We report here on a rare case of primary conjunctival Follicular Lymphoma grade 3B (FL3B). The objective of this report is to discuss the best conduct to be adopted for a localized lymphoma with an exceptional ocular presentation in a young patient.
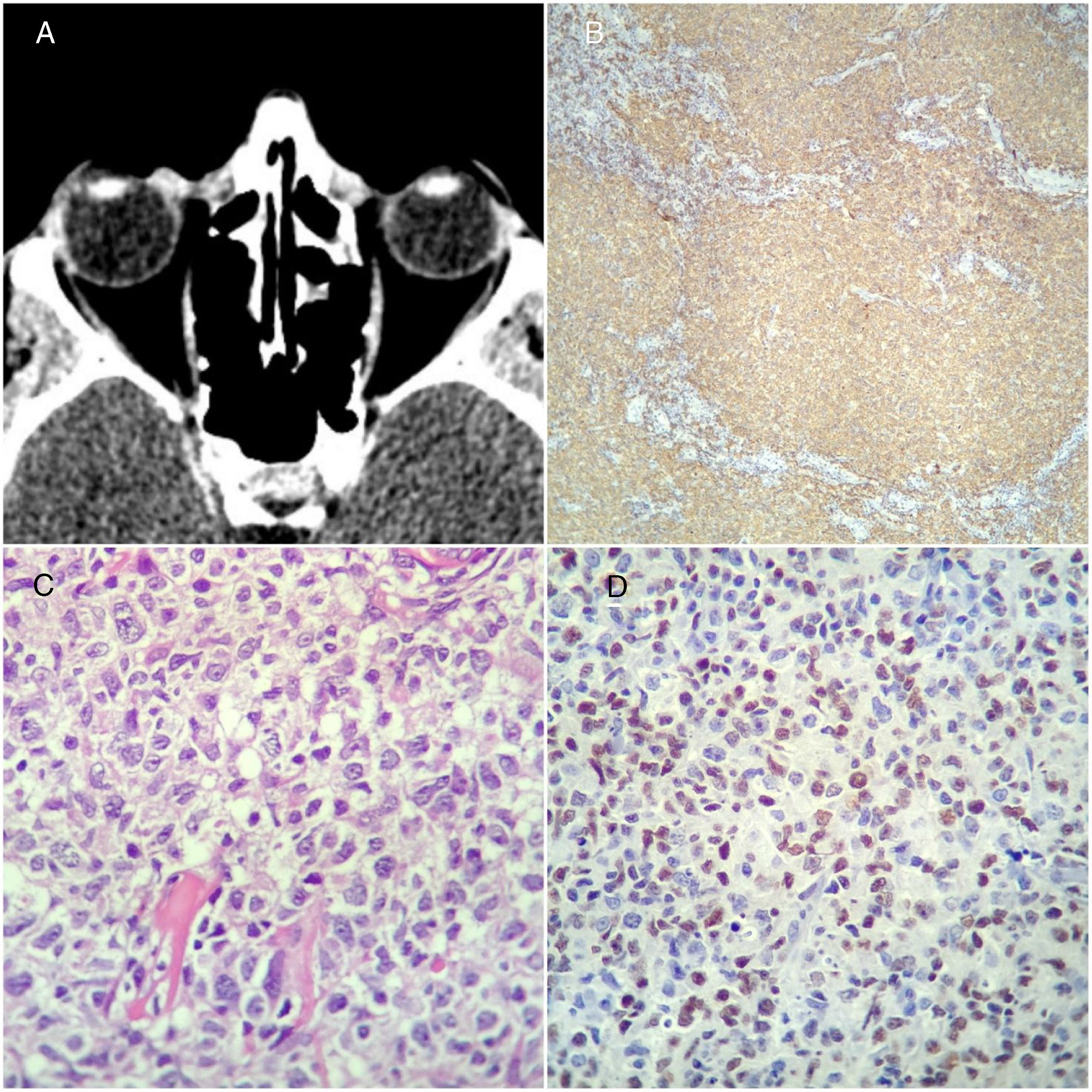
Case reportThe patient, a 31-year-old male, reported the emergence and rapid growth (within three months) of a tumor-like conjunctival lesion in his right eye. His only complaint was a discomfort when turning his eye to the right. He denied having either B symptoms or pain (Figure 1). He was evaluated by an ophthalmologist, who excised the tumor. Following the excision biopsy report: FL3B, he was referred to a hematologist. We started his follow-up five months after surgery. He was asymptomatic, denied having any visual alterations, arising of adenomegalies, or B symptoms. There was no physical alteration, whether general or specifically ophthalmological. No laboratory test result presented an alteration of clinical significance. In addition, cerebrospinal fluid testing was negative for oncotic cytology, and serum results for hepatitis B, hepatitis C and HIV were negative as well. We performed positron emission tomography and nuclear magnetic resonance of the skull and orbit, none of which revealed any measurable lesion.
Thus, according to the Lugano 2014 staging and the American Joint Committee on Cancer (AJCC TNM) 8th Edition Classification of Conjunctival Carcinoma, the tumor was classified as IEA and T1, respectively, and considered low-risk with regard to the Follicular Lymphoma Prognosis Index (FLIPI).
A histopathological review performed by hematopathologists showed conjunctival mucosa harboring, in the superficial and deep chorion, a dense lymphoid infiltrate forming a tumor area up to 0.5cm thick in the analyzed sample, consisting of large lymphoid cells with morphological characteristics of centroblasts. Among these large cells, there were a few smaller cells, with characteristics of centrocytes. We observed a follicular growth pattern, sometimes with confluent boundaries, but without characterizing clearly diffuse areas. This lymphoid proliferation showed the following immunohistochemical profile: CD20+; CD10−; BCL2+, CD23+MUM-1−, BCL6+, KI67 50%. These findings confirm the diagnosis of grade 3B follicular B-cell lymphoma (Figure 1).
We chose to treat the patient with four cycles of rituximab 375mg/m2/day1; cyclophosphamide 750mg/m2/day1; doxurubicin 50mg/m2/day1; vincristine 1.4mg/m2/day1 and prednisolone 100mg days 1–5 every 21 days (R-CHOP-21); and four intrathecal methotrexate 12mg plus dexameathasone 2mg injections as prophylaxis against an infiltration of the central nervous system. He is progressing without any intercurrence, maintaining the absence of measurable disease after the treatment.
Figure 1A: computerized tomography of the orbit, showing a conjunctival tumor in the right eye prior to excision; B: dense lymphoid proliferation of B cells forming poorly defined follicular areas in the conjunctival mucosa (CD20). C: detail of the cellular composition, with predominance of large cells with characteristics of centroblasts (HE). D: nuclear positivity for BCL6 in lymphoid cells.
DiscussionTumors of the ocular conjunctiva may be benign, pre-neoplastic or neoplastic. In a series of 5002 adult patients with conjunctival tumors, about 30% were neoplasms and 7% (358) were diagnosed as lymphoma.1 In a study on 268 cases of conjunctival tumors, we found the following frequencies: 68% of extranodal marginal zone lymphoma of the MALT type, 16% of follicular lymphoma (FL), 7% of mantle-cell lymphoma, and 5% of diffuse large B-cell lymphoma (DLBCL). It has been observed that 31% of conjunctival lymphoma cases have a systemic presentation. Among the FL cases, the mean age was 67 (33–89) years, and 62.8% presented unilateral tumors. About 65.1% of the cases presented EC: IEA and 67.9% T1 on the AJCC TNM staging scale.2 Out of 98 cases from a study that analyzed FL infiltrating ocular annexes, 70% were primary affections. The conjunctiva was affected in 29% of the cases, followed by the orbits (26%) and lacrimal glands (26%). Among the 69 cases of primary FL, 35% presented AJCC TNM T1 staging, 52% T2, and 13% T3 and T4. The age median was 63 years. Out of the 98 cases, 81% had grade 1 or 2 FL, 17 (17.3%) had FL grade 3A, and a single case had FL3B. It is striking how rare the case reported here is, considering that in a reference ophthalmology center a single FL3B case was found in 30 years (1980–2010).3
FL represents about 20% of all non-Hodgkin lymphomas and is classified into subtypes, according to the presence of centroblasts and morphology, as grades 1, 2, 3A, and 3B. The differences considered in the pathologic anatomical, immunohistochemical and molecular diagnosis of FL3B are: a diffuse pattern of centroblasts, decreased expression of CD10, expression of MUM-1 and low frequency of the translocation involving BCL-2,4 besides an increase of cytogenetic alterations affecting the gene BCL-6. As in the present case, some FLs may not have CD10 expression, but BCL6 expression is present. This atypical phenotype FL, defined by the absence of CD10 and/or BCL-2 expression, was studied and it was observed that the majority of atypical cases presented loss of BCL-2 and CD10+ when compared to CD10-/BCL2+ and CD10-/BCL-2−; 48.4%, 39.4% and 12.2%, respectively.5
The incidence of FL3B among FLs is less than 10%, and there are few studies comparing the incidence of grade 3A and grade FL3B. A few studies compared the treatment of these two diseases and showed a 2 to 3:1 relation, respectively.6,7 Compared to grade 1 and 2 FL, FL3B tends to present a lower frequency of advanced disease: 65–70% versus 70–85%, respectively.8
Although there are some variants of FL such as: pediatric-type FL grade 3A and 3B; primary cutaneous follicle center lymphoma and primary duodenal FL with indolent course, we considered the prognosis of this localized conjunctival to be poor, due to the relapse rate found in the largest series of FL cases. Approximately 91% of the cases were treated with R-CHOP and radiotherapy (RDT). The progression-free survival (PFS) median was 5.3 years. The overall survival (OS) rate after 10 and 20 years was 69% and 29%, respectively.3
Concerning conjunctival lymphomas, the main treatment in 91.7% of the cases was radiotherapy with or without chemotherapy (the most commonly used protocol being R-CHOP). FL relapsed in 42.9% of the cases, the PFS median was 6.7 years, and the OS rate after 5 and 10 years was 75% and 59%, respectively. As for the patients with DLBCL, relapses were reported in 66.7% of the cases, the PFS median was 3.5 years, and the OS rate after 5 and 10 years was 55 and 39%, respectively. Although the treatment in this study was not uniform in the different lymphoma subtypes, it was evident, however, that DLBCL presents the poorest prognosis, as compared to FL.2 Therefore, we have no evidence for considering this localized conjunctival FL3B as having an indolent course, because of its extremely rare presentation,3 and because it was confirmed that distinct subtypes of localized conjunctival lymphoma have a different prognosis.2
The fact that the patient is currently asymptomatic and that his disease is not measurable brings about a therapeutic dilemma, for there are no clear rules regarding the exclusive observation of such cases. This becomes evident by reviewing the main studies on phase III FL in symptomatic patients, which exclude LF3B, as well as in asymptomatic patients in which observation is a comparing arm.9 This helped us to decide not just to watch-and-wait. A retrospective study on 505 FL patients clearly revealed different prognoses between FL grade 3A and FL3B patients, with OS medians of 12.2 and 4.4 years, respectively.10 It is therefore understood that FL3B must be seen as an aggressive lymphoma that needs treatment with anthracycline and rituximab, just like DLBCL, despite the fact that all classic phase III studies excluded FL3B cases. Therefore, we made our choice based on risk (ocular sequels from radiotherapy) in a young patient versus effectiveness (little scientific evidence in the absence of measurable disease) and administered exclusively four R-CHOP-21 cycles with intrathecal Methotrexate prophylaxis.
In summary, this report shows an uncommon case of FL3B with an unusual presentation. Thus, we must point out that, since we have no clinical data to support the adoption of one standard protocol, the challenge to be faced in real life is choosing the best possible treatment for our patient.
Conflicts of interestThe authors declare no conflicts of interest.