endoscopically with free margins and were diagnosed as granular cell tumors (S100+, CD117−, Dog1−, CD34−, smooth muscle actin-, Ki67 <5%) (Figure 1B).
A right lung segmentectomy with sampling of the pleura and lymph nodes was then performed. Hematoxylin and eosin (H&E) sections and immunohistochemistry (Ck7+, Ck20−, TTF1+, PSA−) were consistent with primary lung mucinous adenocarcinoma (Figure 1C) involving the lung parenchyma, pleura and mediastinal nodes. Epidermal growth factor receptor (EGFR) gene mutations were not identified in the tumor. The brain was free from metastasis on magnetic resonance imaging, but additional bone metastases were found in a bone scan. Bone marrow smear and biopsy were normal, with no malignant infiltration.
The patient was assumed to have EGFR-negative lung adenocarcinoma with bone and pulmonary metastases (stage T4N2M1b – American Joint Committee on Cancer Staging Manual 7th edition), stomach confined MALT lymphoma (stage IE – American Joint Committee on Cancer Staging Manual 7th edition), and colonic granular cell tumors. He was treated with a full course of omeprazole and antibiotics (metronidazole and clarithromycin), and started chemotherapy with paclitaxel 200mg/m2 D1, carboplatin AUC6 D1, and bevacizumab 15mg/kg Day 1 every 21 days, plus zoledronic acid. Three cycles of chemotherapy were delivered. Post-antibiotic upper endoscopy was performed showing resolution of mucosal abnormalities and histologic remission of the lymphoma and the H. pylori fecal antigen became negative. Re-staging CT scans, however, showed progressive bone and visceral disease. Second-line chemotherapy with pemetrexed 500mg/m2 every 21 days was offered, but proved to be ineffective and the patient eventually died from progressive metastatic lung cancer eight months after the diagnosis of his simultaneous multiple neoplasms.
DiscussionAlthough authors use different criteria to characterize cases of multiple primary tumors, they can be defined as two or more independent primary reportable neoplasms, arising as lesions in the same or separate organs/anatomical portions of the body of an individual.5 A cancer of different cellular composition and distinct site of origin than the original tumor is a separate primary, as well as cancers of different histologic types in the same site.1
The distinct histologies may be identified simultaneously or at different times, as synchronous or metachronous tumors. The time framework to call a tumor synchronous or metachronous is variably established. While some authors state that synchronous tumors occur within two months of each other, and a metachronous tumor occurs more than two months after the initial cancer diagnosis,6 others would classify malignancies as synchronous if the interval between their diagnoses is less than or equal to six months, and metachronous when tumors occur more than six months apart.2,7,8
A literature review of 1,104,269 cancer patients found the prevalence of multiple primary malignant neoplasms to vary between 0.734% and 11.7%.2 More recently, it was observed that 14% of patients diagnosed with a first primary cancer developed a second cancer on extended follow-up with a cumulative incidence of 5.0%, 8.4%, 10.8% and 13.7% at 5, 10, 15, and 25 years, respectively. The highest overall frequency of second cancers was among those diagnosed between 50 and 69 years of age.9
Typically, a patient diagnosed with a first cancer that develops a second one will do so over time. There is limited data on cases of multiple synchronous tumors in one patient; the information available comes mainly from case reports.8 The association of a hematological malignancy with solid tumors may pose particular diagnostic and therapeutic challenges.3 The patient reported herein, however, was diagnosed simultaneously with gastric MALT lymphoma, colon granular cell tumor and metastatic lung cancer, with the microscopic confirmation of each neoplasm occurring within eight days.
Multiple primary cancers may be determined by three principal and non-mutually exclusive factors: shared etiologic exposure, familial cancer syndromes or other genetic susceptibility factors, and prior cancer treatment.10 With the exception of a positive family history – in one series, 32% of multiple primary cancer patients had a family history of oncologic diseases7 – our patient had none of these factors. Tobacco use is one of the major causes of multiple primary cancers, but it is mostly associated with tumors of the lungs and upper aerodigestive tract,10 and H. pylori seropositivity does not appear to be associated with lung cancer.
Despite receiving standard treatment for his multiple primaries at the time, our patient had an aggressive clinical course, succumbing to uncontrolled metastatic lung cancer. In fact, the prognosis of patients with multiple synchronous primaries will be determined by the biology and stage of each cancer. Advanced tumors at presentation will likely be associated with a poor outcome.3
The occurrence of multiple primaries, such as the case reported here of gastric non-Hodgkin MALT lymphoma, granular cell tumor of colon and lung adenocarcinoma, is not only uncommon, but also may result in management dilemmas, requiring that simultaneous treatment of each cancer be delivered cautiously because of toxicity and tolerance concerns; prognostic considerations should be taken into account to prioritize the most virulent tumor.3
The incidence of concurrent tumors may be expected to rise as a result of improved sensitivity and widespread use of screening and staging methods. Lesions not compatible with the anticipated metastatic pattern of a given malignancy, nonparallel response of separate lesions to a certain treatment, and heterogeneous control of symptoms from different lesions while treating a single tumor are all scenarios that should bring to mind the possibility of synchronous multiple tumors,3 with the attendant need of histologic sampling and adequate treatment planning.
Conflicts of interestThe authors declare no conflicts of interest.


![(A) Histologic features of the gastric biopsy: A1 – Gastric mucosa with extensive atypical lymphoid infiltration [hematoxylin and eosin (H&E) – 100×]; A2 – Diffuse reactivity for CD20 – 100×; (B) Histologic features of colon polyps: B1 – Granular cell tumor (H&E – 400×); B2 - Strong and diffuse reactivity for S100 – 400×; (C) Histologic features of lung lesions: C1 – Lung mucinous adenocarcinoma (H&E – 100×); C2 – Positive reactivity for TTF1 – 100×. (A) Histologic features of the gastric biopsy: A1 – Gastric mucosa with extensive atypical lymphoid infiltration [hematoxylin and eosin (H&E) – 100×]; A2 – Diffuse reactivity for CD20 – 100×; (B) Histologic features of colon polyps: B1 – Granular cell tumor (H&E – 400×); B2 - Strong and diffuse reactivity for S100 – 400×; (C) Histologic features of lung lesions: C1 – Lung mucinous adenocarcinoma (H&E – 100×); C2 – Positive reactivity for TTF1 – 100×.](https://static.elsevier.es/multimedia/25311379/0000004000000002/v1_201805170435/S2531137918300063/v1_201805170435/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w93OM6WmS6o9DeZl+SVh74uo=)



