The occurrence of two or more simultaneous or successive malignancies, in the same patient is a rare clinical entity called primary multiple malignant neoplasia. In such an event, the association of two solid tumors, or two onco-hematological disorders, is usual; however, the association between a solid malignancy with a hematological neoplasm is even rarer.1
The liposarcoma is one of the most common soft parts sarcoma, corresponding to 20% of sarcoma in adults, whose genesis is in the differentiation of the primitive mesenchymal cells.1 The World Health Organization recognizes four subtypes: well-differentiated liposarcoma (or atypical lipomatous tumor), myxoid liposarcoma, pleomorphic and undifferentiated. Each type presents specific features.2,3
Multiple myeloma is a hematologic malignancy characterized by the plasma cell clonal proliferation in the bone marrow, hematopoietic suppression, renal dysfunction and osteolytic injury.4 The literature has described the association of other neoplasias prior to, or synchronously with, the diagnosis of multiple myeloma, in the same manner as subsequently to the course of the disease.4,5 However, the synchronous association between liposarcoma and multiple myeloma is a rare clinical entity.
This study aims at describing a synchronous case of a well-differentiated liposarcoma and multiple myeloma in a young female patient.
Case reportA 42-year-old black woman was admitted to the Oncology Service with anemia (hemoglobin 8.1g/l), a monoclonal peak in the gamma globulin region (γ 58.5%) upon serum protein electrophoresis and the presence of the IgG Kappa monoclonal protein in serum protein immunofixation. The diagnosis of multiple myeloma was confirmed by bone marrow aspirate, as it revealed lymphoplamocitary infiltration, representing 26% of global cellularity.
During diagnosis, the ultrasound exam presented a well-enclosed 14cm diameter abdominal mass complex in the right iliac fossa, which was painless to deep palpation during the physical examination, being presumed at that time as an extramedullary manifestation of the underlying disease. Chemotherapy treatment was initiated with a cyclophosphamide, dexamethasone and thalidomide protocol.
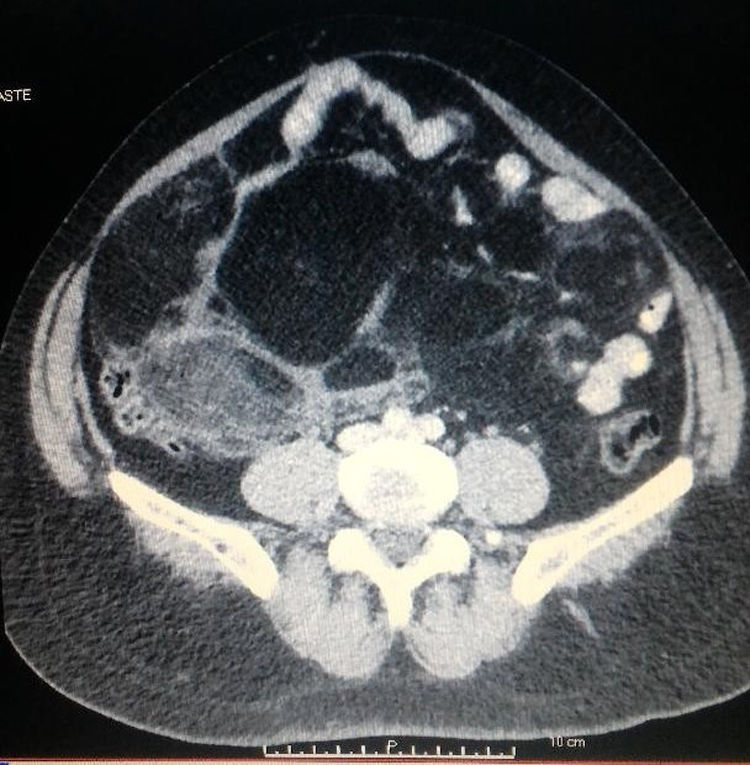
Over 8 months, the patient evolved with partial response to the therapy; however, there was a progressive abdomen increase associated with the development of intestinal constipation, nausea, hyporexia and feeling of early satiety. The computed tomography elucidated the presence of a fat-density heterogeneous mass measuring 17×13cm in the iliac fossa (Fig. 1).
The patient underwent laparotomy with incisional biopsy. The immunohistochemical study of the material revealed the expression for the p16, MDM2, CDK4 and S-100 protein, consistent with the atypical Lipomatous Tumor Well-differentiated Liposarcoma.
Under oncological evaluation, she was simultaneously subjected to three cycles of chemotherapy with ifosfamide and cytoreductive doxorubicin and to hematological treatment with four cycles of the bortezomib and dexamethasone protocol. At the end, there was a disappearance of the monoclonal protein in serum and the urinary immunofixation protein, as well as 4% of bone marrow plasma cells in the complete response of multiple myeloma. Moreover, the abdomen CT showed reduction of mass. The patient underwent laparotomy with complete excision of the remaining tumor. At this time, in solid cancer consolidation therapy, the patient receives 5000cGy of radiation to the abdomen and pelvis in 25 fractions. In parallel, she was directed to the bone marrow transplant service for autologous transplant assessment as multiple myeloma consolidation treatment.
DiscussionThe primary multiple malignant neoplasia is a rare clinical condition, characterized by the occurrence of two or more primary concomitant or successive malignancies in the same patient. According to literature data, its incidence is of 0.7–11.7%. This event is established when the diseases have clear malignancy evidence with distinct histological particularities, discarding the possibility of one malignancy being the metastatic manifestation of the other. They are said to be synchronous when the appearance interval between the secondary neoplasia and the primary neoplasia is less than six months; and metachronous, when this time interval is greater than six months. It is known that the synchronous occurrence is rare, and even less usual is the association of solid tumors with hematologic malignancy.1 We describe a patient case with synchronous multiple myeloma and well-differentiated liposarcoma, as in conjunction with the plasma cell illness diagnosis, the patient had an abdominal mass in the right iliac fossa topography, mistakenly evaluated as an extra-medullary myeloma manifestation. The literature reports less than half a dozen cases of synchronous multiple myeloma and solid tumors, such as colorectal cancer, gynecological cancer, and well-differentiated liposarcoma in the mediastinum.4,6,7 However, no conclusion has been reached regarding the pathogenesis of these synchronous cases of multiple myeloma and solid cancer.
The occurrence of primary multiple malignant neoplasia is related to genetic predisposition, familial cancer history, installed immunosuppression condition, unregulated release of cytokines and underlying chronic inflammatory state.1 The evolution of a secondary tumor subsequent to the diagnosis of primary neoplasia is well-attributed to the adopted chemotherapy and radiation treatment, as well as the development of technologies, the employed nuclear image in the last 15 years for the diagnosis, staging and monitoring of primary oncologic disease, these factors being substantially involved in the unfolding of subsequent oncohematologic illnesses.5
Multiple myeloma is a B-cell clonal malignancy in which there is uncontrolled growth in bone marrow plasma cells. This anomalous proliferation causes disturbances in hematopoiesis exteriorized by anemia, renal dysfunction, and bone destruction. It is an incurable disease; the average diagnosis age is 69 years; three-quarters of patients are diagnosed over 55 years of age, and; there is a black, male predominance.8 Recognized as a systemic disease, the excessive clonal multiplication is typically restricted to the bone marrow. However, a minority of patients may manifest the extramedullary disease at diagnosis, or during disease progression or relapse, being the extamedullary plasmocytoma, an abdominal mass often found in the spleen, liver and lymphoid nodules, which differentiates the Hodgkin's lymphoma from the non-Hodgkin's lymphoma. As an extramedullary disease, it compromises the central nervous system, having a 1% incidence among patients with multiple myeloma. In the literature, there are reports of leptomeningeal myelomatosis, characterized by intraductal masses involving the spinal cord and causing nerve root compression.9 Regardless of the clinical expression, these manifestations are associated with cytogenetic aberrations, predictors of a bad prognosis.10 In the case described above, the abdominal mass in the right iliac fossa, which became evident in the ultrasound examination, was understood as an extramedullary manifestation of the underlying disease.
The hematological malignancies associated with solid tumors include multiple myeloma, chronic lymphocytic leukemia, non-Hodgkin's lymphoma and myelodysplastic syndrome, whether it be due to the underlying state of immunosuppression or primary disease therapy. Among the post-secondary solid neoplasms after the myeloma diagnosis are: breast cancer, colorectal cancer, melanoma, genitourinary cancer, prostate cancer and, in a lower frequency, pulmonary neoplasm and sarcoma. Among the associated onco-hematological disorders after the myeloma diagnosis are especially for acute myeloid leukemia, myelodysplastic syndrome, non-Hodgkin's and Hodgkin's lymphoma. It is known that patients with myeloma who have secondary neoplasms have a reserved prognosis.4
The malignant retroperitoneal tumor corresponds to 80% of the primary adult malignant peritoneal neoplasms, but its early diagnosis is incidental, as the patient initially, in the clear majority, is asymptomatic due to the vast available space in the abdominal cavity for the expansion of the tumor, without compromising vital structures. Retroperitoneal sarcoma is a rare condition. Among its manifestations, the liposarcoma is the most common clinical entity, originating from the mesenchymal cell differentiation, and according to its histology type is classified into: well-differentiated, undifferentiated, myxoid and pleomorphic. The first two are more frequent in the retroperitoneum, while the myxomatous and pleomorphic forms have a predilection for the extremities. The contrast CT scan and/or abdomen and pelvis MRI are the instruments that aid in the diagnosis and staging of the disease.3 In the case described, the CT examination raised the diagnosis possibility, confirmed by the result of collected histopathological material in the lesion biopsy, via laparoscopy. The pathogenesis is still uncertain, but the installed immunodeficiency state due to multiple myeloma can play a key role in the synchronous liposarcoma emergence. However, the number of cases in the literature is very low, which hampers the acquisition of knowledge.
ConclusionThe case described represents a rare clinical condition called primary multiple malignant neoplasia, through the synchronous occurrence of multiple myeloma and liposarcoma. The lack of studies on this synchronous association, as well as the few reported cases in the literature, inhibits a greater clarification of the involved pathogenesis. However, future research and development are welcome to the scientific community for elucidation of the peculiarities that involve this presentation.
The therapeutic approach differs between these two malignancies. Thus, recognition of this uncommon occurrence may help in an early and accurate diagnosis and the development of an appropriate treatment, as soon as possible, in a manner that minimizes the possible underlying comorbidities and strengthens a promising prognosis
Conflicts of interestThe authors declare no conflicts of interest.
We thank the oncology unit of São José do Avaí Hospital in Itaperuna.